Adolescent Idiopathic Scoliosis and Sport: Allies or Enemies?
- 1. La Maison de la Scoliose, Villeneuve d’Ascq, France
- 2. SSR pédiatrique Marc Sautelet, Villeneuve d’Ascq, France
- 3. IFMKNF, Loos, France
- 4. ILIS, Loos, France
ABSTRACT
Introduction: Health professionals generally encourage Physical Activities and Sport (PAS) as it helps for patients suffering from a chronic disease, such as Adolescent Idiopathic Scoliosis (AIS). The experts recommend PAS for AIS patients. But, this notion remains contested by some physicians. The aim of this review is to elucidate the debated impact of Physical Activity and Sport (PAS) on patients with Adolescent Idiopathic Scoliosis (AIS). We carried out a systematic literature review to elucidate the impact of PAS on AIS and to bring a scientific answer to this controversial topic.
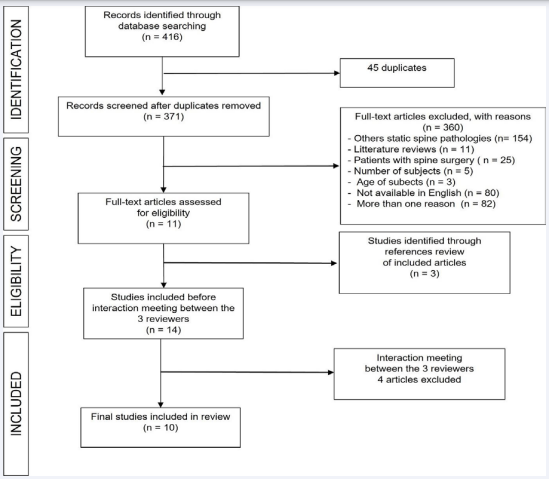
Materials and Methods: We performed a systematic review of the literature according to PRISMA statement and STARTLITE methodology. The search was conducted in PubMed, Cochrane and PEDro, from 1966 to 2019, by 3 independent reviewers.
Results: 416 publications were found, 10 of which were included. These articles had a low level of evidence (level 3-4, grade B-C). The main results are:
- Classical ballet dance and gymnastics increase the risk of having AIS, especially for girls with hyperlaxity that practice at a high level.
- Asymmetric sports (rackets sports) do not increase the risk of scoliosis.
- Swimming is not particularly recommended in AIS.
Conclusions: Regular PAS is commonly recommended in AIS. However, some PAS seem to increase the risk of having scoliosis, especially if they are practiced at a high level (classical ballet dance, gymnastics). In AIS, we recommend to vary different physical activities and to avoid intense practice (no more than 10 hours per week).
CITATION
Jean-François C, Anthony B, Amélie D (2022) Adolescent Idiopathic Scoliosis and Sport: Allies or Enemies? Ann Sports Med Res 9(2): 1193.
INTRODUCTION
Health professionals generally encourage Physical Activities and Sport (PAS) as it helps to maintain good health [primary prevention] in healthy individuals but also for patients suffering from a chronic disease, such as Adolescent Idiopathic Scoliosis (AIS) [1]. AIS is considered a chronic pathology that can lead to various complications including bone mass decrease [2], postural control disorder, a strong disturbance of dynamic proprioceptive pathways [3-5] linked to body image [6], alteration of breathing function [7], psychological disorders [8] and chronic back pain [9]. Indeed, PAS is already known to help limit these complications in other diseases (Table 1).
