Recent Articles
-
August 11, 2023 Opinion Article
 Abstract Up to now, Diagnosis and therapy of multiple sclerosis (MS) are not optimal, they need improvement. We present a diagnostic parameter and two therapeutic methods that offer a prospect of success without burdening the patient. They are the biomarker N.....
Abstract Up to now, Diagnosis and therapy of multiple sclerosis (MS) are not optimal, they need improvement. We present a diagnostic parameter and two therapeutic methods that offer a prospect of success without burdening the patient. They are the biomarker N..... -
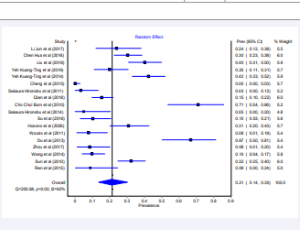
November 06, 2016 Research Article
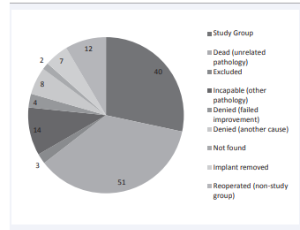 Abstract Purpose: The Dynesys system remains the most widely implanted posterior non fusion pedicle screw system. Various study designs used in investigations with good to excellent short- and mid-term results have been reported in the current literature. How.....
Abstract Purpose: The Dynesys system remains the most widely implanted posterior non fusion pedicle screw system. Various study designs used in investigations with good to excellent short- and mid-term results have been reported in the current literature. How.....