Improving Osteoporosis Assessment and Treatment among High Risk Minimal Trauma Fracture Patients at a Tertiary Centre: A Retrospective Interventional Study
- 1. Senior Pharmacist for Surgery and Critical Care, Pharmacy Department, Frankston Hospital, Australia
- 2. Monash University Pharmacy Student, Parkville, Victoria, Australia
Abstract
Objectives: Osteoporosis management rates among patients admitted with a minimal trauma fractures (MTF) have been low in hospitals around Australia. A study was conducted to determine the change in osteoporosis management rates at a metropolitan hospital after trials of different interventions.
Methods: A retrospective study of patients admitted to a tertiary hospital over a 12 months period (March 2019-March 2020) with MTF was conducted in Australia after an addition of an endocrinology registrar in February 2019 and an ortho-geriatric service in the previous 5 years. Rates of osteoporosis assessment and treatment were compared to the rates in 2010 and 2012-2013 periods, when educational and system based intervention were trialled. The results were analysed using chi squared.
Results: Osteoporosis assessment and treatment rates for the 2019-2020 cohort were 73.0% and 6.9% respectively. The assessment results were at 84.7% for patients who were admitted to the orthopaedic ward, which were similar to the results obtained from the interventional study in 2010 (87.6%, p=0.470) and higher than the 2012-2013 study results (12.5%, p<0.001). Majority of assessments were incomplete with less than 50% having vitamin D levels checked. The treatment rate for the 2019-2020 cohort had fallen significantly compared to the results in 2010 (71.6%, p<0.001) and compared to low results of the 2012-2013 period (20.9%, p<0.001).
Conclusion: The results of this study indicate that the additional medical services have not improved secondary osteoporosis management. Guideline recommended approaches, such as the implementation of a fracture liaison service should be considered to manage this condition.
Keywords
Osteoporosis; Minimal trauma fracture; Assessment; Treatment and hospital
Citation
Banakh I, Davey E, Hanna U, Montera H, Teh C, et al. (2021) Improving Osteoporosis Assessment and Treatment among High Risk Minimal Trauma Fracture Patients at a Tertiary Centre: A Retrospective Interventional Study. JSM Clin Case Rep 9(2): 1191.
INTRODUCTION
Osteoporosis is one of the leading causes of morbidity in Australia, and it is expected to affect over 6 million people by 2022 with a rate of fractures to exceed 180,000 per year [1]. Diagnosis of osteoporosis can be made by measuring bone mineral density (BMD), but it can also be presumed among “all individuals over the age of 50 who sustain a fracture following minimal trauma (such as a fall from standing height or less)” [1-3]. Despite the high prevalence, morbidity and significant mortality after hip and neck of femur fractures (NOF), the level of recognition of the underlying cause and subsequently the use of effective therapies is low [1,3-5]. This high level of under treatment exist across both primary and tertiary health care in Australia [1,6,7].
In order to address the treatment gap that has been identified in Australian hospitals in 2005 by Teede et al. [7], a tertiary centre in Victoria has implemented multiple interventions over a 15-year period. These interventions included: employment of an osteoporosis nurse until 2012, a trial of a pharmacist led junior medical staff osteoporosis education and assessment initiation for minimal trauma fracture (MTF) patients, and more recently introduction of an orthogeriatric team, and lastly an addition of a second endocrinology registrar to take referrals for osteoporosis assessment and treatment initiation [8,9]. In order to evaluate the effectiveness of the more recent intervention, a retrospective audit was conducted to determine the rate of osteoporosis assessment and treatment among MTF patients and to compare these with the results of previous interventions.
METHODS
PRO-OSTEO Extend 2 study was a retrospective, single centre study of all patients admitted to a tertiary centre in Victoria, Australia, with a presentation of a MTF between March 2019 to March 2020. The tertiary hospital provides both medical and surgical services with 454-beds, and over 120 surgical beds that include a dedicated orthopaedic ward. The study excluded any patient under the age of 18, patients on active osteoporosis therapy (not including calcium and vitamin D supplements), patients with fractures of the face, phalanges, tarsals, carpals, metatarsals or metacarpals, and those admitted with nonminimal trauma fractures [1]. Patients who had insufficient documentation to determine the nature of their fracture were also excluded from the study.
