2022 Volume 10 - Issue 1
-
June 18, 2022 Research Article
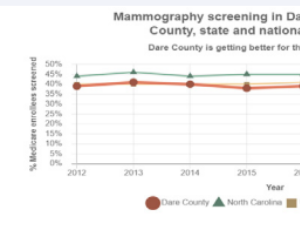 Abstract We are a rural hospital with access to care barriers historically linked to geography. We see a disproportionate percentage of late stages of breast cancer, with correspondingly worse mortality rates. A decade ago, screening mammogram rates were low .....
Abstract We are a rural hospital with access to care barriers historically linked to geography. We see a disproportionate percentage of late stages of breast cancer, with correspondingly worse mortality rates. A decade ago, screening mammogram rates were low ..... -
November 25, 2022 Case Report
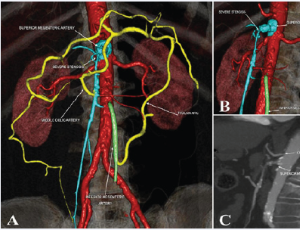 Abstract Chronic mesenteric ischemia (CMI) is an uncommon entity occurring in patients with severe stenosis of at least 2 of the 3 mesenteric vessels. It produces abdominal pain and nutritional status deterioration. Although open revascularization has been th.....
Abstract Chronic mesenteric ischemia (CMI) is an uncommon entity occurring in patients with severe stenosis of at least 2 of the 3 mesenteric vessels. It produces abdominal pain and nutritional status deterioration. Although open revascularization has been th..... -
November 25, 2022 Research Article
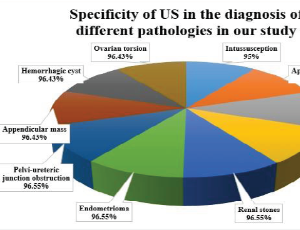 Abstract Background: Ultrasound (US) is considered the preferred imaging tool to evaluate the surgical causes of acute abdominal pain. Methods: Our study aimed to reappraise the role of US in the evaluation of surgical causes of acute abdominal pain in pedia.....
Abstract Background: Ultrasound (US) is considered the preferred imaging tool to evaluate the surgical causes of acute abdominal pain. Methods: Our study aimed to reappraise the role of US in the evaluation of surgical causes of acute abdominal pain in pedia..... -
January 08, 2023 Case Report
 Abstract Pneumomediastinum (PNM) is a pathological condition characterized by the penetration of air into the mediastinal space. The most frequent cause of pneumomediastinum is trauma that can cause burst rupture of the esophagus, trachea or bronchi (closed t.....
Abstract Pneumomediastinum (PNM) is a pathological condition characterized by the penetration of air into the mediastinal space. The most frequent cause of pneumomediastinum is trauma that can cause burst rupture of the esophagus, trachea or bronchi (closed t.....