International Journal of Clinical Anesthesiology
Volume 2 - Issue 4 Articles
-
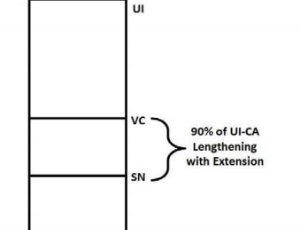
ArticleNovember 03, 2014 | Pages : 205 - 450Abstract The length of the human trachea in both awa-e and anesthetized and paralyzed patients is a critical consideration in preventing both endobronchial intubation and tracheal extubation. It is clear from the literature that with the dynamic clinical chan.....
-
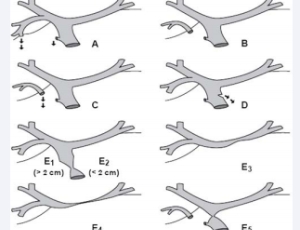
ArticleColin Huntley Eric W. Schaefer Kane High Margaret M. Wojnar Michael Goldenberg Shannon M. Grap Sonia VaidaNovember 03, 2014 | Pages : 205 - 450Abstract Background: Tracheostomy is a common surgical procedure performed in the adult intensive care unit (ICU) population etc. Our objective was to identify characteristics associated with one year mortality in adult ICU patients following tracheostomy pla.....
-
ArticleNovember 03, 2014 | Pages : 205 - 450Abstract Management of sphenoid wing meningioma is a big challenge not only for the neurosurgeon, for the anesthesiologist also. It requires extensive preoperative work up and assesement, on toe intraoperative monitoring with quick response skills and effecti.....
-
ArticleNovember 03, 2014 | Pages : 205 - 450Abstract Sequence variations in the RYR1 gene encoding the skeletal muscle sarcoplasmic reticulum calcium release channel are the cause of malignant hyperthermia susceptibility and of several myopathies. This article reviews the RYR1-related myopathies and th.....
Volume 2 - Issue 3 Articles
-
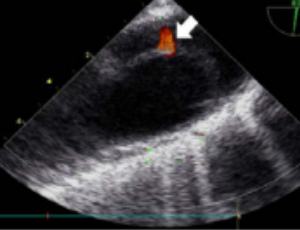
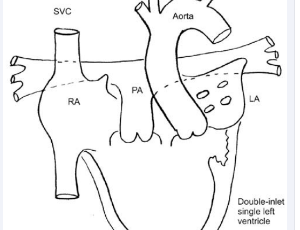
ArticleJune 06, 2014 | Pages : 205 - 450Abstract Intraoperative acute descending aortic dissection is a rare and potentially fatal complication of open cardiac surgery. We report the case of a 62-year-old female who developed this condition during surgery includingmitral valvuloplasty, tricuspid va.....
-
ArticleJuly 06, 2014 | Pages : 205 - 450Abstract Laparoscopic surgery is a very common and widely established technique. Benefits include decreased postoperative pain, improved patient satisfaction (including cosmetic results), reduced hospital stays and fewer postoperative complications compared w.....
-
ArticleJuly 14, 2014 | Pages : 205 - 450Abstract We report the successful management of Total Intravenous Anesthesia (TIVA) for a narcoleptic patient using propofol and remifentanil under Bispectral Index (BIS) monitoring. A 63-year-old woman with narcolepsy required oral surgery under general anes.....
-
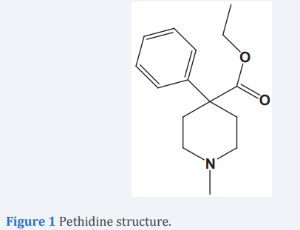
ArticleAbdel Fatah Salem Abu Dayyih W Dania El Tannir Eyad Mallah Mohammad Hamad Nasir Idkaidek Riad Awad Tawfiq ArafatJune 06, 2014 | Pages : 205 - 450Abstract Background: Since 1940, pethidine became the most widely used opioid for labor analgesia. However, pethidine administration may cause fetal distress especially if delivery occurred in a short time after administration and due to genetic variations be.....
Volume 2 - Issue 2 Articles
-
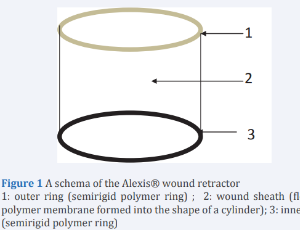
ArticleJune 06, 2014 | Pages : 205 - 450Abstract We present a case of severe hypotension associated with insertion of an Alexis® wound protector/retractor during lower abdominal surgery in a child. A 3-year old female patient underwent ureteroneocystostomy for vesicoureteral reflux under general a.....