After obtaining a list of all patients who were admitted with a fracture from the study site’s health information service, patients who met the inclusion criteria had deidentified data collected from electronic health care records as well as digitised medical records. Information collected included: patient demographics, location of the MTF, history of previous fractures, co-morbidities and pre-admission medications that are associated with increased risk of falls and osteoporosis [1,8-10]. These were: hypertension, obesity, diabetes mellitus, dyslipidaemia, congestive cardiac failure, cerebrovascular accident/ transient ischaemic attack, ischaemic heart disease, peripheral vascular disease, gastrooesophageal reflux disease, cancer, hyperthyroidism, Parkinson’s disease, epilepsy, smoking status, history of alcohol abuse, chronic obstructive pulmonary disease, asthma, rheumatoid arthritis/inflammatory bowel disease and dementia [1]. Preadmission medications that were recorded included: proton pump inhibitors (PPIs), selective serotonin reuptake inhibitors (SSRIs)/ serotonin noradrenaline reuptake inhibitors (SNRIs), diuretics, levothyroxine, corticosteroids, benzodiazepines, tricyclic antidepressants (TCAs)/mirtazapine, antipsychotics, antihypertensives, phenytoin and valproate [1,11-13]. Additionally, pathology results from osteoporosis screens were collected and included full blood examination (FBE), urea and electrolytes (U&E), calcium and phosphate levels, liver function test (LFT), vitamin D levels, Thyroid Stimulating Hormone (TSH) level, Parathyroid Stimulating Hormone (PTH) level, testosterone level (for male patients not on hormone suppressive therapy), erythrocyte sedimentation rate (ESR) and free light chains and protein electrophoresis testing [14]. Osteoporosis therapy initiation or decision not to initiate due to reduced life expectancy or poor prognosis was recorded, along with mention of osteoporosis diagnosis or recommendations for dual energy X-ray absorptiometry (DEXA) scan or therapy in the discharge summary to the patients’ general practitioners.
The primary outcomes for PRO-OSTEO Extend 2 study were the osteoporosis assessment rate as specified in the medical notes and active osteoporosis therapy initiation rate (excluding calcium and vitamin D supplements). The secondary outcomes included: rates of orders of individual pathology tests for osteoporosis screen, levels of abnormal results and mention of osteoporosis in the discharge summaries to the general practitioners
The results were compared to the outcomes of previous interventions at the study site from 2010 and 2012-2013 respectively, after the addition of a second endocrinology registrar at the study site in February 2019 and the introduction of orthogeriatric services between 2013-2015 [8-10]. The second endocrinology registrar was tasked with taking on all internal osteoporosis management referrals at the study site. The registrar would primarily review patients with MTF who were aged below 65 years. Patients who were 65 years old or older were managed mostly by the orthogeriatric service.
Data was analysed using SPSS 24 with data normality checked using Kolmogorov-Smirnov test, while the rates of assessment and treatment comparisons were made using Chi-squared tests.
PRO-OSTEO Extend 2 study was not funded and has received an exemption from the human research ethics committee review due to the retrospective nature of the study with study registration number QA59887/PH-2019.
RESULTS
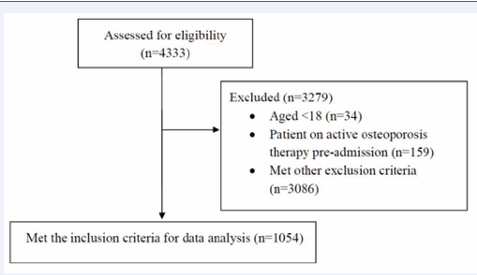
A total of 4333 patients were admitted to the study site between March 2019 and March 2020 with a diagnosis of a fracture. After screening patients for the inclusion and exclusion criteria, 1054 patients were left in the final analysis (Figure 1).
