Recent Articles
-
March 30, 2024 Case Report
 Abstract Metastases from follicular thyroid carcinomas are rare. Thoracic metastases mainly involve the lungs, mediastinal lymph nodes and pleura. We report a case showing the natural course of follicular thyroid cancer in a female patient aged 66, exposed to.....
Abstract Metastases from follicular thyroid carcinomas are rare. Thoracic metastases mainly involve the lungs, mediastinal lymph nodes and pleura. We report a case showing the natural course of follicular thyroid cancer in a female patient aged 66, exposed to..... -
March 05, 2024 Short Communication
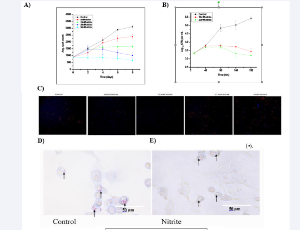 Abstract Tuberculosis is one of the top ten causes of human death. The generation of reactive nitrogen intermediates within the macrophages and to some extent in Mycobacterium tuberculosis cells as well is well documented. Release of NO from lung macrophage c.....
Abstract Tuberculosis is one of the top ten causes of human death. The generation of reactive nitrogen intermediates within the macrophages and to some extent in Mycobacterium tuberculosis cells as well is well documented. Release of NO from lung macrophage c..... -
November 14, 2023 Case Report
-
September 25, 2023 Short Communication
 Abstract High-altitude Illnesses (HAI) in the climbing population on Mount Kilimanjaro form a small but steady patient population in our tertiary referral centre. The aim of this study was to document neurological disorders in climbers independent of HAI. Met.....
Abstract High-altitude Illnesses (HAI) in the climbing population on Mount Kilimanjaro form a small but steady patient population in our tertiary referral centre. The aim of this study was to document neurological disorders in climbers independent of HAI. Met..... -
September 12, 2023 Case Report
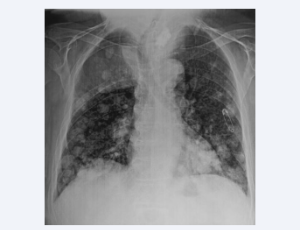
 Abstract Microscopic polyangiitis is a rare systemic necrotizing vasculitis of unknown origin that affects small-caliber vessels. We report the case of a 42 years old némale patient who presented for 4 months several episodes of gradual onset, medium-abundan.....
Abstract Microscopic polyangiitis is a rare systemic necrotizing vasculitis of unknown origin that affects small-caliber vessels. We report the case of a 42 years old némale patient who presented for 4 months several episodes of gradual onset, medium-abundan..... -
August 19, 2023 Research Article
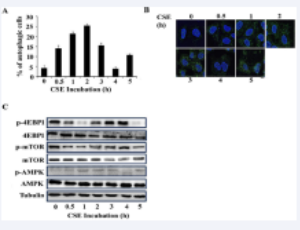 Abstract Cigarette smoke-induced protein accumulation and aggresome formation is a major pathological hallmark of COPD disease. Aggresome formation results from a defect in autophagy. To understand the mechanism of cigarette smoke-induced autophagy defect, th.....
Abstract Cigarette smoke-induced protein accumulation and aggresome formation is a major pathological hallmark of COPD disease. Aggresome formation results from a defect in autophagy. To understand the mechanism of cigarette smoke-induced autophagy defect, th..... -
July 10, 2023 Case Report
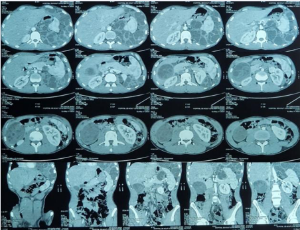
 Abstract Abstract Hydatidosis is an anthropozoonosis caused by the development of cysts corresponding to the larval form of a taenia called Ecchinococcus granulosis. Bone hydatidosis is rare, accounting for only 0.9% to 2.5% of all cases. We report the case o.....
