Periprosthetic Fractures after Total Knee Arthroplasty (TKA): A Review of Literature from 1985 to 2006 with Clinical Commentry
- 1. Department of Orthopaedic and Trauma Surgery, ASL BARI, Italy
Abstract
Background: Periprosthetic fractures associated with total knee arthroplasty are becoming increasingly more common.
Methods, Results and Conclusions: The nature of the treatment of periprosthetic fractures depends on the localization, stability of the prosthesis and the condition of bone. Several classifications have proved to be of value in determinating specific modes of treatment. The current review analyses the different therapeutic options resulting in a concept of fracturespecific treatment.
The purpose of this article is to review general concepts about the management of fractures that occur adjacent in TKA, discuss various treatment options for the fractures, and provide some technical pearls about the procedures with a review of the rilevant literature. Numerous sound treatment strategies are available in the surgeon’ s arsenal with which to address these complex fractures. In this review, there are not outcomes and tables.
Keywords
Periprosthetic fractures after total knee arthroplasty; Risk factors; Classifications; Treatments; Review of literature from 1985 to 2006
Citation
Saccomanni B (2022) Periprosthetic Fractures after Total Knee Arthroplasty (TKA): A Review of Literature from 1985 to 2006 with Clinical Commentry. JSM Foot Ankle 4(1): 1052
KEY POINTS
Fractures of the distal femur, proximal tibia, and patella that occur adjacent to a total knee replacement may be very difficult to treat.
Fixation options are compromised because of the short articular segment, frequent comminution, pre-existing osteoporosis, previous surgical incisions, and the presence of the knee implant itself.
This review article summarizes current concepts regarding the epidemiology, classification, treatment options and outcomes for periprosthetic fractures of the knee.
INTRODUCTION
Little has been written on the subject of periprosthetic fractures following total knee arthroplasty. Despite this glaring difference, these two fractures entities share commonality with respect to classification principles and treatment options. Periprosthetic fractures after total knee arthroplasty are uncommon complications that are, however, difficult to treat effectively. Several therapeutic options and recommendations are described, but a fracture specific treatment, taking all the different therapeutic options into consideration, does not exist. The aim of the current review is to analyze current concepts regarding the epidemiology, classification, the results of the different therapeutic options resulting in a concept of fracture – specific treatment.
Similarly to fractures of the hip, periprosthetic fractures associated with total knee arthroplasty occur both intraoperatively and postoperatively. They can involve either the distal femur or proximal tibia. They are classified according to location, stability of the implant and surrounding bone quality. All of these factors are considered when discussing treatment options.
EPIDEMIOLOGY
The postoperative incidence of supracondylar femur fractures is 0,6% to 2,5 % [1].They generally occur within 10 years after surgery, usually secondary to relatively minor trauma [1]. Fracture of patella after total knee arthroplasty may occur, with prevalence of 0.1 % to 8.5 % [1].
The incidence of distal femur methaphyseal periprosthetic fractures associated with total knee arthroplasty has been reported to range between 0.3% and 2.5% [2-10]. In contrast, periprosthetic tibial fractures are much less common [11]. Similar to fractures about the hip, it is postulated that the rate of periprosthetic fractures of the knee is also increasing. Associated risk factors include the presence of osteopenic or osteoporotic bone, anterior femoral notching [12], and in the setting of revision arthroplasty [7], both osteolitysis and infection [8].
RISK FACTORS OF SUPRACONDYLAR FRACTURES
Supracondylar fractures after total knee replacement [1] are multifactorial in origin and risk factors [1] include:
- Osteoporosis;
- Preexisting neurologic disease;
- Notching of the anterior cortex:
Biomechanical analysis: 3 mm of anterior notching reduces torsional strength by 29 %.
- There is a high correlation between notching and supracondylar fractures in patients with rheumatic arthritis and significant osteopenia.
- In absence of significant osteopenia, there is no correlation between notching and supracondylar fractures [1].
Classification
Fractures involving either the distal femur or proximal tibia associated with knee replacement can also be classified [see 12 and 13] according to anatomic location, , timing of the fracture, stability of both the fractures and implant, and quality of the bone stock. Felix and coworkers [13], devised a comprehensive classification for periprosthetic tibia fractures, though quality of bone stock was not specifically addressed.
Supracondylar femur fractures Classification [1] Neer, with modification by Merkel
Type I: Minimally displaced supracondylar fracture
Type II: Displaced supracondylar fracture
Type III: Comminuted supracondylar fracture
Type IV: Fracture at the tip of the prosthetic femoral stem of fracture of the diaphysis above the prosthesis
Type V: Any Fracture of the tibia.
