Laparoscopic Common Bile Duct Exploration for the Treatment of Choledocholithiasis
- 1. Department of Digestive System Surgery, Federal University of Triangulo Mineiro, Brazil
- 2. Department of General Surgery, Federal University of Triangulo Mineiro, Brazil
- 3. Department of Digestive System Surgery, Federal University of Triangulo Mineiro, Brazil
- 4. Department of Health Sciences, Federal University of Triangulo Mineiro, Brazil
- 5. Department of Health Sciences, Federal University of Triangulo Mineiro, Brazil
- 6. Department of Digestive System Surgery, Federal University of Triangulo Mineiro, Brazil
Abstract
Background and aim: Choledocholithiasisis a prevalent complication in cholelithiasis and the laparoscopic treatment may be an alternative approach. Evaluate the results of the laparoscopic approach of choledocholithiasis in patients with cholelithiasis.
Methods: A total of 290 patients with cholelithiasis associated with choledocholithiasis, including 191 women (65.86%), with a mean age of 58.4 years (21-80), were treated. A transcystic approach was used in 46 cases (15.86%) and longitudinal choledochotomy in 244 (84.14%). Conversion to open surgery was necessary in 26 cases (8.96%).
Results: There was no case of death and the rate of early complications was 9.31% (27 cases). Thirteen patients (4.48%) had a biliary fistula demonstrated by cholangiography and all cases were treated clinically. Hyperamylasemia was detected in 11 cases (3.8%) and four patients (1.38%) had mild acute pancreatitis. All patients were treated clinically. Three cases (1.03%) developed choleperitoneum after removal of the bile duct catheter on postoperative day 21, and perforation of the posterior wall of the common bile duct was observed in one patient (0.34%). Late complications occurred in six cases (2.07%), including a residual stone in four (1.38%), which was treated by therapeutic endoscopy. Two cases (0.68%) developed bile duct stenosis; good resolution was observed in one after dilation and biliary stenting andrecurrence of stenosis occurred in the other case, which required a biliodigestive anastomosis consisting of interposition of a jejunal tube.
Conclusions: The results showed that treatment of choledocholithiasis in a single procedure through laparoscopic bile duct clearance is safe, reproducible and associated with a low rate of complications, in addition to preserving sphincter functions of the duodenal papilla.
Keywords
Choledocholithiasis; Bile duct; Laparoscopic; Monti tube
Citation
Crema E, Terra-Júnior JA, Oliveira PF, de Carvalho Borges M, et al. (2021) Laparoscopic Common Bile Duct Exploration for the Treatment of Choledocholithiasis. JSM Clin Case Rep 9(3): 1193.
INTRODUCTION
The incidence of choledocholithiasis ranges from 8 to 20% [1] among patients with symptomatic biliary lithiasis. This incidence increases with age, reaching 31% in patients aged 61 to 70 years and 48% after the age of 70. These stones can migrate spontaneously to the duodenum or lodge in the duodenal papilla, causing bile duct obstruction, cholangitis and/or biliary pancreatitis [2].
Clinical factors such as cholestatic jaundice, acute pancreatitis and acute cholecystitis, laboratory factors such as elevated serum levels of alkaline phosphatase, gamma-glutamyltransferase and bilirubins, and imaging findings such as dilation of the bile duct or demonstration of stones inside the duct by ultrasound can predict the presence of choledocholithiasis [3,4].Laboratory and imaging exams should be recent and should be performed within a maximum period of 3 weeks prior to surgery. Goodquality images, expressed as the degree of ductal visualization, are essential.
Endoscopic treatment is indicated during the pre- and postoperative period or, possibly, during cholecystectomy, while surgical treatment consists of exploration of the cystic duct or classical choledochotomy, and also during laparoscopic cholecystectomy. The time of diagnosis of choledocholithiasis is important to establish the type of treatment.
The best complementary method for the diagnosis of choledocholithiasis, even in adults, is magnetic resonance cholangiopancreatography (MRCP), which shows a sensitivity of 95%, is not invasive, is multiplanar, does not use ionizing radiation, and is of low risk to the patient.
