Blood Pressure (BP) Level and Urine Albumin Excretion (UAE) among Patients with Essential Hypertension Seen in the Primary Care Clinic of a Tertiary Hospital in South-West Nigeria
- 1. Federal Medical Centre, Abeokuta, Ogun state, Nigeria
- 2. Olabisi Onabanjo University Teaching Hospital, Sagamu, Ogun State, Nigeria
Abstract
Background: The detection of microalbuminuria (MAL) is a point of care test in primary care that indicates early kidney disease among patients with essential hypertension. Despite the strong prognosticating index of UAE in hypertension, there is a dearth of local studies at primary care setting that elucidate the relationship between UAE and BP level. The aim of the study was to assess the relationship between UAE and BP level in patients with essential hypertension attending a primary care clinic in South West Nigeria.
Methods: This was a cross-sectional hospital based study. Data were collected through a pre-tested interviewer administered questionnaire. Systematic random sampling technique was used in selecting 360 respondents with essential hypertension. They were screened for MAL using Micral Test strip- II from Roche Diagnostics. Statistical Package for Social Sciences (SPSS) version 17.0 was used to analyze data.
Results: The prevalence of MAL was 77.5%. BP was controlled in 24.7% of the respondents. Microalbuminuric respondents had higher mean BP compared to their normo-albuminuric counterparts (P<0.001). Urinary MAL was directly associated with age (P=0.02) and severity of hypertension according to JNC VII criteria (P=0.01).
Conclusions: The high prevalence of MAL in this study underscores the significance of screening for MAL in patients with essential hypertension at diagnosis and at intervals during therapy. This is particularly more important among those with uncontrolled BP and elderly patients. This will assist in risk stratification and appropriate management.
Keywords
• Essential hypertension
• Primary care clinic
• Blood pressure level
• Urine albumin excretion
• Microalbuminuria
Citation
Meeden IA, Joseph AA, Olukayode MS, Solomon OO (2018) Blood Pressure (BP) Level and Urine Albumin Excretion (UAE) among Patients with Essential Hypertension Seen in the Primary Care Clinic of a Tertiary Hospital in South-West Nigeria. J Family Med Community Health 5(2): 1148.
ABBREVIATIONS
BP: Blood Pressure; UAE: Urine Albumin Excretion; MAL: Microalbuminuria
INTRODUCTION
Hypertension is an important worldwide public health challenge [1]. It is estimated that nearly one billion people are affected by hypertension worldwide, and this figure is predicted to increase to 1.5 billion by the year 2025 [2]. In Nigeria, the prevalence of hypertension varied extensively between studies, ranging from a minimum of 12.4% to a maximum of 34.8% [3].
MAL which is defined as urinary albumin excretion (UAE) of 30-300mg/dl in 24 hours is frequently seen in patients with essential hypertension [4-7]. Therefore, detecting and monitoring the level of MAL in patients with essential hypertension is a desirable secondary preventive measure against severe renal and cardiovascular damage in these patients.
Cardiovascular morbidity and mortality as well as chronic kidney diseases are preventable if hypertensive nephropathy is detected at the microalbuminuric stage. There is overwhelmingly evidence that pharmacologic blockade of rennin-angiotensinaldosterone system (RAAS) by angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) provide effective reduction of MAL, blood pressure (BP), and long term prevention of adverse CV events beyond BP reduction [5-7].
Remarkably, despite the compelling evidence on the reversibility or delay of chronic kidney disease if detected at microalbuminuric stage [5-7], screening of patients with hypertension for microalbuminuria is not a routine practice in primary care in Nigeria. In addition, the dearth of local tudies conducted at primary care levels which assess the association between UAE and BP levels in patients with essential hypertension made it necessary to carry out this study. This study was aimed at determining the prevalence of MAL as well as finding out the relationship between UAE and blood pressure levels among patients with essential hypertension attending a primary care clinic.
MATERIALS AND METHODS
Study Setting
The study was carried out at General Outpatient Clinic (GOPC) of a tertiary hospital in South West, Nigeria. The hospital runs residency programme in Family Medicine, Obstetrics and Gynaecology, Paediatrics, Anaesthesia and Internal Medicine. The GOPC is run by the Department of Family Medicine and its annual attendance was 26,247 for the year 2016.
Study Design
This study was a hospital-based, cross-sectional descriptive study conducted on 360 adults aged 18 years and above who had essential hypertension. The estimated population per year based on the number of adult patients with essential hypertension (cases) that attended the GOPC in 2016 was 5,412.
