2022 Volume 7 - Issue 1
-
October 23, 2022 Short Communication
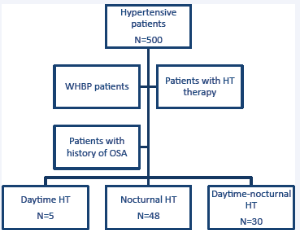 Abstract Introduction: Guidelines suggest suspecting obstructive apnea-hypopnea syndrome (OSA) in patients with hypertension (HT) if the nocturnal blood pressure is elevated, a patient is a non-dipper or an inverse pressure pattern is observed. The objective .....
Abstract Introduction: Guidelines suggest suspecting obstructive apnea-hypopnea syndrome (OSA) in patients with hypertension (HT) if the nocturnal blood pressure is elevated, a patient is a non-dipper or an inverse pressure pattern is observed. The objective .....