2022 Volume 9 - Issue 4
-
December 30, 2022 Research Article
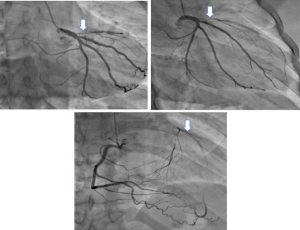
 Abstract There is little longitudinal BP data in patients with thoracoabdominal aortic dissections (TAAD). In patients attending an aortic diseases clinic, thoracic aortic dissection (TAD) having false lumen extensions past the renal arteries (Group 1) were c.....
Abstract There is little longitudinal BP data in patients with thoracoabdominal aortic dissections (TAAD). In patients attending an aortic diseases clinic, thoracic aortic dissection (TAD) having false lumen extensions past the renal arteries (Group 1) were c.....