Inclusion criteria
Patients aged 18 years and above with essential hypertension, either newly diagnosed or already on treatment attending GOPC of the hospital.
Exclusion criteria:
1. Patients with secondary hypertension.
2. Patients with other causes of proteinuria- urinary tract infection, chronic renal disease, congestive cardiac failure, diabetes mellitus, pregnancy, acute febrile illness and emergency conditions.
PATIENTS WITH MACROALBUMINURIA.
Sample size determination
The sample size (n) was calculated using the formula [8] n= z2 pq/d2 . At 95% confidence interval and a precision level of 5%, z=1.96 and d=0.05. The proportion of hypertensive patients with MAL (p) was 41% from previous study [9].Therefore, p=0.41 and q=1-0.41=0.59. Then, (n)=1.962 x0.41x0.59/0.052 =382.77
Since the number of patients with essential hypertension (N) that attended the GOPC in 2016 was 5,412 (less than 10,000), the sample size was adjusted by the formula; nf =n/ (1+n/N) [8]. Thus, nf=382.77/ (1+382.77/5,412)=357.48 which is approximately 360.
Sampling Technique
A systematic random sampling technique was utilized to select 360 hypertensive patients from the GOPC. The total number of adult patients with essential hypertension that attended the GOPC in 2016 was 5,412. This translated to a total of 1,353 hypertensive subjects in three months. Thus, a sampling interval of approximately 4 (1,353/360) was used. The first person was selected from the first four patients with essential hypertension arriving the clinic by simple random sampling (balloting) once at the outset of the study. Therefore, every consenting fourth person with essential hypertension who presented at the GOPC and met the selection criteria was enrolled in the study.
Data collection tool and process
The eligibility for the study was determined and consent was taken. Data were collected through interview using a pretested questionnaire. The pre-testing of the questionnaire was conducted on 30 hypertensive patients who were selected from the General outpatient clinic of the state General Hospital in the same study location. The necessary amendment was made on the questionnaire based on the outcome of the pre-test before it was finally adopted for the study.
The questionnaire consisted of various items including: Socio-demographic characteristics, Medical history, Physical Examination and Investigations (urine tests). It extracted information regarding patients’ demographic factors, social history, level of education and occupation. The age of the respondents were categorized into young (18-39 years), middle age (40-59 years) and elderly (≥60 years).
Blood pressure measurement for each subject was taken in the clinic using an Accosson® mercury sphygmomanometer after subjects had rested for five minutes. Systolic blood pressure and diastolic blood pressure were measured at Korotkoff phases I and V respectively.10 Blood pressure greater than or equal to 140/90mmHg was taken as hypertension.11 The BP of the respondents was further classified using the JNC VII staging [11]. Weight of the respondents was measured using Surgifriend Medicals’ standard weighing scale to the nearest 0.1kg according to standard protocol [12]. Height was measured with the stadiometer to the nearest centimeter according to standard protocol.12 Body mass index was then calculated using the formula BMI= Weight (kg)/Height2 (m2 ). BMI of respondents was categorized into normal range (18.5-24.9kg/m2 ), underweight (<18.5kg/m2 ), overweight (25.0-29.9kg/m2 ) and obesity (≥30kg/ m2 ) [12].
The waist and hip circumference were measured according to standard protocol [13]. Waist-hip ratio was calculated. Waist circumference of more than 40 inches (102cm) in men and greater than 35 inches (88cm) for women was considered abnormal. Also, a waist-hip ratio of greater than or equal to 0.90 in male and greater than or equal to 0.85 in female was considered abnormal [13].
Patients with fever and patients on medications that can raise microalbuminuria were excluded. Macroalbuminuria, glycosuria, micro-haematuria and evidence of UTI were also ruled out using the Combur-Test Strip. All patients whose urine samples were negative for these conditions mentioned above were then screened for microalbuminuria using Micral-Test strip according to manufacturer’s direction on the strip leaflets. MAL was said to be present when a urine sample produced a reaction colour corresponding to 20mg/L albumin (threshold for MAL) or more. The colour change ranges from white (MAL 100mg/L). The UAE status of respondents were categorized into MAL negative (MAL<20mg/L) and MAL positive (MAL ≥20mg/L).
Statistical analysis
Data were entered into the Statistical Package for Social Sciences (SPSS) version 17.0 programmes. Continuous variables were summarized as mean and standard deviations while categorical variables were summarized as percentages. Chi squared test was used to determine the association between the categorical variables. The difference between means was analyzed using t-test. All statistical tests were two-tailed and p-value < 0.05 was considered statistically significant.