Table 1 : Adolescent Idiopathic Scoliosis complications versus Physicaland Sportive Activities benefits.
|
AIS complications |
PSA benefits |
|
Bone mass decrease |
Prevention |
|
Postural stability decrease |
Improvement |
|
Psychological disorders |
Improvement |
|
Perturbation of the corporal image |
Improvement |
|
Decrease of the breathing function |
Improvement |
|
Back pain |
Decrease |
AIS = Adolescent Idiopathic Scoliosis PSA = Physical and Sportive Activities
A decrease of bone mass, osteopenia is found in 20 to 38% of AIS [2] and is a risk factor in the progression of AIS [10]. Practicing a PAS is already a therapeutic option suggested for AIS patients with osteopenia. In fact, resistance and impact sports have been shown to improve bone mineral density [10- 12]. Multiple AIS studies indicate postural orthostatic control disturbance [13], but it is difficult to determine if this disturbance is secondary to the scoliotic curvature or if it influences the evolution of AIS. Nevertheless, there is a statistical link between lumber discopathy and postural orthostatic loss of control. Recent studies carried out with athletic individuals proved that practicing PAS leads to better postural control, especially as proprioceptive and vestibular information is better integrated [14-16]. Studies carried out on adolescents are rare, however, a study by Bruyneel et al. showed that dancing enables a better adaptation of postural control in children between 8 and 16 years of age [15]. Mentally, it has been clearly shown that adolescents with AIS have more psychological issues, low self-esteem and show signs of depression [8]. A recent literature review concluded that adolescents who practice PAS suffer from less of these psychological disorders [17]. Others have proved that AIS patients develop a distorted body image [18]. Segreto et al. found that athletic adolescents with AIS have a better body image those non-athletic individuals. In fact, even the parents of athletic AIS patients had a better perception of their child’s deformity [19]. Another common and dreaded complication in adolescents with major AIS is the impact on breathing by a diminished lung capacity which leads to a lower tolerance to physical exercise [7]. Nonetheless, this can be improved with aerobic training as shown by Shen et al. [20]. A recent literature review revealed a prevalence of 34.7% to 42.0% of low back pain in AIS [9]. Frequent aerobic PAS practice is associated with a lower probability that adolescents will suffer from low back pain [21].
These examples show the positive impacts of PAS in AIS and the International Society on Scoliosis Orthopedic and Rehabilitation Treatment (SOSORT) recommends PAS for AIS patients [22]. Although in practice, this notion remains contested by some physicians [19, 23]. AIS patients are consistently deterred from sports that require asymmetric muscular activity, such as racket sports, that are known for worsening the scoliotic curvature. On the other hand, some PAS are frequently recommended, such as swimming, even though there is no strong evidence to support this claim [24, 25]. Thus, this systematic review aims to elucidate the impact of PAS on AIS patients based on the literature.
METHODS
We carried out a systematic review of literature according to the following criteria (Table 2):
Table 2: STARLITE and PICO strategies used for the literature review.
|
Step 1: Definition of the topic's revue Goals: |
Answer to the 3-following questions: - What are the PSA effects on adolescents with AIS? - What is the AIS prevalence in function of PSA type? - What are the PSA recommended in AIS? |
|
Step 2 PICO strategy |
- Participants: adolescents with scoliotic deformation - Intervention: practical evaluation of a PSA on the risk of presenting AIS with the prevalence measure - Comparator: non practicing PSA evaluation on the risk of presenting AIS with the prevalence measure - Outcomes: flux diagram according to the PRISMA method |
|
Step 3 STARLITE strategy
|
- Sampling strategy (s): Systematic review - Type of studies (T): controlled studies and cohort monitoring - Approaches (A): electronic research with the following sources: PubMED, PEDro, Cochrane and in the highlighted articles. - Range of years (R): from the 1st of January 1983 until the 31st of December 2019 - Limits (L): publishing in English only - Inclusion: at least 30 topics evaluated, Cobb superior angle or equal to 10°, trunk rotation angle superior or equal to 5° on the Bunnel's scoliosometer, scoliotic idiopathic curvature - Terms used (T): cf. algorithm research - Exclusion (E): literature reviews, expert's recommendations, articles which do not include PSA, articles which don't include scoliotic deformations, individuals aged under 10 years, scoliotic subjects with arthrodesis surgery |
|
Step 4 Completion of the literature's |
review The articles obtained by PICO and STARLITE strategies were databased in a google drive notepad where the 3 reviewers could have access |
|
Step 5 Filter |
3 independent reviewers selected different articles depending on keywords, in the title or abstract |
|
Step 6 Comparing the researches results |
Flux diagram according to the PRISMA method upon 416 articles found in the database |
|
Step 7 Eligibility |
14 articles were conserved after checking their eligibility and after being compared between the 3 reviewers 7 articles are immediately included For 7 articles, a meeting was set up in order to interact about the differences of opinion between the 3 reviewers: 3 articles have been included and 4 were excluded (heterogeneous population, imprecise methodology...) |
|
Step 8 Including articles |
Finally, 10 articles were included for analysis |
PSA : Physical and Sportive Activities AIS : Adolescent Idiopathic Scoliosis PICO : Participants-Intervention-Comparator-Outcomes.