Figure 1 Patients screened for PRO-OSTEO Extend 2 study.
The average age of patients was 76.9 years and 68.2% were female, with 79.7% of patients aged over 65 years. Three hundred and twenty-nine patients (31.2%) were admitted to emergency department (ED) only, with direct discharge to preadmission residence. These patients were on average 4 years younger than those admitted to the orthopaedic ward (73.2 versus 77.2, p=0.040). The average length of hospitalisation was 6 days for the studied population.
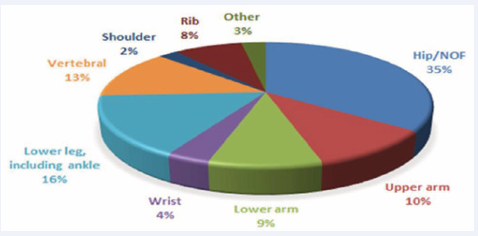
The overall population in this cohort was similar to the patients included into the study site’s osteoporosis studies in 2010 and 2012-2013 (Table 1), with similar gender distribution and age range overlaps. The most common comorbidities were hypertension, dyslipidaemia, gastroesophageal reflux disease and diabetes mellitus (Table 2). Previous fracture history was identified in 22.8% of patients. The most common sites of fracture during the incident admission were hip or NOF in 35.0%, lower leg in 16.0% and vertebral fractures in 13.0% (Figure 2).
Figure 2 Fracture distribution in 2019-2020 patient cohort.
The most commonly prescribed pre-admission medication which contributes to falls or fracture was: antihypertensives at 51.2%, PPIs at 34.1% and SSRI/SNRIs at 21.2% (Table 3). These results were similar to the cohort from 2012-2013 periods.
Table 1: Patient characteristics across three time periods.
|
Table 1: Patient characteristics across three time periods. |
|||
|
Characteristic |
2019-2020 N=1054 |
20108 N=74 |
2012-20139 N=560 |
|
Age mean (95%CI) |
76.9 (74.1-79.7) 73.2 (71.4-75.0) ED only 77.2 (75.6-78.8) Inpatients |
79.8 (76.8-82.8) |
77.5 (76.2-78.8) |
|
Gender Female (%) |
68.2% 240 (72.9%) ED only 479 (66.1%) Inpatients |
71.1% |
71.3% |
Table 2: Patient comorbidities in 2019-2020 cohort.
|
Table 2: Patient comorbidities in 2019-2020 cohort. |
|
|
Comorbidity |
Rate |
|
Hypertension |
52.8% |
|
Diabetes |
18.4% |
|
Dyslipidemia |
29% |
|
Obesity |
8.8% |
|
CCF |
8.2% |
|
IHD |
15.3% |
|
PVD |
4.6% |
|
CVA/TIA |
11.8% |
|
Parkinson’s |
3.4% |
|
Epilepsy |
3.1% |
|
Cancer |
18% |
|
Smoker |
10.5% |
|
Ex-smoker |
14.9% |
|
COPD |
11.9% |
|
Asthma |
9.2% |
|
RA/IBD |
3.8% |
|
Dementia |
15.4% |
|
GORD |
21.6% |
|
Hyperthyroidism |
1.8% |
|
Alcohol Abuse |
8.5% |
|
CCF = Congestive Cardiac Failure. IHD = Ischaemic Heart Disease. PVD = Peripheral Vascular Disease. CVA/TIA = Cerebrovascular Accident/ Transient Ischaemic Attack. COPD = Chronic Obstructive Pulmonary Disease. RA/IBD = Rheumatoid Arthritis/ Irritable Bowel Disease GORD = Gastro-Oesophageal Reflux Disease |
|
CCF = Congestive Cardiac Failure. IHD = Ischaemic Heart Disease. PVD = Peripheral Vascular Disease. CVA/TIA = Cerebrovascular Accident/ Transient Ischaemic Attack. COPD = Chronic Obstructive Pulmonary Disease. RA/IBD = Rheumatoid Arthritis/ Irritable Bowel Disease GORD = Gastro-Oesophageal Reflux Disease.