Ethical consideration
Informed consent was also obtained from the respondents included in the study. Ethical approval was obtained from the Hospital Research Ethics Committee.
RESULTS
A total of four hundred and one (401) subjects were interviewed during the study but forty-one respondents had missing data. Three hundred and sixty respondents were recruited and their data were analyzed. This gave a completion rate of 89.8%.
The age range of the respondents was 25-107 years with a mean age of 57.24±12.17 years. There were more female [n=218 (60.6%)] than male [n=142 (39.4%)] respondents with male to female ratio of 1:1.5. Most of the respondents were elderly [n=176 (48.9%)] (Table 1).
Table 1: Socio-demographic characteristics of the respondents.
| Variables | Categories | Frequency (%) |
| Age in years categorized | 18-39 (Young) 40-59 (Middle-age) ≥ 60 (Elderly) |
27 (7.5) 157 (43.6) 176 (48.9) |
| Gender | Male Female |
142 (39.4) 218 (60.6) |
| Ethnicity | Yoruba Igbo Hausa Others |
322 (89.4) 24 (6.7) 1 (0.3) 13 (3.6) |
| Marital status | Single Married Separated / Divorce Widowed |
4(1.1) 235 (65.3) 37 (10.3) 84 (23.3) |
| Level of education | No formal education Primary Secondary Tertiary |
114 (31.7) 68(18.9) 62 (17.2) 116 (32.4) |
| Religion | Christianity Islam |
233 (64.7) 127 (35.3) |
| Occupation | Pensioner Unemployed Retired Artisan Trading Civil servant Professional Others |
67 (18.6) 18 (5.0) 8 (2.2) 27 (7.5) 128 (35.6) 34 (9.4) 32 (8.9) 46 (12.8) |
The mean SBP, mean DBP and mean MAP according to the age percentile were shown in Table 2.
Table 2: Mean blood pressure of respondents according to age in percentile.
| Blood pressure characteristics | Age in tenth percentile | ||||||||
| 25-34 years | 35-44 years | 45-54 years | 55-64 years | 65-74 years | 75-84 years | 85-94 years | 95-104 years | 105-114 years | |
| SBP | 138.2± 8.4 | 137.2±10.1 | 156.4±14.3 | 152.8±10.2 | 168.4±11.4 | 163.9±10.6 | 144.8±14.2 | 143.6±11.8 | 146.5±3.1 |
| DBP | 90.6±8.6 | 90.9±7.9 | 92.6±5.7 | 96.5±7.4 | 92.8±4.8 | 89.6±6.9 | 90.8±4.1 | 88.5±4.4 | 91.8±4.9 |
| MAP | 92.2± 7.6 | 95.9±8.7 | 101.3±10.4 | 98.4±10.8 | 116.3±13.8 | 113.0±16.2 | 98.6±7.4 | 99.8±8.2 | 100.3±10.4 |
| SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MAP: Mean Arterial Pressure | |||||||||
The mean systolic BP, mean diastolic BP and mean arterial pressure (MAP) of the patients in this study were 159.50+21.09, 92.38+12.85 and 113.16+18.89mmHg respectively. The mean BMI and mean WHR were 26.79±8.81 and 0.93±0.06 respectively.
The duration of HTN since diagnosis ranged between 6 months to 40 years. Majority of the respondents were diagnosed as having hypertension five years previously [n=256(71.1%)]. One hundred and twenty-three (34.1%) were overweight while 87 (24.2%) were in the obesity category. Eighty-nine (24.7%) of the patients had controlled BP (Table 3).
Table 3: Clinical characteristics of the respondents.
| Variables | Categories | Frequency (%) |
| Duration of hypertension ( years) | 0-5 6-10 ≥11 |
256 (71.1) 63 (17.5) 41 (11.4) |
| Body mass index | Underweight Normal Overweight Obesity |
13 (3.6) 137 (38.1) 123 (34.1) 87 (24.2) |
| Blood pressure control | Controlled Uncontrolled |
89 (24.7) 271 (75.3) |
| JNC VII classification of blood pressure of the respondents | Normal/ Pre-hypertension Stage 1 Stage 2 |
89 (24.7) 125 (34.7) 146 (40.6) |
| Current alcohol consumption | Yes No |
45 (12.5) 315 (87.5) |
| Currently smoking | Yes No |
10 (2.8) 350 (97.2) |
| Urine albumin excretion | MAL negative MAL positive |
81 (22.5) 279 (77.5) |
| Urine albumin excretion re-categorized | MAL negative 20-50mg/dl 51-100mg/dl >100mg/dl |
81 (22.5) 82 (22.8) 84 (23.3) 113 (31.4) |
| Consumption of herbal preparation | Yes No |
293 (81.4) 67 (18.6) |
| JNC: Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure | ||
A large proportion of the respondents had MAL in the urine [n=279(77.5%)] (Table 3 and Figure 1).