- Objective: to give clear guidelines regarding the practice of PAS in AIS.
- Database: PubMed, Cochrane, PEDro, from 1966 to 2019.
- Use of the PRISMA-P 2015 checklist [26].
- Use of STARLITE [Sampling strategy
- Type of studies - Approaches - Range of years - Limits - Inclusion - Terms used - Exclusion] [27] and PICO (Patient-Intervention-ComparisonOutcome) [28] methodologies to define the review’s parameters.
hysiotherapist, a teacher in adapted physical activities, a medical doctor specialized in physical medicine and rehabilitation) participated in this review. These three independent examiners carried out article screening and evaluated their eligibility. These articles were selected by consensus from inclusion and exclusion criteria, described in Table 2. A conciliation meeting was organized in case of opinion divergence.
The remaining articles were included unanimously by the 3 reviewers.
- Research problem: this review seeks to answer the 3 following questions:
What are the effects of PAS on adolescents with AIS?
What is the prevalence of AIS for each type of PAS?
What are the PAS recommendations in AIS?
- Research algorithms: the MeSH key is the following
“((sport[MeSH Terms]) AND (scoliosis[MeSH Terms])) OR ((sport[MeSH Terms]) AND (spinal curvature[MeSH Terms])) OR ((physical, activity [MeSH Terms]) AND (scoliosis[MeSH Terms])) OR ((physical, activities [MeSH Terms]) AND (scoliosis[MeSH Terms])) OR ((dancing[MeSH Terms]) AND (scoliosis[MeSH Terms])) OR ((dancing[MeSH Terms]) AND (spinal curvature[MeSH Terms]))”.
These terms are used according to our research topic. The keywords “sports” and “sport” are completed by the keywords” physical activity” and “physical activities”, which are more often used in recent publications. The keyword “scoliosis” is completed by “spinal curvature”. The keyword “dancing” has been added because some authors do not classify this activity as a sport.
- The data extraction method is made according to an Excel board including: author’s name, year of publishing, study type, number of individuals evaluated, AIS prevalence, evaluation method used for the AIS diagnostic, statistic results… The included studies are classified according to their level of evidence and reviewers prioritize the articles based on the amount of evidence Table 3.
Table 3: Prevalence of scoliotic deformations in athletic population.
|
Authora |
Study type |
Population |
PSA |
Evaluation |
Results: prevalence of the scoliotic deformations |
|
Kenanidis 2008 [3] |
Controlled Retrospective Level 3 Grade C |
1134 Sportive Subjects mean age 13,4 years 1253 Controls mean age 13, 4 years |
Aquatic sports Team sports Racket sports Diverse individual sports |
Clinical and radiographic evaluation |
NS |
|
Longworth 2014 [10] |
Prospective Controlled Matched Level 3 Grade C |
30 Sportive Subjects mean age 12 years 30 Controls mean age 12 years |
Classic Danse |
Scoliometer |
p = 0,006
Classic dancers = 30% Controls = 3,33 % |
|
Zaina 2014 [14] |
Controlled Retrospective Level 3 Grade C |
112 Sportive Subjects mean age 12,5 years 217 Controls mean age 12, 5 years |
Competition swimming |
Scoliometer |
NS for TRA > 5°
For TRA > 7° Girls : p < 0,05 |
|
Zaina 2016 [15] |
Controlled Retrospective Level 3 Grade C |
102 Sportive Subjects mean age 12 years 203 Controls mean age 12, 3 years |
Competition tennis |
Scoliometer |
NS |
|
Tanchev 2000 [16] |
Retrospective Cohort No control group Level 4 Grade C |
100 Sportive Subjects mean age 12,4 years |
Gymnastics |
Clinical and radiographic evaluation |
Gymnasts = 12% |
PSA : Physical Sportive Activity,NS : Non Significative,TRA = Trunk Rotation Angle
Table 4.