Abstract Abstract Hydatidosis is an anthropozoonosis caused by the development of cysts corresponding to the larval form of a taenia called Ecchinococcus granulosis. Bone hydatidosis is rare, accounting for only 0.9% to 2.5% of all cases. We report the case o..... -
June 28, 2023 Research Article
 Abstract Objective: The detection of smear-positive and culture-negative (SPCN) status during pulmonary tuberculosis treatment can be seen at a constant rate. However, its risk factors and duration of detection have not been well evaluated with short-interval.....
Abstract Objective: The detection of smear-positive and culture-negative (SPCN) status during pulmonary tuberculosis treatment can be seen at a constant rate. However, its risk factors and duration of detection have not been well evaluated with short-interval..... -
May 08, 2023 Case Report
 Abstract Takayasu’s vasculitis is a rare chronic inflammatory arteritis of unknown origin affecting large arteries in young subjects. We report the observation of a 32-year-old female patient who presented for 6 months with dyspnea stage II mMRC associated .....
Abstract Takayasu’s vasculitis is a rare chronic inflammatory arteritis of unknown origin affecting large arteries in young subjects. We report the observation of a 32-year-old female patient who presented for 6 months with dyspnea stage II mMRC associated ..... -
March 19, 2023 Case Report
 Abstract Miss H.N., aged 39, has no toxic habits. She has been followed up since childhood for tuberous sclerosis of Bourneville (TBS), which was retained in view of the skin involvement. She reported chronic dyspnoea for about ten years. She was hospitalized.....
Abstract Miss H.N., aged 39, has no toxic habits. She has been followed up since childhood for tuberous sclerosis of Bourneville (TBS), which was retained in view of the skin involvement. She reported chronic dyspnoea for about ten years. She was hospitalized..... -
February 13, 2023 Case Report
 Abstract Rasmussen’s aneurysm is a false inflammatory aneurysm of a branch of the pulmonary artery within or adjacent to a tuberculous cavern or other excavated lung lesion, whose rupture may lead to massive hemoptysis. Our patient, who was at 35 days of a.....
Abstract Rasmussen’s aneurysm is a false inflammatory aneurysm of a branch of the pulmonary artery within or adjacent to a tuberculous cavern or other excavated lung lesion, whose rupture may lead to massive hemoptysis. Our patient, who was at 35 days of a..... -
January 13, 2023 Research Article
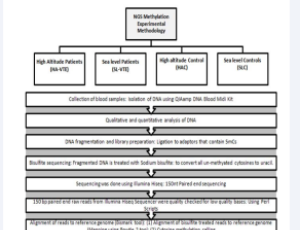
 Abstract COPD is the third leading cause of death worldwide and has a particular impact on the population of India. About 53 million people are affected by COPD in India, and this disease disproportionately affects those in the low-middle income class. This r.....
Abstract COPD is the third leading cause of death worldwide and has a particular impact on the population of India. About 53 million people are affected by COPD in India, and this disease disproportionately affects those in the low-middle income class. This r..... -
October 14, 2015 Review Article
 Abstract Sleep related breathing disorders (SRBD) are common in critically ill as well as in postoperative patients. Because of anatomical reasons the risk of difficulties of endotracheal intubation is increased in these patients. Furthermore, awareness of SR.....
Abstract Sleep related breathing disorders (SRBD) are common in critically ill as well as in postoperative patients. Because of anatomical reasons the risk of difficulties of endotracheal intubation is increased in these patients. Furthermore, awareness of SR..... -
October 07, 2015 Review Article
 Abstract Pulmonary hypertension is a major reason for elevated perioperative morbidity and mortality, even in non-cardiac surgical procedures. Patients more often experience serious complications, such as right-ventricular failure, arrhythmias, and early post.....
Abstract Pulmonary hypertension is a major reason for elevated perioperative morbidity and mortality, even in non-cardiac surgical procedures. Patients more often experience serious complications, such as right-ventricular failure, arrhythmias, and early post..... -
October 01, 2015 Short Communication
 Abstract Introduction: Sleep disorders affect 10-15% of the US population, which has significant implications for quality of life. Oncology patients often experience more prominent detrimental effects of sleep deprivation. Fatigue is one of the most debilitat.....
