Recent Articles
-
August 13, 2021 Original Research
 Abstract Burns are serious traumatic injuries. Their management follows a well-established hierarchy of priorities. Lifesaving is the primary objective, then after securing survival of the burn victim, treatment aims at functional recovery, and finally aesthe.....
Abstract Burns are serious traumatic injuries. Their management follows a well-established hierarchy of priorities. Lifesaving is the primary objective, then after securing survival of the burn victim, treatment aims at functional recovery, and finally aesthe..... -
July 30, 2021 Short Communication
-
July 30, 2021 Research Article
 Abstract Male, Long-Evans rats with lateral hypothalamic stimulating electrodes were tested using a threshold-tracking procedure. This procedure determined the minimum stimulation frequency (i.e., stimulation threshold) necessary to maintain ?30 presses/min d.....
Abstract Male, Long-Evans rats with lateral hypothalamic stimulating electrodes were tested using a threshold-tracking procedure. This procedure determined the minimum stimulation frequency (i.e., stimulation threshold) necessary to maintain ?30 presses/min d..... -
July 06, 2021 Review Article
 Abstract The objective of this review is to assess the hazardous effects of substance abuse in Ethiopia. Substance abuse is a maladaptive pattern characterized by repeated adverse consequences related to the repeated use of the substance. Alcohol, khat and ci.....
Abstract The objective of this review is to assess the hazardous effects of substance abuse in Ethiopia. Substance abuse is a maladaptive pattern characterized by repeated adverse consequences related to the repeated use of the substance. Alcohol, khat and ci..... -
June 25, 2021 Original Research
 Abstract Background: Depression in the peripartum period is prevalent in low-income-countries. The identification of women needing referral is often lacking and on the other hand, women in need of support and treatment do not make use of existing support. .....
Abstract Background: Depression in the peripartum period is prevalent in low-income-countries. The identification of women needing referral is often lacking and on the other hand, women in need of support and treatment do not make use of existing support. ..... -
May 29, 2021 Research Article
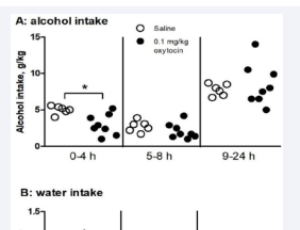
 Abstract Endogenous opioid system plays an essential role in regulating alcohol consumption. Genetic deletion of mu-opioid receptor (MOP-r) decreases alcohol intake and reward in mouse models. A single-nucleotide polymorphism (SNP; A118G, rs1799971) in human .....
Abstract Endogenous opioid system plays an essential role in regulating alcohol consumption. Genetic deletion of mu-opioid receptor (MOP-r) decreases alcohol intake and reward in mouse models. A single-nucleotide polymorphism (SNP; A118G, rs1799971) in human ..... -
May 12, 2021 Perspective
 Abstract Risk factors for severe COVID-19 pathology are currently being investigated worldwide. Using a mouse model, we identify heavy alcohol and cannabinoid consumption as risk factors for increased pulmonary pathology in the setting of exposure to a microb.....
Abstract Risk factors for severe COVID-19 pathology are currently being investigated worldwide. Using a mouse model, we identify heavy alcohol and cannabinoid consumption as risk factors for increased pulmonary pathology in the setting of exposure to a microb..... -
February 23, 2021 Short Communication
 Abstract Objective: We intend to provide a subjective and scientific report on a tragic incident happened during COVID-19 outbreak in Iran which is a mass methanol poisoning in one of the provinces in Iran. Unexpectedly, this poisoning has outnumbered COVID-1.....
Abstract Objective: We intend to provide a subjective and scientific report on a tragic incident happened during COVID-19 outbreak in Iran which is a mass methanol poisoning in one of the provinces in Iran. Unexpectedly, this poisoning has outnumbered COVID-1..... -
January 23, 2021 Research Article
 Abstract Background: A worldwide and ever-growing population of children are using psychoactive substances. To slow this problem, the Child Intervention for Living Drug-Free (CHILD) Curriculum was created to train treatment providers on how to screen, assess,.....
Abstract Background: A worldwide and ever-growing population of children are using psychoactive substances. To slow this problem, the Child Intervention for Living Drug-Free (CHILD) Curriculum was created to train treatment providers on how to screen, assess,..... -
January 23, 2021 Research Article
 Abstract Background: Substance use during pregnancy and early parenting years is a well-known global public health problem, but the literature comparing treatment programs for this subpopulation across countries is limited. This article both describes three w.....
Abstract Background: Substance use during pregnancy and early parenting years is a well-known global public health problem, but the literature comparing treatment programs for this subpopulation across countries is limited. This article both describes three w..... -
October 19, 2017 Research Article
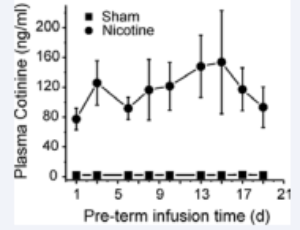 Abstract Rationale: In-utero exposure to tobacco smoke is strongly associated to sudden infant death syndrome (SIDS) with cardiac arrhythmias considered the final cause of death. The mechanisms causing these arrhythmias remain largely unknown but seem to be l.....
Abstract Rationale: In-utero exposure to tobacco smoke is strongly associated to sudden infant death syndrome (SIDS) with cardiac arrhythmias considered the final cause of death. The mechanisms causing these arrhythmias remain largely unknown but seem to be l..... -
April 14, 2017 Case Report
 Abstract This article presents the first Mexican study about the relationship between cocaine/crack use disorder and antisocial behavior, based on the comparison of cocaine/crack patients and non stimulant drug patients (attended for alcohol, cannabis, heroin.....
Abstract This article presents the first Mexican study about the relationship between cocaine/crack use disorder and antisocial behavior, based on the comparison of cocaine/crack patients and non stimulant drug patients (attended for alcohol, cannabis, heroin..... -
January 17, 2014 Editorial