Bile duct exploration exclusively through the laparoscopic route has been suggested by some authors as the gold standard for the treatment of choledocholithiasis. Depending on the surgical conditions, access to the biliary tract can be obtained through the cystic or common bile duct. Historically, Ludwig Courvoisier first treatedcholedocholithiasis by choledochotomy in Switzerland in 1989. The endoscopic approach was used by Kasai in Japan in 1994 and by Classen and Demling in Germany in the same year. The first report of gallstone removal from the common bile duct by the laparoscopic approach dates back to 1991, which was performed by Jacobs, Peterlinand Philips.Resolution rates of choledocholithiasis by laparoscopic treatment ranged from 8.57 to 97.2% in the last decade, with minor complications of 2.9 to 9.1%.
In a recent meta-analysis including 15 studies, Liu et al. [5], compared the clinical effectiveness of choledocholithiasis treatment by laparoscopic common bile duct exploration and endoscopic sphincterotomy. The success of clearance was 92.7% for the laparoscopic procedure and 89.1% for the endoscopic procedure (p<0.05). The two groups did not differ significantly in terms of the frequency of retained stones, which was 5.2% in the laparoscopic group and 6% in the endoscopic group. There was also no significant difference in complications, hospital stay, or hospital cost [5].
In addition to possible complications (1 to 3%) that require laparotomy for treatment [6] such as bleeding, perforation and severe pancreatitis, the duodenal papilla approach with sectioning or dilation can cause long-term recurrence of common bile duct stones (2 to 16%), acute cholangitis (1 to 6%) and stenosis of the papilla (1 to 7%). Persistent reflux causes chronic inflammation, with consequent hyperplasia and development of bile duct cancer.
f laparoscopic common bile duct exploration in patients with acute cholangitis and common bile duct stones. Seventy-two patients with bile duct stones were admitted from January 2009 to December 2012. Laparoscopic common bile duct exploration by a transductal approach for common bile duct stones was performed in all patients. Thirty-seven patients underwent emergency laparoscopic common bile duct exploration and 35 underwent elective laparoscopic common bile duct exploration. The duration of the procedures, complications, retained stones, hospital stay, and total costs were compared between the two groups. Additionally, the characteristics of patients undergoing emergency laparoscopic common bile duct exploration were compared before and after surgery. There was no significant difference in the diameter of the common bile duct and the number of common bile duct stones based on imaging findings, or in the operative results between the two groups studied. No conversion to open surgery, major bile duct injuries or mortality was observed in the two groups. There was no significant difference in patients with or without acute or chronic cholecystitis, duration of surgery, overall hospital stay,or total costs between the two groups. Four cases of retained stones and four cases of biliary fistulae occurred in patients undergoing emergency laparoscopic common bile duct exploration and two cases of retained stones were observed in the group undergoing elective laparoscopic common bile duct exploration. The results showed that both procedures are safe and effective in the treatment of patients with nonsevere acute cholangitis with common bile duct stones [7].
Koc et al. [6], conducted a prospective randomized study on 120 patients to compare the efficacy, safety and surgical outcomes of laparoscopic common bile duct exploration plus laparoscopic cholecystectomy (LCBDE+LC) and ERCP plus laparoscopic cholecystectomy (ERCP+LC). The success rate was 96.5% in the LCBDE+LC group and 94.4% in the ERCP+LC group. Complication rates were 7% and 11.1% in the LCBDE+LC and ERCP+LC groups, respectively. The authors concluded that laparoscopic common bile duct exploration is an alternative therapeutic approach that has less morbidity, is of low cost, and permits earlier recovery and a reduced period of disability [6].
Noble et al. [8] compared the outcomes after endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy versus laparoscopic bile duct exploration during laparoscopic cholecystectomy in patients with choledocholithiasis. The results showed no difference between groups in terms of postoperative hospital stay, complications, or conversion in high risk patients. The laparoscopic approach was more effective and efficient, avoiding unnecessary invasive procedures [8].
For the treatment of small stones (<6 mm) detected by cholangiography during surgery, Masoni et al. [9], proposed dilation of the papilla through a transcystic catheter and subsequent irrigation with saline, which showed good results (96%) in bile duct clearance.