Periprosthetic femur fractures about total knees (Lewis and Rorabeck) [1]. This classification taken into account both fracture displacement and prosthesis stability
Type I: The fracture is nondisplaced, and the bone-prosthesis interface remains intact
Type II: The interface remains intact, but the fracture is displaced.
Type III: The patient has a loose or failing prosthesis in the presence of either a displaced or a nondiplaced fracture.
TREATMENT
Principles [1]
- Anatomic and mechanical aligment are critical.
- Nondisplaced fractures may be treated nonoperatively.
- ORIF is indicated if the alignment is unacceptable by closed means and if bone stock is adequate for fixational devices.
- If bone quality is poor, the fracture should be treated nonoperatively, despite poor aligment, with clinical and radiographic revalutation after healing.
- Immediate prosthetic revision is indicated in selected cases.
Nonoperative treatment
Long leg casting or cast bracing for 4 to 8 weeks may be used to treat minimally displaced fractures [1].
Operative treatment
-Displaced periprosthetic fractures around a total knee replacement are almost always managed with ORIF because of the difficulties in maintaining acceptable alignment after displacement [1].
- A blade plate, dynamic condylar screw, dynamic compression plate, condylar buttress plate, locked plate, or retrograde intramidullary nailing may be used for operative stabilization [1].
- Primary revision with a stemmed component may be considered if there is involvement of the bone- implant interface [1].
- Bone loss may addressed with autologous grafting [1].
- Cases of severe bone loss, especially in the methaphyseal region, may be addressed with distal femoral replacement, with a specialized prosthesis designed for oncology management [1].
-Fracture around the diaphysis or the tip of a femoral component may be treated with cortical struct grafts and cerclage wiring, dynamic compression plate, locked plate, or of a combination of techniques [1].
- Acceptable alignment guidelines [1] are:
- angulation from inferior 5 to 10° in either plane
- inferior 5 mm translation;
- inferior 1 cm shortening Tibial fractures [1]
RISK FACTORS
Risk factors [1] are:
- significant trauma (shaft fractures);
- tibial component malalignment associated with increased medial plateau-stress fractures;
- revision surgery with press-fit stress.
CLASSIFICATION
Periprosthetic tibial fractures (Felix et al) [1]
The classification is based on three factors: location of the fractures, stability of the implant, and whether the fracture occurred intraoperatively or postoperatively [1].
Type I: occur in the tibial plateau.
Type II: Adjacent to the stem
Type III: Distal to prosthesis
Type IV: involve the tubercle
The stability of the implant [1], is then used to classify the fractures further:
Subtype A is a well-fixed implant
Subtype B is loose
Subtype C fractures are intraoperative
TREATMENT
Nonoperative treatment
-Closed reduction and cast immobilization may be performed for most tibial shaft fractures after alignment is restored [1].
-Early conservation to a cast brace to preserve knee range of motion is adviced [1].
Operative Treatment
Periprosthetic tibial fractures not involving the plateau require ORIF if closed reduction and cast immobilization are unsuccessful [1].
Type I fractures involving the tibial plateau typically involve the bone-implant interface, necessitating revision of the tibial component [1].
PATELLA FRACTURES [1]
Epidemiology
The postoperative incidence is 0,3 % to 5,4% reported as high as 21% [1].
Risk factors
Risk factors [15] are Large, central peg component;
Excessive resection of the patella during prosthetic implantation
Lateral release, with devascularization of the patella Malalignment
Thermal necrosis (secondary to methylmethacrylate).
Classification
Goldberg [1]:
Type I: fractures not involding cement /implant composite or quadriceps mechanism;
Type II: fractures involving cement/ implant composite and / or quadriceps mechanism;
Type III A: Inferior pole fractures with patellar ligament distruption.
Type III B: inferior pole fractures without patellar ligament distruption.
Type IV: fracture-dislocations.
Treatment
Nonoperative treatment: Fractures without component loosening, extensor mechanism repture, or malignment of the implant (type I or IIIB) may be treated nonoperatively [1].
The patient may be placed in the knee immobilizer for 4 to 6 weeks, with partial weight bearing on the crutches [1].
Operative treatment: It is indicated for patients with distruption of the extensor mechanism, patellar dislocation or prosthetic loosening [15].
Treatment options [1] include: ORIF with revision of the prosthetic patella. This is indicated for type II, IIIA and IV fractures [1].
Fragment excision: this may be undertaken for small fragments that do not compromise implant stability or patellar tracking [15].
Patellectomy: this may be necessary in cases of extensive comminution or devascularization with osteonecrosis [1].
Surgical considerations include adequate medial arthrotomy, adequate lateral release, preservation of the superior lateral geniculate artery, and preservation of the patellar fat pad [15].