Abstract Introduction: Sleep disorders affect 10-15% of the US population, which has significant implications for quality of life. Oncology patients often experience more prominent detrimental effects of sleep deprivation. Fatigue is one of the most debilitat..... -
October 16, 2014 Research Article
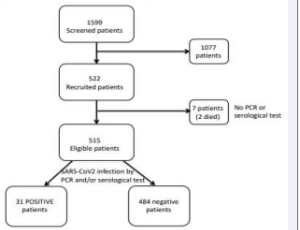
 Abstract Background: Companion animals may have a positive impact on physical activities and on quality of life (QoL) in individuals. However, many lung transplant (LTx) patients are advised against them due to the risk of zoonotic infections. Methods: A .....
Abstract Background: Companion animals may have a positive impact on physical activities and on quality of life (QoL) in individuals. However, many lung transplant (LTx) patients are advised against them due to the risk of zoonotic infections. Methods: A ..... -
October 30, 2014 Case Series
 Abstract Obstructive sleep apnea (OSA) is a common sleep disorder the American Academy of sleep medicine note that it effective 2% to 4% of the adult population. This article follows two patients with sleep apnea and who are experiencing cardiac and pulmonary.....
Abstract Obstructive sleep apnea (OSA) is a common sleep disorder the American Academy of sleep medicine note that it effective 2% to 4% of the adult population. This article follows two patients with sleep apnea and who are experiencing cardiac and pulmonary..... -
September 30, 2020 Research Article
 Abstract Background and significance: It is estimated that 4800 children living in the USA are currently supported by mechanical ventilation at home. Despite advances in technology, the mortality rate of 21% remains high. Previous studies identified knowled.....
Abstract Background and significance: It is estimated that 4800 children living in the USA are currently supported by mechanical ventilation at home. Despite advances in technology, the mortality rate of 21% remains high. Previous studies identified knowled..... -
January 29, 2018 Research Article
 Abstract Rationale: Atrial Fibrillation (AF) is a potent risk factor for ischemic cerebrovascular Accident (ICVA). Inflammation is potential pathogenic factor for atherosclerosis and ICVA. Chronic Obstructive pulmonary disease (COPD) is associated with increa.....
Abstract Rationale: Atrial Fibrillation (AF) is a potent risk factor for ischemic cerebrovascular Accident (ICVA). Inflammation is potential pathogenic factor for atherosclerosis and ICVA. Chronic Obstructive pulmonary disease (COPD) is associated with increa..... -
October 12, 2017 Research Article
 Abstract In our previous study we showed that in normal areas of usual interstitial pneumonia (UIP), type II alveolar epithelial cells telomerase positive (AEC2T+) expression was significantly inferior when compared to normal lung tissue (NLT). Nevertheless.....
Abstract In our previous study we showed that in normal areas of usual interstitial pneumonia (UIP), type II alveolar epithelial cells telomerase positive (AEC2T+) expression was significantly inferior when compared to normal lung tissue (NLT). Nevertheless..... -
June 28, 2017 Perspective
 Abstract Acute respiratory distress syndrome is a syndrome of acute onset characterized by hypoxemia and infiltrates on chest radiographs that affects both adults and children of all ages. It is an important cause of respiratory failure in pediatric intensive.....
Abstract Acute respiratory distress syndrome is a syndrome of acute onset characterized by hypoxemia and infiltrates on chest radiographs that affects both adults and children of all ages. It is an important cause of respiratory failure in pediatric intensive..... -
June 28, 2017 Review Article
 Abstract The objective of this study was to review the last 16 years of literature on the clinical and functional risk factors for asthma exacerbation, as well as on biochemical parameters in severe pediatric asthma refractory to treatment (SPART). In searche.....
Abstract The objective of this study was to review the last 16 years of literature on the clinical and functional risk factors for asthma exacerbation, as well as on biochemical parameters in severe pediatric asthma refractory to treatment (SPART). In searche..... -
May 25, 2017 Case Report
 Abstract Sarcoidosis is a chronic granulomatous inflammatory disease of unknown etiology. It affects predominantly lungs, thoracic lymph nodes, skin and eyes. Thyroid gland, skull and vertebrae are rarely involved. The diagnosis is suggested on the basis of c.....
