Recent Articles
-
October 02, 2023 Research Article
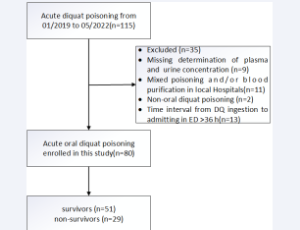 Abstract Background: Diquat (DQ) poisoning is an important public health and social security agency. This study aimed to develop a prognostic model and evaluate the prognostic value of plasma DQ concentration in patients with acute oral DQ poisoning, focusing.....
Abstract Background: Diquat (DQ) poisoning is an important public health and social security agency. This study aimed to develop a prognostic model and evaluate the prognostic value of plasma DQ concentration in patients with acute oral DQ poisoning, focusing.....