Over a third of patients were discharged to rehabilitation sites (36.5%), 42.2% patients went home from hospital, while 1.1% of patients from home and 2.3% of patients from residential care facilities required admission to nursing homes. There were 19 (1.8%) fatalities during the admissions for fractures.
STUDY OUTCOMES
Osteoporosis assessment and treatment rates for the 2019- 2020 cohorts were 73.0% and 6.9% respectively. The assessment results were at 84.7% for patients who were admitted to the orthopaedic ward, which were similar to the best results obtained from the interventional study in 2010 (87.6%, p=0.470) and significantly higher than the 2012-2013 study results (12.5%, p<0.001). The treatment rate for the 2019-2020 cohort had fallen significantly compared to the best results in 2010 (71.6%, p<0.001) and compared to low results of the 2012-2013 period (20.9%, p<0.001). Fifty-one patients (4.8%) were specified in the medical notes as not for active osteoporosis therapy.
Bisphosphonates were prescribed to 2.5% (versus 47.3% in 2010 and 15.4% in 2012-2013, p<0.001) and denosumab to 4.5% of patients. The prescribing of calcium supplements had dropped to 4.8% (versus 78.4% in 2010 and 27.7% in 2012- 2013, p<0.001), as did the use of colecalciferol to 17.0% (versus 79.7% in 2010 and 32.0% in 2012-2013, p<0.001) even though 17.9% were found to be with levels below 50nmol/L. Majority of prescribing of active therapy occurred at the study site (4.0% versus 8.6% in 2012-2013, p<0.001), and 2.9% at the study site associated rehabilitation centres (versus 7.0% in 2012-2013, p<0.001).
While the mention of osteoporosis assessment in the notes was at 84.7%, these were incomplete, with only 45.4% of patients having a vitamin D level checked, 53.4% with calcium levels,53.0% with phosphate levels, 43.0% with TSH levels, 18.3% with PTH levels, 16.7% with ESR, 7.2% with testosterone levels, and 25.0% with protein electrophoresis. Abnormal results among patients who had an osteoporosis assessment showed that 17.9% of patients had vitamin D deficiency, 7.9% had elevated PTH levels, 6.9% had suppressed and 4.6% elevated TSH levels, 4.8% of men had low testosterone levels and 0.19% had ESR above 100mm/hour. Abnormal corrected calcium levels were identified in 2.0% of patients, while 7.2% had abnormal phosphate levels.
|
Table 3: Pre-admission medications that increase risk of falls and osteoporosis. |
||
|
Medication |
2019-2020 |
2012-201310 |
|
PPIs |
34.1% |
42.9% |
|
SSRIs/SNRIs |
21.2% |
25.6% |
|
Diuretics |
19.6% |
9.8% |
|
Levothyroxine |
8.4% |
11.4% |
|
Corticosteroids |
8.7% |
9.5% |
|
Benzodiazepines |
17.5% |
26.1% |
|
TCAs/Mirtazapine |
9.4% |
7.0% |
|
Antipsychotics |
8.4% |
10.4% |
|
Antihypertensives |
51.2% |
52.9% |
|
Phenytoin/valproate |
2.4% |
9.5% |
|
Warfarin |
4.3% |
11.6% |
|
Aromatase inhibitor or androgen antagonist |
1.2% |
N/A |
|
PPIs = Proton Pump Inhibitors. SSRIs = Selective Serotonin Reuptake Inhibitors SNRIs = Serotonin Noradrenaline Reuptake Inhibitors. TCAs = Tricyclic Antidepressants. LMWH = Low Molecular Weight Heparin. N/A = Not Available. |
||
Discharge summaries specified a diagnosis of osteoporosis in 31.4% of patients, an increase from 6.6% in the 2012-2013 cohort (p<0.001), with 17.6% including treatment recommendations and 9.3% suggesting a DEXA scan. Only 7.7% of patients were found to have an endocrinology referral noted in their discharge summary. However, this was not always specifically for management of osteoporosis, but rather other comorbidities such as diabetes or hypothyroidism.