Table 4: Correlation evaluation between Physical Activity and Sport [PAS] and Adolescent Idiopathic Scoliosis [AIS].
|
Author |
Study type |
Population |
PSA |
Results |
|
Meyer 2006 [2] |
Retrospective Controlled Level 3 Grade C |
201 AIS mean age 14,5 years Cobb angle ≥ 10°
192 Controls mean age 15,3 years |
Gymnastics Aquatic sports Team sports Various sports |
Gymnastics p <0.001 PSA from outside p <0.005 Team sport p <0.001 Fighting sport p <0.005 |
|
Meyer 2008 [13] |
Retrospective Controlled Level 3 Grade C |
169 AIS mean age 14,8 years Cobb angle ≥ 10°
100 Controls mean age 15,2 years |
Gymnastics Aquatic sports Team sports Various sports |
Practice of a PSA DMC versus SMC : p=0,006* DMC versus control : NS SMC versus control : NS |
|
McMaster 2015 [1] |
Retrospective Controlled Level 3 Grade C |
79 AIS mean age 15,1 years Cobb angle > 10°
77 Controls mean age 14,7 years |
Gymnastics Dance Team sports Various sports |
Risk increasing of presenting AIS if non- participation Danse p = 0,045* Gymnastics p = 0,005* Karate p = 0,005* Skating p <0,001* Horse riding p = 0,003* |
|
Diarbakerli 2016 [12] |
Retrospective Controlled Level 3 Grade C |
239 AIS mean age 16 years Cobb angle ≥ 10°
58 Controls mean age 14,6 years |
Vigorous PSA Moderated PSA Walking |
NS |
|
Watanabe 2017 [11] |
Retrospective Cohort No control group Level 4 Grade C |
2600 AIS mean age 13,9 ans Cobb angle median 14° |
Gymnastics Classical dance Swimming Team sports Racket sports |
Risk increasing of presenting AIS if participation Classic dance
Risk decreasing of presenting AIS if participation Basketball Badminton Volleyball |
AIS : Adolescent IdiopathicScoliosis PSA: Physical and Sportive Activity DCM : Double Curvature major SCM : Simple Curvature major
NS : Non Significative.
Table 5.
Table 5: Influence of PSA in AIS.
|
PSA TYPE |
INFLUENCE ON AIS |
|
Gymnastics |
No deleterious effect if practiced at moderated level Effect potentially deleterious if intensive practice and/or early practice |
|
Classic dance |
No deleterious effect if practiced at moderated level Effect potentially deleterious if intensive practice |
|
Racket sports |
No deleterious effect in competitive practice Protecting effect from badminton |
|
Swimming |
No protecting effect Effect potentially negative if intensive practice |
|
Equitation |
Protecting effect |
AIS = Adolescent Idiopathic Scoliosis PSA = Physical and Sportive Activities.
Figure 1
Figure 1 PRISMA flow diagram.
RESULTS
Using the various search engines, 416 publications were found with three additional publications identified in their bibliography, making an initial total of 419 articles. From these we found 45 articles that crossover. 360 articles were excluded as they did not respect the inclusion/exclusion criteria (Figure 1). Fourteen studies were selected after their eligibility was further checked by the 3 reviewers. Seven articles were immediately included, 7 articles required a conciliation meeting because of opinion divergence between reviewers: 3 articles were included, 4 were excluded (heterogeneous patient population, unspecified methodology…). In the end, 10 articles were accepted unanimously. The most evaluated sports are: gymnastics (5 studies), dancing particularly classical ballet dance (3 studies), racket sports (2 studies), aquatic sports especially swimming (2 studies) and horse riding? (2 studies). In some of the selected articles several PAS were evaluated within the same study. For more clarity, results were represented according to the different PAS type.