Abstract Sarcoidosis is a chronic granulomatous inflammatory disease of unknown etiology. It affects predominantly lungs, thoracic lymph nodes, skin and eyes. Thyroid gland, skull and vertebrae are rarely involved. The diagnosis is suggested on the basis of c..... -
May 24, 2017 Review Article
 Abstract Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines COPD as a progressive disease with persistent airflow limitation, associated with an enhanced chronic inflammatory response in the airways and the lung to the noxious particles or .....
Abstract Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines COPD as a progressive disease with persistent airflow limitation, associated with an enhanced chronic inflammatory response in the airways and the lung to the noxious particles or ..... -
May 18, 2017 Short Note
-
May 09, 2017 Research Article
 Abstract Background: Idiopathic Pulmonary Fibrosis (IPF) is a fatal lung disease of unknown etiology, where different pathogenetic hypotheses have been suggested. Notwithstanding the unrecognized first trigger that leads to the disease, an imbalance between o.....
Abstract Background: Idiopathic Pulmonary Fibrosis (IPF) is a fatal lung disease of unknown etiology, where different pathogenetic hypotheses have been suggested. Notwithstanding the unrecognized first trigger that leads to the disease, an imbalance between o..... -
October 01, 2016 Review Article
 Abstract Much research has been done to explain the mechanism behind the third most common cause of Cystic Fibrosis (CF), a missense mutation in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) protein. The G551D mutation is caused by a glycine .....
Abstract Much research has been done to explain the mechanism behind the third most common cause of Cystic Fibrosis (CF), a missense mutation in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) protein. The G551D mutation is caused by a glycine ..... -
October 01, 2016 Case Report
 Abstract Hematothorax is a rare but potential life-threatening complication following thoracocentesis, which is most commonly due to intercostal artery laceration during the insertion of the needle. We report a case of a pleural catheter insertion into an.....
Abstract Hematothorax is a rare but potential life-threatening complication following thoracocentesis, which is most commonly due to intercostal artery laceration during the insertion of the needle. We report a case of a pleural catheter insertion into an..... -
May 23, 2016 Review Article
 Abstract The underwater environment is characterized by an increase of the hydrostatic pressure surrounding the body who is immersed. Each 10 meters under the sea-surface the hydrostatic pressure increases by one atmosphere. It turns that this increase can el.....
Abstract The underwater environment is characterized by an increase of the hydrostatic pressure surrounding the body who is immersed. Each 10 meters under the sea-surface the hydrostatic pressure increases by one atmosphere. It turns that this increase can el..... -
October 30, 2015 Review Article
 Abstract Non-communicable diseases (NCDs) will increase over the next decades. Understanding the complexity of chronic NCDs and the adaptation of the health care system to implement new management strategies addressing the patients’ needs, are still major c.....
Abstract Non-communicable diseases (NCDs) will increase over the next decades. Understanding the complexity of chronic NCDs and the adaptation of the health care system to implement new management strategies addressing the patients’ needs, are still major c..... -
October 23, 2015 Review Article
 Abstract Cardiopulmonary bypass (CPB) during open-heart surgery is associated with pulmonary complications, such as atelectasis, acute respiratory distress syndrome (ARDS), pulmonary vascular injury and respiratory failure. Many patients require prolonged mec.....
Abstract Cardiopulmonary bypass (CPB) during open-heart surgery is associated with pulmonary complications, such as atelectasis, acute respiratory distress syndrome (ARDS), pulmonary vascular injury and respiratory failure. Many patients require prolonged mec..... -
June 16, 2015 Mini Review
 Abstract Pulmonary complications are a major concern after hematopoietic stem cell transplantation and are an important cause of morbidity and mortality. This pictorial essay reviews and illustrates the CT imaging findings of pulmonary complications after HSC.....
Abstract Pulmonary complications are a major concern after hematopoietic stem cell transplantation and are an important cause of morbidity and mortality. This pictorial essay reviews and illustrates the CT imaging findings of pulmonary complications after HSC..... -
April 04, 2015 Research Article
 Abstract Objective: To evaluate the effect of menarche before 11 years of age on the incidence of wheezing/asthma in girls 11 to 18 years of age. Methods: The study sample comprised 1,350 girls from a birth cohort that started in 1993 in the urban area of .....