Common causes of conversion to open surgery during laparoscopic treatment of choledocholithiasis are Mirizzi’s syndrome and stones lodged in the papilla.
Dasari et al. [10], analyzing an expressive sample, compared endoscopic and laparoscopic bile duct clearance. The authors observed no significant difference in morbidity or mortality; however, there was a significant increase in retained stones in the endoscopic treatment (25%) compared to the laparoscopic approach (9%).
METHODS AND RESULTS
A total of 290 patients with cholelithiasis associated with choledocholithiasis, including 191 women (65.86%) and 99 men (34.14%), with a mean age of 58.4 years (21- 80), were treated using a single laparoscopic procedure.
Step-By-Step Procedure of Bile Duct Clearance
1) Pressure-washing with warm saline
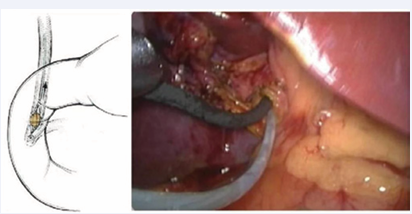
After compression of the bile duct at the level of the junction with the cystic duct with an aspirator, 20 ml warm saline is injected under pressure in an attempt to push the stone to the duodenum.The papilla is dilated with hyoscine and warm saline solution (Figure 1).
Figure 1 Removal of a gallstone using a basket under endoscopic guidance.
2) Dilation of the papilla
In the case of narrowing of the papilla, Levin tubes of progressively larger calibers (8, 10, 12 Fr) are passed to the duodenum, or the papilla is dilated with a Fogarty catheter. For the latter procedure, the catheter is inserted until reaching the duodenum and the balloon is inflated (1 ml),pulled to the papilla, deflated by half the volume of saline, and reinflated with saline in order to force dilation of the papilla. The two techniques are efficient and can be monitored by radioscopy and intermittent administration of saline through the tube into the bile duct and/ or duodenum.
The pressure-washing procedure can be repeated after dilation. It is important to note that the assistant should always compress the hepatic duct with the aspirator when fluid is injected under pressure into the bile duct, thus avoiding stones from migrating to the proximal bile duct and warm saline from flowing back to the portal system, causing bacteremia if bacteria are present in the bile.
These two simple procedures permit clearance of the bile duct in up to 20% of cases without the need for sophisticated devices or instruments.
3) Removal of gallstones through the cystic duct using a basket
Previous dilation of the cystic duct permits the passage of a basket and capture of smaller stones under radioscopic guidance (Figure 1).
4) Passage of the endoscope through the previously dilated cystic duct and capture of the stone with a basket under direct vision, or moving the gallstone with the tip of the endoscope or irrigation tube to the duodenum.
We have used a pediatric bronchoscope since it is more resistant and more durable, permitting good visualization of the proximal and distal bile duct under continuous saline irrigation. The ideal approach is to pass the bronchoscope through the entry of the subhepatic right hypochondrium, facilitating its placement inside the cystic and/or common bile duct and preventing angulation of the bronchoscope. These methods are feasible and reproducible in the medium term and are of low cost.Another limitation of the transcystic approach is the anatomic position, insertion and size of the cystic duct, which sometimes impairs bile duct clearance. At our institution, 46 (15.86%) cases were treated using methods 3 and 4 alone or in combination.
5) Choledochotomy
For choledochotomy, the anterior surface of the common bile duct should be dissected at the lowest level possible (juxtaduodenal). Only the anterior surface should be dissected, remembering that irrigation of the biliary tract is lateral (at 3 and 9 o’clock) and ischemia of the bile duct should be avoided. The injection of physiological saline into the bile duct facilitates identification for dissection and subsequent opening. The spontaneous exist of stones at the time of opening and in the presence of physiological saline in the bile duct is not uncommon. Pressure-washing can now be repeated with wider tubes. Since the common bile duct is open, stones may easily exit through the opening since the hepatic duct is closed by external compression of the aspirator at the junction of the hepatic duct with the cystic duct (Figure 1).
Another method, which is the most effective in our experience, is the use of a guided Fogarty catheter or a pediatric urinary catheter, which is less costly.
