International Journal of Clinical Anesthesiology
Volume 3 - Issue 2 Articles
-
ArticleDecember 16, 2015 | Pages : 205 - 450Abstract During pregnancy % 0.75-2 of patients need surgery and anesthesia. Ovarian torsion which requires emergency surgery is one of them. When surgery is needed during pregnancy period, anesthetic management should be planned to protect both mother and fet.....
-
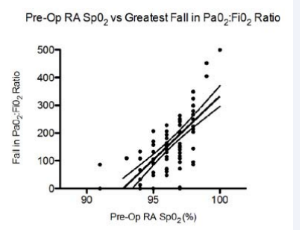
ArticleSeptember 14, 2015 | Pages : 205 - 450Abstract Aim: Pain following shoulder surgery can be severe; interscalene brachial plexus blockade (ISB) and high dose opioid analgesia are commonly used management options, however both impair oxygenation by multiple mechanisms. We aimed to quantify the ex.....
-
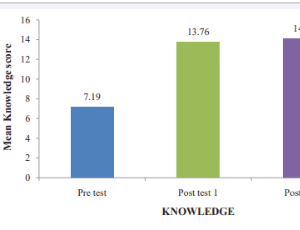
ArticleAugust 31, 2015 | Pages : 205 - 450Abstract Cardiac or respiratory arrests are common emergencies in adults, children and neonatal period. Resuscitation is the art of restoring life or consciousness of one apparently dead. The main aim of the study was to assess and compare knowledge and pract.....
Volume 3 - Issue 1 Articles
-
ArticleAbolfazl Firouzian Mehran Fazli Mohammad Sadegh Zamani-Ranani Najme Galyan Moghaddam Seyyed Abbas HashemiJanuary 05, 2015 | Pages : 205 - 450Abstract Background: Inguinal hernia repair is one of the most common surgeries and can be performed under general, spinal or local anesthesia. The aim of this study was to compare the complications of local anesthesia (LA) with spinal anesthesia (SA) in surg.....
-
ArticleJuly 20, 2015 | Pages : 205 - 450Abstract Intravenous dexmedetomidine is been increasingly used in perioperative setting including as an adjunct to local anaesthetic in various regional techniques with an intent to either improve the block quality, increase the duration of block or to provid.....
-
ArticleJuly 20, 2015 | Pages : 205 - 450Abstract Acute radial nerve paralysis developed following general anaesthesia for tympanoplasty surgery in a 22-year old male with a 4-year history of manual work. Standard pads were used under the extremities and the patient position was changed at intervals.....
-
ArticleJuly 13, 2015 | Pages : 205 - 450Abstract The number of patients receiving organ transplants is increasing around the world. So, anesthesiologists are often have to manage transplant recipients in hospitals for procedures that are not related to transplantation. There are many possible probl.....
-
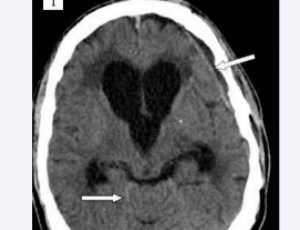
ArticleMay 02, 2015 | Pages : 205 - 450Abstract The underlying pathophysiology in low-pressure hydrocephalus (LPH) includes brain viscoelastic properties, brain turgor, transmantle pressure gradient and cerebrospinal fluid leaks. LPH consists of ventriculomegaly with low or negative intracranial p.....
Browse by Year
Author Information
X
Subscribe to Newsletters
And stay informed about our news and events