Gymnastics
A study by Tanchev et al., found a high prevalence of AIS (12%) in high level female gymnasts (> 12 hours training per week). The scoliotic curvatures were exclusively lumbar and thoraco-lumbar, mostly with right convexity, with a minor Cobb angle (mean = 16°) [29]. On the other hand, the study carried out by Watanabe et al., on 2600 adolescent females, of which 47.2% have AIS with a Cobb angle higher or equal to 15°, does not show a significant correlation between AIS and the practice of gymnastics [30]. Mc Master et al., evaluated groups of scoliotic and non-scoliotic adolescents and highlighted the fact that not participating in gymnastics lessons (OR 2.7; IC at 95% [1.4-5.4]; p= 0.005) leads to a higher risk of having AIS [31]. A transversal study by Meyer et al. with AIS adolescents and non-scoliotic controls found that gymnastics is the most popular (36.3%; p<0.001) and practiced PAS in the scoliotic group compared to the control group (OR 3; IC at 95% [1.9-4.9]) [32]. Scoliotic adolescents who practice gymnastics are more hyperlax than non-scoliotic adolescents who do not practice gymnastics (p <0.05) [32]. The same team evaluated the correlation between scoliotic curvature, single or double major curvature (SMC, DMC) and the type of PAS practiced in AIS. It was significantly revealed that scoliotic adolescents with DMC practice more gymnastics than the scoliotic group with SMC, who themselves practice more gymnastics than the control group [33].
Classical ballet dance
Longworth et al. studied the prevalence of scoliotic deformations in 30 female ballet dancers versus 30 controls. The mean age of patients was 12 years old, with a minimum of 3 years of experience and practiced at least 4 hours of dancing per week [34]. The results showed a scoliotic deformation for 30% of the ballet dancers versus 3.3% for the non-dancers. Thus, suggesting ballet dancers have a higher risk of having a scoliotic deformation (OR: 12.4; p=0.006). Hyperlaxity was found in 21 ballet dancers compared to only one adolescent in the control group (p=0.04). The study by Watnabe et al. featuring 2600 female adolescents (mean age = 13.8), shows a significant correlation between the risk of having AIS and the practice of ballet [30]. The risk increases if the patient started classical dance before the age of 7 [OR 1.3; IC at 95% (1-1.7]) [30]. This work also showed that a higher frequency of training sessions can be correlated to an increased risk factor of AIS. Indeed, 58.1% of dancers who train 2 to 3 times a week have AIS (OR 1.5; IC at 95% [1-2.1]) whereas 69.7% of dancers who practice ballet 4 times a week or more have AIS (OR 2.30; IC at 95% [1-4.9]) [30]. But a contradictory study by McMaster et al. on 79 AIS girls (mean age = 15.1) versus 77 controls (mean age = 14.7), shows that a lack of participation in classical dance lessons increases the risk of having AIS (OR 2.2; IC at 95% [1-4.7]; p=0.045) [31].
Racket sports
Zaina et al. studied the prevalence of scoliotic deformations on 102 adolescents who are competitive tennis players (with an average of 4 and a half hours of training per week) and 203 controls [25]. The comparison did not put forward any significant differences between both groups. Moreover, Watnabe et al.’s study also shows no significant correlation between having scoliosis and practicing tennis [30]. Although the authors did find that practicing badminton at least 4 times a week reduces the risk of having AIS (OR 0.6; IC at 95% [0.4-0.8]).
Swimming
level adolescent swimmers (8 to 15 hours of training per week) and 217 controls, found that high level female swimmers have an important risk of scoliosis (OR 2.5; IC at 95% [1.2-5.2]). The evaluation criteria for AIS were a trunk rotation angle higher than 7° on the scoliometer [24]. On the other hand, Watnabe et al., show no evidence that swimmers have a higher risk of having AIS [30]. Horse riding
McMaster et al. found in their controlled study that not practicing horse riding increases the risk of having AIS (OR 3.1; IC at 95% [1.5-6.5]; p= 0.003) [31].