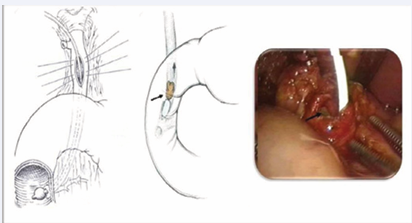
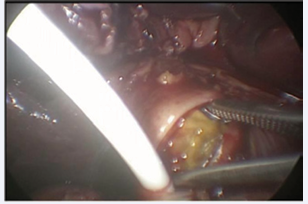
The tube is passed until the duodenum and the balloon is inflated, pulled to the papilla, deflated by half the volume, passed through the papilla, and reinflated, followed by pulling the Foley catheter. Usually, the balloon moves the stone until the opening of the common bile duct, which can then be removed by grasping or exits spontaneously (Figures 2,3).
Figure 2 Removal of a gallstone with a Fogarty catheter. Note the exit of the stone moved by the inflated balloon (arrow).
Figure 3 Removal of a gallstone with a Fogarty catheter. Note the exit of the stone moved by the inflated balloon and removed with grasping forceps.
In the present study, this method was the most effective, accounting for 58.61% of all cases.
All of these methods can be repeated in this sequence and are usually sufficient for good bile duct clearance. Good clearance needs to be confirmed by choledoscopy or intraoperative cholangiography.
We have used passage of the catheters through an opening in the right hypochondrium above the 5-mm puncture with the aid of a tentacannula. This approach permits to pass the tubes without losing the work ports or pneumoperitoneum.
Exceptionally, in our sample, metal tweezers such as those employed in open surgery can be used in 7% of cases, which are inserted through the same orifice as the catheters. The best metal tweezers are those with a greater curvature and lower angulation. The risk associated with their use is perforation of the bile duct, especially the posterior wall, with the formation of false passages. We had one case of perforation in our sample, which was identified by intraoperative endoscopy and treated only by drainage of the bile duct using T-Tube method after total bile duct clearance.
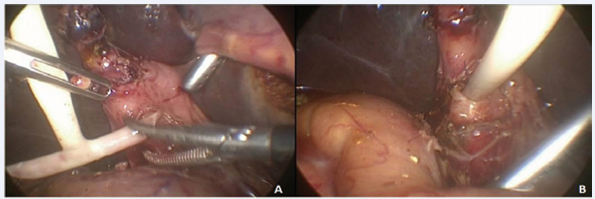
6) Choledochotomy and T-Tube drainage
We have routinely drained the bile duct after choledochotomy using a T-Tube drain as employed in open surgery and attached with 3.0 PDS at the site of cholangiography (Figure 4).
Figure 4 Note the placement of a fenestrated T-Tube drain (A). Note T-Tube drain in position and attached to the bile duct (B).
The drain is removed 3 weeks after cholangiography and confirmation of good bile duct clearance.
Among the 290 cases of choledocholithiasis treated by laparoscopy who required bile duct instrumentation, a transcystic approach under radioscopic guidance was used in 46 (16.86%) and choledoscopy through a choledochotomyin 244 (84.14%). Twenty-six (8.96%) of these cases required conversion to laparotomy. There was no case of death in this sample and complications were observed in 27 (9.31%) cases.
A biliary fistula characterized by the leakage of bile through the drain left in the subhepatic space, irrespective of volume and clinical presentation, was observed in 13 (4.48%) cases. In all cases, cholangiography confirmed that the leak was due to a closed biliary duct and/or around the drain. Treatment was clinical and the bile leak stopped within a mean period of 4 days in all cases (2-9).
Hyperamylasemia was detected in 11 (3.8%) cases and mild acute pancreatitis in 4 (1.38%). None of the patients developed severe complications and all of them improved with clinical treatment. In one case, intraoperative choledoscopy identified perforation of the posterior wall of the common bile duct after the use of metal tweezers for removal of a stone lodged in the papilla. After clearance, the bile duct was drained with a T-Tube tube and the patient improved without subsequent complications.
A choleperitoneum was observed in three cases (1.03%), which required a new laparoscopy and redrainage of the bile duct. In all cases, the choleperitoneum occurred after removal of the drain from the bile duct 3 weeks after surgery, two cases involved siliconized drains and one was a filled T-Tube drain.