-
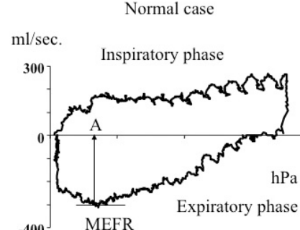
ArticleJune 06, 2014 | Pages : 205 - 450Abstract Background: Recently, the open-lung concept has been used in the respiratory care of patients with Acute Lung Injury (ALI), however, the expiratory phase in ALI patients has not yet been studied in detail. In this study, we paid attention to the pres.....
-
ArticleJune 06, 2014 | Pages : 205 - 450Abstract Introduction: The incidence and risk factors of Postoperative Acute Kidney Injury (PO-AKI) after liver surgery are not well established. The purpose of the present study was to evaluate the incidence and perioperative risk factors of PO-AKI in patien.....
-
ArticleJune 06, 2014 | Pages : 205 - 450Abstract Background: Intra-articular injection of lidocaine is a recognized anesthetic technique for closed reduction of Anterior Internal Shoulder Dislocation (AISD), which may be of particular benefit to patients in developing countries. Methods: A prospe.....

-
ArticleJune 11, 2014 | Pages : 205 - 450Abstract The anaesthetic management of patient with craniofacial pathology often presents unique challenges because soft tissue and bony abnormities can affect the airway and influence airway management. In emergency cases having difficult airway it’s alway.....

-
ArticleJune 16, 2014 | Pages : 205 - 450Abstract Sivelestat is a potent inhibitor of neutrophil elastase activity. We report a patient who suddenly developed hypoxia during surgery, which improved by the administration of sivelestat. A 72-year-old woman underwent emergency resection of a perforated.....
Volume 2 - Issue 1 Articles
-
ArticleJanuary 21, 2014 | Pages : 205 - 450
-
ArticleJanuary 13, 2014 | Pages : 205 - 450Abstract Venous-venous extracorporeal membrane oxygenation [ECMO] can be life saving in clinical situations where awake, fiberoptic intubation or tracheostomy were indicated but were not feasible because of critical airway obstruction in the lower airways. We.....
-
ArticleJanuary 12, 2014 | Pages : 205 - 450Abstract Restrictive familial cardiomyopathy (RCM) is a rare cardiac disease which imposes serious risks on the parturient, especially during labor and delivery. I describe a case of a patient with severe RCM who successfully underwent emergency cesarean sect.....
-
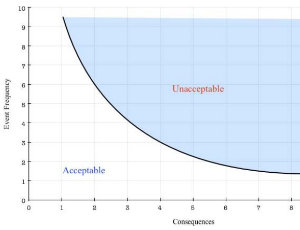
ArticleJanuary 15, 2014 | Pages : 205 - 450Abstract This article discusses risk and uncertainty of general anesthesia, taking into account consideration of unknown and random variables and probabilities as well as the acknowledgment of known and possibly controlled variables as it applies to anesthesi.....
-
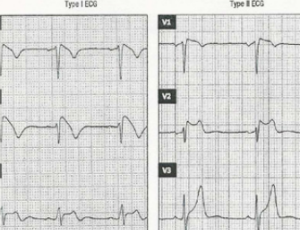
ArticleJanuary 10, 2014 | Pages : 205 - 450Abstract Brugada syndrome (BS) is a rare cardiac channelopathy that was first described in 1992. It accounts for four percent of all sudden deaths and up to twenty percent of sudden deaths in patients without structural cardiac defects. Since known and unknow.....
-
ArticleS Mangione Alessandra Casuccio BS Benedetto Santostefano Cristina Agozzino Dario D’ Anna Mario Mazzara Rosalia D’ Angelo Rosanna Bellingardo Sebastiano MercadanteJanuary 07, 2014 | Pages : 205 - 450Abstract The aim of this study was to assess the characteristics of patients admitted to a recovery room [RR] in an oncological department. The secondary outcomes were to evaluate how RR was able to prevent immediate postoperative complications and which are .....
Browse by Year
Author Information
X
Subscribe to Newsletters
And stay informed about our news and events