Other sports
evel adolescent athletes (with a continuous practice of a PAS during at least 2 years and a training regime of at least 10 hours per week) compared with 1253 adolescent controls. The risk of having AIS in the 2 groups was not significantly impacted by high level training [35]. Watnabe et al., found in their study that female adolescents have a lower risk of having AIS if they practice basketball (OR 0.6; IC at 95% [0.5-0.9]), or volleyball (OR 0.7; IC at 95% [0.5-1]) [30]. In the same way, McMaster et al. found in 79 adolescents with AIS versus 77 controls that non-participation in karate classes (OR 2.7; IC at 95% [1.4-5.4]; p=0.005), or skating (OR 5.7; IC at 95% [2.8-11.5]; p0.05).
DISCUSSION
Limitations
The aim of this study was to identify the PAS recommendations for AIS patients as well as analyze their impact. Before assessing the results of our review, it is important to highlight the scarcity of the scientific literature on this issue. Indeed, there are few studies – less than 500 publications in over 30 years – only one of which is a prospective study. But the quality of the work published is also lacking. Moreover, the evaluation of PAS in AIS is only based on non-standardized questionnaires with possible information and memorization bias. Even the diagnostic methodologies of AIS (radiography, surface topography, clinical exam) and population of individuals can be heterogeneous (gender, PAS type). However, a medical practician who treats AIS is often confronted with the same question: “Which sports is my child allowed to practice?”. It seems important for us to provide evidence-based answers and not recommendations based on beliefs. In this context, we have also suggested recommendations based on our own observations.
General synthesis
Nevertheless, not participating in PAS does seem to double the risk of having AIS [31].
Practice of gymnastics and AIS
As in Kenanidis et al.’s 2010 literature review, we found that AIS prevalence is more important in adolescents who practice gymnastics [37]. Interestingly, gymnastics is the most popular PAS for females with AIS, especially those with DMC [32]. There are several possible explanations: gymnastics and AIS have a feminine predominance; hyperlaxity is a symptom often found in gymnasts and adolescents with AIS [29, 32, 38]. Therefore, scoliotic female adolescents could preferentially choose gymnastics because joint laxity gives them more physical ability for this PAS. These two factors, feminine predominance and hyperlaxity, could explain why studies find a high prevalence of AIS in gymnasts, especially when it is practiced at a high level [29,32]. The intensive practice of this PAS could have damaging effects on the spine for immature and hyperlax female adolescents. This is likely to be caused by repeated mechanical stress on the spine although no study has evaluated the evolution of the scoliotic curvatures of AIS patients who practice gymnastics. It must also be noted that a moderate practice of gymnastics has not been linked to an increased risk of AIS [31- 30].
Therefore, intensive practice of gymnastics is not recommended for adolescents with AIS, especially if they have ligament hyperlaxity.
Practice of classical dance and AIS
Two out of three studies have shown a higher risk [up to 12 times] of having AIS for classical dancers [30- 34]. In fact, this risk increases with the duration and intensity of trainings [30]. Just as in gymnastics, ligament hyperlaxity and feminine predominance in AIS probably encourages female adolescents to choose this activity [34]. The moderated practice of dancing does not increase the risk of having AIS [31]. Based on the recommendation given for gymnastics, intensive practice of classical dance is not recommended in AIS, especially when associated to ligament hyperlaxity.
Practice of racket sports and AIS
A common belief among parents but also by health care professionals is that practicing an asymmetrical sport, such as racket sports, rises the risk of having AIS [25]. Yet, the prevalence of having AIS is not higher for an adolescent tennis player, even if this sport is practiced at a high level [25- 30]. In fact, this risk is even lower for female adolescents who practice badminton [30].
Racket sports do not increase the risk of having AIS and are not contraindicated, even if practiced at a high level.
