2022 Volume 9 - Issue 1
-
February 14, 2022 Review Article
 Abstract Background: Beta - Thalassemia is the most common hemoglobinopathy throughout the world. Beta globin chain synthesis is completely or partially compromised in the affected individuals. This leads to transfusion dependency in majority of patients. How.....
Abstract Background: Beta - Thalassemia is the most common hemoglobinopathy throughout the world. Beta globin chain synthesis is completely or partially compromised in the affected individuals. This leads to transfusion dependency in majority of patients. How..... -
March 21, 2023 Review Article
 Abstract Human parvo virus B19 (B19V) is a small single stranded DNA virus with known tropism and cytotoxicity for erythroid progenitors. Its infection is associated with various hematological disorders like aplastic crisis, erythroid hypoplasia, idiopathic t.....
Abstract Human parvo virus B19 (B19V) is a small single stranded DNA virus with known tropism and cytotoxicity for erythroid progenitors. Its infection is associated with various hematological disorders like aplastic crisis, erythroid hypoplasia, idiopathic t..... -
August 02, 2022 Research Article
 Abstract Background: Blood donations are generally well tolerated but they are not completely without risk. Adverse reactions are complications of blood donations with significant donor discomfort and negative effect on donor satisfaction and return for donat.....
Abstract Background: Blood donations are generally well tolerated but they are not completely without risk. Adverse reactions are complications of blood donations with significant donor discomfort and negative effect on donor satisfaction and return for donat..... -
December 15, 2022 Case Report
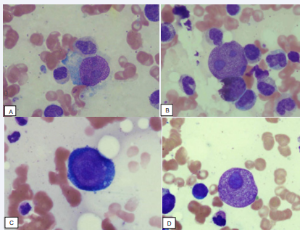
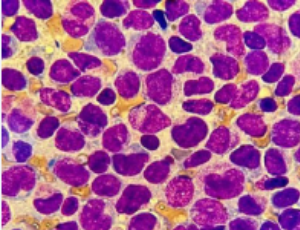 Abstract Acute Promyelocytic Leukemia (APL) is characterized by the PML-RARA fusion gene, as a consequence of the t (15;17(q22;q21) translocation. Depending on the PML breakpoint, usually located within intron6, exon6, or intron 3, different PML/RARA transc.....
Abstract Acute Promyelocytic Leukemia (APL) is characterized by the PML-RARA fusion gene, as a consequence of the t (15;17(q22;q21) translocation. Depending on the PML breakpoint, usually located within intron6, exon6, or intron 3, different PML/RARA transc..... -
December 16, 2022 Research Article
 Abstract Introduction: Human immunodeficiency virus (HIV) can be transmitted through blood transfusion. It is therefore important to screen all blood donors properly for HIV in order to ensure the safety of all blood products that will be transfused into reci.....
Abstract Introduction: Human immunodeficiency virus (HIV) can be transmitted through blood transfusion. It is therefore important to screen all blood donors properly for HIV in order to ensure the safety of all blood products that will be transfused into reci.....