DISCUSSION
The results of this study indicate that over the last 15 years there has been a fluctuation in osteoporosis assessment rates, and while it has improved since the 2012-2013 period, many patients had significant lapses in completeness with nearly half the patients not having their vitamin D, calcium or phosphate levels checked. Among patients with some of the osteoporosis screening completed, a significant proportion had been identified to have abnormalities that would require follow up and review by an endocrinologist.
Even though the treating clinicians are considering osteoporosis assessment, the treatment rates have collapsed to below the levels identified in the initial Australian hospitals audit of 2003-2005 [7]. This indicates that the addition of a second endocrinologist registrar in 2019 and the orthogeriatric service in the previous 5 years have not improved osteoporosis management levels. Additionally, osteoporosis diagnosis was specified in less than a third of patients’ discharge summaries, similar to the previous results from 2012-2013 [9]. This would reduce the likelihood of any active osteoporosis therapies being started in general practice or primary care, which is already low as has been demonstrated by previous research in Australia and overseas, as well as by the high preadmission fracture history without any therapy [1,3,6].
It was also noted that a common reason for delaying osteoporosis treatment initiation during hospitalisation was the requirement for a dental check to avoid a rare adverse event of osteonecrosis of the jaw. As dental checks are not done on site during acute hospitalisation, the responsibility to initiate antiresorptive therapy was passed onto the general practitioner in primary care. This creates an unnecessary hurdle for many patients as dental checks are only needed for patient who has major dental work planned, such as tooth extractions and dental implants [15]. This adverse event is also more likely among patients who use high doses for oncological indications rather than for osteoporosis, with rates of 1 in 10,000 to 1 in 100,000 patients at osteoporosis indicated doses [15].
These results indicate that the treatment gap has widened at the study site and would require further intervention to reverse the falling treatment rates and to improve completeness and follow up of osteoporosis assessment. Previously successful approaches suggested by the national and international guidelines include the introduction of the fracture liaison service (FLS) [1,14,16,17]. Published results for FLS have demonstrated improved assessment, treatment and communication rates for osteoporosis management. A dedicated service to managing osteoporosis, especially for secondary prevention, is costeffective and would make a significant improvement in the identified results at the study site [16,17].
The main limitations of this study are the single centre approach and retrospective design. However, the study included a population that covered a complete 12 months period and showed no significant changes in the type of patients managed over the last decade. Another limitation of the study may have been that the additional service of the second endocrinology registrar may have been inadequately promoted to other clinicians, leading to a low referral rate. This was not examined as part of the study.
CONCLUSION
As osteoporosis prevalence continues to grow and contribute to a larger level of morbidity, mortality and cost of healthcare in Australia, an evidence-based approach for managing MTF is required. Interventions of adding non-dedicated services have failed to reverse poor levels of secondary treatment of osteoporosis. Alternative strategies, such as the implementation of a fracture liaison service are required to improve osteoporosis management in patients admitted with MTF as recommended by national and international guidelines.
Practice Impact Statement
Osteoporotic fracture management in Australian hospitals has been addressed using multiple interventions; however the most successful method (FLS) that is recommended by national and international guidelines is not regularly available in most hospitals. FLS should be introduced to most tertiary centres with orthopaedic services managing MTF patients.
REFERENCES
8. Banakh I. PRO-OSTEO Project (improving osteoporosis management in the acute hospital setting): a single-centre pilot study. Arch Osteoporos. 2011; 6: 157-165.
9. Banakh I, Chao S. PRO-OSTEO Extend I study (improving osteoporosis management.
10.in the acute and rehabilitation settings): multicentre audit. J Pharm Pract Res. 2015; 45: 38–45.