Practice of swimming and AIS
In practice, swimming is the most recommended sport for AIS patients although there is no strong scientific evidence to back this recommendation [24]. On the contrary, competitive swimmers have 1.86 more risk of having AIS than the general population [24-39]. This risk is even multiplied by 2.5 for girls [24]. The high proportion of scoliosis in swimmers can be explained by the fact that it is often recommended in AIS [24]. Swimming, even at high level, does not protect against having AIS [31,32], nor does it improve osteopenia [40]. Bone mineral density in swimmers is lower than for people who practice impact sports [40]. Finally, high level female swimmers (8 to 15 hours training per week) have more rachalgia than female non-swimmers [24].
Swimming is not particularly recommended in AIS and must be practiced at a moderate intensity [less than 8 hours per week] in association with impact sports figure 2.
Figure 2: Example of adapted physical activity [climb].
Horse riding and AIS
Horse riding is rarely recommended in AIS because mechanical pressures on the spine can worsen back pain and promote AIS progression. However, this practice can stabilize the pelvis, respect lumbar lordosis by opening the trunk-thigh angle and encourage trunk straightening [41]. The assessment of horse riding does not seem to show an increased risk of having AIS [32]. Surprisingly, the lack of horse riding could increase the risk of scoliosis [OR 3.1; IC at 95% [1.5-6.5]; p=0.003] [31].
Horse riding does not increase the risk of having AIS and therefore is not discouraged in AIS.
High level sport practice and AIS
According to the recommendations made by the WHO (World Health Organization), adolescents should practice at least 60 minutes of PAS per day, or 7 hours per week [1]. But intensive practice should be avoided as it can lead to rachialgia, anxiety, poor body image, delays in puberty – all of which can already be found in AIS [42-44]. Studies carried out on athletic adolescents who train for up to 28 hours per week found this population presented a higher prevalence of AIS [24,29,34]. When practiced at a high level, some PAS can cause spine diseases (lumbar spondylolysis, discopathy, injuries, Scheuerman disease…) [45,46].
We recommend adolescents with AIS not to practice sports for more than 10 hours per week [curricular and extra-curricular PAS combined.]
Future recommendations
Our recommendations can be completed by the ones made by the SOSORT in 2016, particularly regarding PAS at school throughout the treatment, including during the brace treatment [22]. According to the SOSORT, PAS are not considered as part of the therapeutic arsenal in AIS. But we believe that specific PAS, supervised by a physical adapted activities teacher, can become a real therapeutic solution if combined with PSSE (Physiotherapeutic Scoliosis Specific Exercise) and orthopedic treatments such as a brace. These adapted PAS could become an additional tool to encourage the automatic postural correction of scoliotic curvature, previously learnt with a physiotherapist (Figure 2). These therapeutic technics based on adapted PAS will require scientific validation. It would be interesting to carry out new research regarding the link between PAS and AIS, especially with prospective studies, conducted over several years. It would allow us to evaluate the AIS incidence in adolescents practicing one single extra-curricular PAS (gymnastics, swimming, classical ballet dance …), but also to understand the consequences of these PAS on AIS progression.
CONCLUSION
This literature review shows that most PAS can be recommended in AIS, even though the robustness of the scientific data is lacking. Nevertheless, intensive practice of PAS, such as ballet or gymnastics, should be avoided in AIS, especially for adolescents with ligament hyperlaxity. Additional studies are necessary to confirm the impact of PAS on AIS patients. Such studies could lead to the inclusion of adapted PAS in the therapeutic arsenal for AIS treatment.
ACKNOWLEDGMENTS
Funding: This research was supported by the Cotrel Foundation - France Institute
Thanks for logistical assistance to “La Maison de la Scoliose”
![Example of adapted physical activity [climb].]( https://www.jscimedcentral.com/public/assets/images/uploads/image-1704886689-2.PNG)







































































































