Control cholangiography is performed before removal of T-Tube drain, which detected retained stones in seven (2.41%) cases. These cases were treated by smooth muscle relaxation and pressure-washing (n=2) or therapeutic endoscopy (n=5). Late complications were observed in six (2.07%) cases. A gallstone was detected by magnetic resonance cholangiography in four (1.38%) cases, which were treated by therapeutic endoscopy. Two cases developed bile duct stenosis. Good resolution was observed in one of these cases after dilation and biliary stenting. Recurrence of stenosis occurred in the other case, which required a biliodigestive anastomosis consisting of interposition of a jejunal tube (Monti Tube) [11-13] between the hepatic duct and duodenum. The patient showed satisfactory evolution after this procedure.
DISCUSSION
Since the advent of laparoscopic bile duct exploration, the treatment of choledocholithiasis has been a matter of much debate. Several methods exist for pre- or postoperative clearance of the common bile duct, such as endoscopy combined with laparoscopic cholecystectomy [14-17].
Our group trained in the laparotomy era continued to practice the same technical principles used in open surgery for the treatment of choledocholithiasis by the laparoscopic approach, i.e., to perform treatment in a single procedure, since the combination of laparoscopy and endoscopy increases complication rates, mortality and treatment costs. In the randomized study of Healy et al. [18] which compared 84 patients treated by a single procedure with 84 patients submitted to the combination of laparoscopic and endoscopic techniques, a significant increase in complications and treatment costs was observed for the combination of methods. However, in a metaanalysis, Li et al. [14] found that different combinations of endoscopic and laparoscopic methods were similar to the single procedure for the treatment of cholelithiasis associated with choledocholithiasis. The only difference was the shorter hospital length of stay in the group submitted to the single procedure.
In the present study, laparoscopic exploration of the bile duct was efficient in clearing the duct. Standardization of less invasive to more invasive techniques permitted clearance in 104 cases (35.86%) without the use of special instruments. The most efficient technique was the use of catheters with distal cuffs (Fogarty or urinary catheter), which permitted clearance in 169 cases (58.27%). Although the transcystic approach is less invasive than choledochotomy, the former is limited in the case of gallstones larger than 9 mm in diameter, terminal tapering of the common bile duct and multiple or intrahepatic stones, and considering the anatomical aspects of the cystic duct with its long, tortuous and thin trajectory. At our service, Tinoco et al. [19] reported excellent results of bile duct clearance with the preferential use of transcystic exploration. Several other authors also prefer choledochotomy for clearance of the common bile duct [20].
Endoscopy through the cystic or bile duct during common bile duct surgery is very useful for the removal of gallstones and mainly for the endoscopic confirmation of clearance.Studies comparing the use of fluoroscopy and choledochoscopy found no significant differences in complications, clearance rate or mortality. Only the length of surgery was greater in the group submitted to choledochoscopy. There are few studies reporting good results with the use of laser lithotripsy for common bile duct clearance [21].
In this study, drainage was performed in all cases through the cystic duct using a plastic catheter (No. 8 nasogastric tube) or preferentially through the bile duct using a rubber T-Tube drain. Several studies have shown that primary closure of the choledochotomy without external biliary drainage is a safe technique and that the results of long-term follow- up (48.8 months) are the same in terms of residual stones and bile duct stenosis [22-24].
Although several studies and some meta-analyses only found differences in the costs and length of hospital stay when the single procedure was compared to the combination of endoscopic clearance and laparoscopic cholecystectomy, longterm follow- up is still need to evaluate the consequences of mutilation of the sphincter of the papilla and of duodenogastric reflux resulting from the retrograde endoscopic approach to the bile duct. Furthermore, the training and preparation of the professional for safe execution of the procedure are less intensive and more reproducible for the single procedure compared to the endoscopic approach.
CONCLUSION
The results showed that treatment of choledocholithiasis in a single procedure through laparoscopic bile duct clearance is safe, reproducible and associated with a low rate of complications, in addition to preserving sphincter functions of the duodenal papilla.