Abstract Objective: To evaluate the effect of menarche before 11 years of age on the incidence of wheezing/asthma in girls 11 to 18 years of age. Methods: The study sample comprised 1,350 girls from a birth cohort that started in 1993 in the urban area of ..... -
February 10, 2015 Review Article
 Abstract The causes for the death of cancer patients’ deaths can be multi-factorials and pathogenesis progresses in clinics. Apart from direct causes from tumor progressions and metastases by genetic inheritance, mutations, deletions, repeating and other ty.....
Abstract The causes for the death of cancer patients’ deaths can be multi-factorials and pathogenesis progresses in clinics. Apart from direct causes from tumor progressions and metastases by genetic inheritance, mutations, deletions, repeating and other ty..... -
February 10, 2015 Review Article
 Abstract Primary graft dysfunction (PGD) is a common early complication after lung transplantation and represents an acute lung injury with clinical, radiographic, and histological features similar to acute respiratory distress syndrome (ARDS). PGD is associa.....
Abstract Primary graft dysfunction (PGD) is a common early complication after lung transplantation and represents an acute lung injury with clinical, radiographic, and histological features similar to acute respiratory distress syndrome (ARDS). PGD is associa..... -
December 21, 2014 Case Report
 Abstract The Bronchus Associated Lymphoid Tissue Lymphoma invades the bronchial epithelial tissue and is histologically characterized by a lympho epithelial small cell infiltrate. We present a case of a Bronchus Associated Lymphoid Tissue (BALT) Lymphoma, rad.....
Abstract The Bronchus Associated Lymphoid Tissue Lymphoma invades the bronchial epithelial tissue and is histologically characterized by a lympho epithelial small cell infiltrate. We present a case of a Bronchus Associated Lymphoid Tissue (BALT) Lymphoma, rad..... -
December 10, 2014 Research Article
 Abstract Background: Flying disc (FD) game might improve the physical activity (PA) in patients with long-term oxygen therapy (LTOT). However, the objectively-measured intensity and the safety of FD game have not been evaluated. In order to apply the FD game .....
Abstract Background: Flying disc (FD) game might improve the physical activity (PA) in patients with long-term oxygen therapy (LTOT). However, the objectively-measured intensity and the safety of FD game have not been evaluated. In order to apply the FD game ..... -
October 13, 2014 Review Article
 Abstract Pulmonary arterial hypertension (PAH) is a rare condition characterized by small pulmonary artery remodeling that leads to chronic precapillary pulmonary hypertension, elevated pulmonary vascular resistance, and right heart failure. Therapeutic optio.....
Abstract Pulmonary arterial hypertension (PAH) is a rare condition characterized by small pulmonary artery remodeling that leads to chronic precapillary pulmonary hypertension, elevated pulmonary vascular resistance, and right heart failure. Therapeutic optio..... -
October 13, 2014 Research Article
 Abstract Background: The WHO has identified ambient air pollution as a high public health priority. The community health research programs that were performed by Tikrit University College of Medicine have estimated that more than a fourth of Iraqi populations.....
Abstract Background: The WHO has identified ambient air pollution as a high public health priority. The community health research programs that were performed by Tikrit University College of Medicine have estimated that more than a fourth of Iraqi populations..... -
October 16, 2014 Short Communication
 Abstract Mucociliary transport in the nose serves as the first host defense against the inhalation of atmospheric particulate matter. Nasal Mucociliary Clearance (NMC) is determined to obtain an in vivo measurement of the effectiveness of the interaction betw.....
Abstract Mucociliary transport in the nose serves as the first host defense against the inhalation of atmospheric particulate matter. Nasal Mucociliary Clearance (NMC) is determined to obtain an in vivo measurement of the effectiveness of the interaction betw..... -
October 10, 2014 Review Article
 Abstract Despite adequate adherence and completion of anti-asthmatic treatment, many patients remain poorly controlled or uncontrolled. Asthma management is based on the use of medication to reverse the bronchial obstruction and eliminate the airway inflammat.....