INTRAOPERATIVE FRACTURES OF THE FEMUR
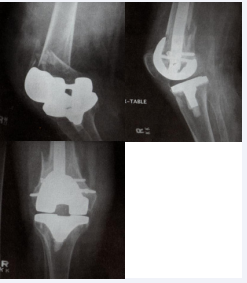
Fractures of the femur or identified intaoperatively often occur despite having adequate bone stock and include femoral condyle fractures, low transcondylar fractures, distal metaphyseal fractures and those that extent even proximally. Once identified, they must be judiciously treated with osteosynthesis by any number of treatment options. For displaced femoral condyle or transcondyle fractures and a stable implant, limited open reduction and internal fixation with screw fixation is often sufficient and can be augmented with protected weight-bearing postoperatively and careful monitoring of range of motion exercises postoperatively. Use of additional fixation devices such as plates is also reasonable. For distal methaphyseal fractures and those extending proximally, use of either a retrograde intramidullary nail (Figure 1),
Figure 1: Supracondylar periprosthetic femur fractures treated with retrograde intramedullary nailing
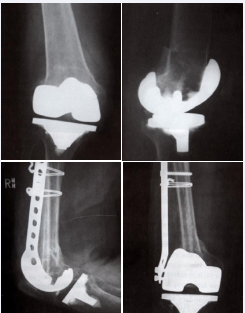
if permitted by an appropriately spacious and open intercondylar box, or fixed angled plate with or without allograft structs (Figure 2),
Figure 2: Supracondylar periprosthetic femur treated in a novel fashion with periarticular plate and intramedullary fibular struct allograft.
are both permissible assuming the implant is stable. If the femoral component is found to have become unstable in the process, then revision to a stemmed prosthetic and one perhaps greater constraint would be warranted.
POSTOPERATIVE FEMORAL FRACTURES
Fractures that occur postoperatively can occur secondary to injury or trauma, but are often a direct consequence of osteolytis and poor bone stock and may hence involve a loose prosthesis. In low-demand patients, conservative management such as the use of a hinged cast brace and restricted weight-bearing may be advocated if the fracture is found to be undisplaced and the component thought to be stable based on radiographic evidence. However, fractures warrant operative fixation. If the implant is stable, then osteosynthesis by any appropriate means would be raccomanded, and the addition of bone graft is warranted in cases of diminished bone stock. However, in cases of loose prosthetis, the prosthesis must be revised to a stemmed component, coupled with fracture fixation by screws, plate and cortical onlay struct allograft. The most difficult cases, however, involve a loose prosthesis coupled with deficient bone stock rendering a basic revision procedure impossible. In this regard, Kassab and coworkers [14], have described the use of a stemmed constrained revision component with structural distal femoral allograft composite as an effective means of providing both implant and fracture stability. Reconstruction of the distal femur with such a composite allows reattachment of host tissue, including specifically the collateral ligaments, which impart some additional stability to the knee postoperatively, thus circumventing the use of a hinged prosthetis. An alternative would be the use of a tumour megaprosthesis to reconstruct a deficient distal femur.
TIBIAL FRACTURES
Fractures of tibia identified intaoperatively are infrequent and rarely involve a loose prosthesis. In the low-demand patient, conservative management as described for fractures of the femur is possible, though operative fixation with either periarticular or buttress plates is often preferable.
Fractures identified postoperatively must be carefully assessed by radiographic means. If the implant is stable, then fracture fixation independent of the prosthesis is acceptable. If the prosthesis is loose, then revision to stemmed component is warranted, ensuring the fracture is bypassed by least 2 cortical diameters, and/or the fracture is independently treated with osteosynthesis. In cases of deficient bone stock, use of either a proximal tibial allograft with stemmed revision component composite or a tumour prosthesis are the only viable options.
CONCLUSION
Despite careful operative technique, the incidence of periprosthetic fractures of the knee continues to increase in direct response to ever-increasing numbers of total knee replacement performed around the world. As in all cases of a complex lower extremity reconstruction, meticulous soft tissue handling and judicious preoperative planning to ensure availability of all necessary components is imperative. Numerous sound treatment strategies are available in the surgeon’s arsenal with which to address these complex fractures.
REFERENCES
11.Healy WL. Tibia fractures below total knee arthroplasty. In: Insall JN, Scott WN, Scuderi GR Current concepts in primary and revision total knee arthroplasty. Lippincott-Raven Publishers, Philadelphia, 1996; 163-167.
13.Gross AE. Periprosthetic fractures of the knee: puzzle pieces. J Arthroplasty. 2004; 19: 47-50.