2022 Volume 8 - Issue 1
-
March 07, 2022 Research Article
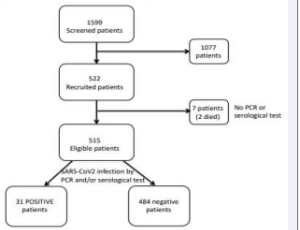 Abstract Background: Cancer patients are highly vulnerable to SARS-CoV-2 infection and the risk-benefit of active cancer treatment should be evaluated if infection occurs. Thus, it was of interest to assess the SARS-CoV2 infection prevalence among cancer outp.....
Abstract Background: Cancer patients are highly vulnerable to SARS-CoV-2 infection and the risk-benefit of active cancer treatment should be evaluated if infection occurs. Thus, it was of interest to assess the SARS-CoV2 infection prevalence among cancer outp..... -
May 28, 2022 Opinion Article
 Abstract Pneumonia (AP) has been known to medicine throughout its foreseeable history as a severe inflammatory disease that does not pose a danger to others in contact with the patient.
Abstract Pneumonia (AP) has been known to medicine throughout its foreseeable history as a severe inflammatory disease that does not pose a danger to others in contact with the patient. -
June 18, 2022 Research Article
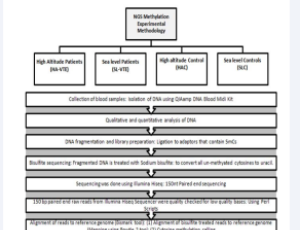 Abstract Background: Pathophysiology of venous thrombo-embolism (VTE) depends upon several acquired, inherited and environmental risk factors, including high altitude (HA) exposure. The present study aims to gain insights into pathophysiological mechanism(s) .....
Abstract Background: Pathophysiology of venous thrombo-embolism (VTE) depends upon several acquired, inherited and environmental risk factors, including high altitude (HA) exposure. The present study aims to gain insights into pathophysiological mechanism(s) ..... -
December 26, 2022 Case Report
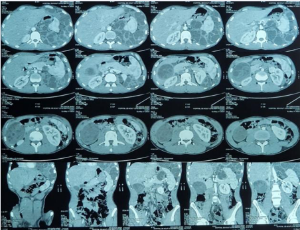 Abstract Background: Hydatidosis is a parasitic infection that is still frequent in the world, especially in the Mediterranean area and in breeding regions such as Morocco. The management of complicated hydatid cysts remains delicate, especially in the case o.....
Abstract Background: Hydatidosis is a parasitic infection that is still frequent in the world, especially in the Mediterranean area and in breeding regions such as Morocco. The management of complicated hydatid cysts remains delicate, especially in the case o.....