Abstract Despite adequate adherence and completion of anti-asthmatic treatment, many patients remain poorly controlled or uncontrolled. Asthma management is based on the use of medication to reverse the bronchial obstruction and eliminate the airway inflammat..... -
April 29, 2014 Review Article
 Abstract n the present study, a review of the literature that examines the widely used clinical applications of Forced Oscillation Technique (FOT) and Impulse Oscillometry (IOS) is attempted, in order to evaluate the contribution of the method to laboratory l.....
Abstract n the present study, a review of the literature that examines the widely used clinical applications of Forced Oscillation Technique (FOT) and Impulse Oscillometry (IOS) is attempted, in order to evaluate the contribution of the method to laboratory l..... -
April 29, 2014 Case Report
 Abstract Background: Electromagnetic Navigation Bronchoscopy (ENB) is generally implemented as a diagnostic tool in the investigation of suspicious pulmonary nodules. The use of this technique to mark pulmonary nodules (using dye) prior to surgical resection .....
Abstract Background: Electromagnetic Navigation Bronchoscopy (ENB) is generally implemented as a diagnostic tool in the investigation of suspicious pulmonary nodules. The use of this technique to mark pulmonary nodules (using dye) prior to surgical resection ..... -
May 07, 2014 Review Article
 Abstract Chronic Lung Allograft Dysfunction (CLAD) or chronic rejection after lung transplantation may exhibit a conventional obstructive form (bronchiolitis obliterans syndrome, BOS) or a restrictive form with predominant involvement of peripheral lung tissu.....
Abstract Chronic Lung Allograft Dysfunction (CLAD) or chronic rejection after lung transplantation may exhibit a conventional obstructive form (bronchiolitis obliterans syndrome, BOS) or a restrictive form with predominant involvement of peripheral lung tissu..... -
May 23, 2014 Review Article
 Abstract Chronic obstructive pulmonary disease is defined as a situation of progressive airflow limitation, sometimes reversible, whose pathogenetic mechanisms responsible are to be attributed, on the one hand, to the progressive obstruction of the central an.....
Abstract Chronic obstructive pulmonary disease is defined as a situation of progressive airflow limitation, sometimes reversible, whose pathogenetic mechanisms responsible are to be attributed, on the one hand, to the progressive obstruction of the central an..... -
January 27, 2014 Short Communication
 Abstract Nutritional depletion is known to be a determinant of outcome in chronic respiratory disease but there is a paucity of evidence on nutritional intervention in bronchiectasis. The aim of this study was to retrospectively review body mass index (BMI).....
Abstract Nutritional depletion is known to be a determinant of outcome in chronic respiratory disease but there is a paucity of evidence on nutritional intervention in bronchiectasis. The aim of this study was to retrospectively review body mass index (BMI)..... -
August 02, 2013 Review Article

-
August 02, 2013 Review ArticleRespiratory and Sleep Disorders in Chronic Neuromuscular Disease, an Update and Therapeutic Approach
 Abstract Respiratory and sleep disorders are common in patients with neuromuscular disease but under recognized especially during sleep or when patients are asymptomatic. In the last decades there has been great interest in understanding the mechanism of dise.....
Abstract Respiratory and sleep disorders are common in patients with neuromuscular disease but under recognized especially during sleep or when patients are asymptomatic. In the last decades there has been great interest in understanding the mechanism of dise..... -
August 02, 2013 Editorial
 Abstract Numerous lung diseases have high morbidity and mortality rates and there are no cures or treatments apart from lung transplantation. In United States, respiratory diseases kill more than 400,000 individuals each year and significantly reduce qual.....
Abstract Numerous lung diseases have high morbidity and mortality rates and there are no cures or treatments apart from lung transplantation. In United States, respiratory diseases kill more than 400,000 individuals each year and significantly reduce qual..... -
August 02, 2013 Editorial
-
August 03, 2013 Review Article
 Abstract Acute lung injury (ALI) and its more severe form, acute respiratory distress syndrome (ARDS), have high mortality rates with few treatment options. A crucial factor in the pathology observed in ALI/ARDS is a disruption of the pulmonary endothelial b.....
Abstract Acute lung injury (ALI) and its more severe form, acute respiratory distress syndrome (ARDS), have high mortality rates with few treatment options. A crucial factor in the pathology observed in ALI/ARDS is a disruption of the pulmonary endothelial b..... -
August 02, 2013 Research Article
 Abstract Background: Following curative surgery for non-small cell lung carcinoma (NSCLC), patients remain at risk for recurrence or for development of second primary lung cancer (SPLC). While regular surveillance imaging may detect early stage recurrence or .....
Abstract Background: Following curative surgery for non-small cell lung carcinoma (NSCLC), patients remain at risk for recurrence or for development of second primary lung cancer (SPLC). While regular surveillance imaging may detect early stage recurrence or ..... -
October 07, 2015 Review Article
 Abstract Pulmonary hypertension is a major reason for elevated perioperative morbidity and mortality, even in non-cardiac surgical procedures. Patients more often experience serious complications, such as right-ventricular failure, arrhythmias, and early post.....
Abstract Pulmonary hypertension is a major reason for elevated perioperative morbidity and mortality, even in non-cardiac surgical procedures. Patients more often experience serious complications, such as right-ventricular failure, arrhythmias, and early post..... -
October 16, 2014 Research Article
 Abstract Background: Companion animals may have a positive impact on physical activities and on quality of life (QoL) in individuals. However, many lung transplant (LTx) patients are advised against them due to the risk of zoonotic infections. Methods: A si.....
Abstract Background: Companion animals may have a positive impact on physical activities and on quality of life (QoL) in individuals. However, many lung transplant (LTx) patients are advised against them due to the risk of zoonotic infections. Methods: A si..... -
October 14, 2015 Review Article
 Abstract Sleep related breathing disorders (SRBD) are common in critically ill as well as in postoperative patients. Because of anatomical reasons the risk of difficulties of endotracheal intubation is increased in these patients. Furthermore, awareness of SR.....
Abstract Sleep related breathing disorders (SRBD) are common in critically ill as well as in postoperative patients. Because of anatomical reasons the risk of difficulties of endotracheal intubation is increased in these patients. Furthermore, awareness of SR..... -
October 01, 2015 Review Article
 Abstract Introduction: Sleep disorders affect 10-15% of the US population, which has significant implications for quality of life. Oncology patients often experience more prominent detrimental effects of sleep deprivation. Fatigue is one of the most debilitat.....
Abstract Introduction: Sleep disorders affect 10-15% of the US population, which has significant implications for quality of life. Oncology patients often experience more prominent detrimental effects of sleep deprivation. Fatigue is one of the most debilitat..... -
June 30, 2014 Case Series
 Abstract Obstructive sleep apnea (OSA) is a common sleep disorder the American Academy of sleep medicine note that it effective 2% to 4% of the adult population. This article follows two patients with sleep apnea and who are experiencing cardiac and pulmonary.....
Abstract Obstructive sleep apnea (OSA) is a common sleep disorder the American Academy of sleep medicine note that it effective 2% to 4% of the adult population. This article follows two patients with sleep apnea and who are experiencing cardiac and pulmonary..... -
October 10, 2014 Research Article
 Abstract Background and Objectives: Quantitative loop-mediated isothermal amplification (qLAMP) has been considered an efficient approach for validating infectious pathogens. We assessed that the qLAMP could be served as a great implement for steering of the .....
Abstract Background and Objectives: Quantitative loop-mediated isothermal amplification (qLAMP) has been considered an efficient approach for validating infectious pathogens. We assessed that the qLAMP could be served as a great implement for steering of the ..... -
April 13, 2014 Research Article
 Abstract Purpose: The relevance of Time to Disappearance (Td) of Tuberculosis (TB) bacilli from sputa in response to anti-TB therapy and clinical parameters were investigated to determine clinical factors that predict response to anti-TB therapy. Method: A .....
Abstract Purpose: The relevance of Time to Disappearance (Td) of Tuberculosis (TB) bacilli from sputa in response to anti-TB therapy and clinical parameters were investigated to determine clinical factors that predict response to anti-TB therapy. Method: A ..... -
August 02, 2013 Review Article