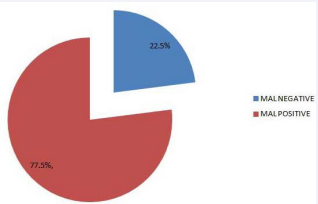
Figure 1 pattern of urine albumin excretion among the respondents MAL: Microalbuminuria.
There was direct association between the presence of MAL in respondents’ urine and their age, SBP, DBP and blood pressure level according to JNC VII. This was statistically significant when subjected to chi square test at P=0.02, P=0.002, P<0.001 and P=0.0013 respectively (Table 4,5).
Table 4: Relationship between microalbuminuria status and socio-demographic characteristics of the respondents.
| Variables | Categories | Urine albumin excretion status | X2 | P-value | |
| Micral Negative | Micral Positive | ||||
| Age | 18-45 ( Young) 45-64(Middle age) >65(elderly) |
19 (34.5%) 43 (22.3%) 19 (17.0%) |
36 (65.5%) 150 (77.7%) 93 (83.0%) |
6.51 | 0.022 |
| Gender | Male Female |
35 (24.1%) 46 (21.4%) |
110 (75.9%) 169 (78.6%) |
1.28 | 0.80 |
| Marital status | Single Married Separated / Divorce Widowed |
1 (25.0%) 57 (24.9%) 6 (16.2%) 17 (20.7%) |
3 (75.0)% 172 (75.1%) 31 (83.8%) 65 (79.3%) |
1.67 | 0.42 |
| Level of education | No formal education Primary Secondary Tertiary |
23 (19.8%) 16 (23.1%) 12 (18.8%) 30 (27.0%) |
93 (80.2%) 53 (76.9%) 52 (81.2%) 81 73.0%) |
2.31 | 0.62 |
Table 5: Relationship between urine albumin excretion status and clinical factors of the respondents.
| Variables | Categories | Micral test | X2 | P-value | |
| Negative | Positive | ||||
| Duration of hypertension ( years) | 0-5 6-10 ≥11 |
56 (21.9%) 13 (20.6%) 12 (29.3% |
200 (78.1%) 50 (79.4%) 29 (70.7%) |
1.28 | 0.57 |
| Body mass index | Underweight Normal Overweight Obesity |
2 (15.4%) 34 (24.8%) 28(22.8%) 17 (19.5%) |
11 (84.6%) 103 (75.2%) 95 (77.2%) 70 (80.5%) |
1.24 | 0.74 |
| Systolic blood pressure | Normal/ Prehypertension Stage 1 Stage 2 |
13 (39.4%) 36 (26.7%) 32 (16.7%) |
20 (60.6%) 99 (73.3%) 160 (83.3%) |
10.49 | 0.002 |
| Diastolic blood pressure | Normal/ Prehypertension Stage 1 Stage 2 |
29 (32.2%) 31 (25.2%) 21 (14.0%) |
61 (67.8%) 92 (74.8%) 129 (86.0%) |
11.56 | P< 0.001 |
| JNC VII classification of blood pressure of the respondents | Normal/ Prehypertension Stage 1 Stage 2 |
28 (31.8%) 30 (23.8%) 23 (15.8%) |
60(68.2%) 96 (76.2%) 123 (84.2%) |
8.25 | 0.01 |
| Current alcohol consumption | Yes No |
9 (20.0%) 72 (22.9%) |
36 (80.0%) 243 (77.1%) |
0.18 | 0.68 |
| Consumption of herbal preparation | Yes No | 61 (20.7%) 20 (30.8%) |
234(79.3%) 45 (69.2%) |
3.15 | 0.31 |
| JNC: Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure | |||||
Similarly, the mean MAP (mmHg), mean SBP (mmHg) and mean DBP (mmHg) of micral positive respondents were significantly higher than the corresponding measurements in micral negative respondents (P<0.001) Table 6.
Table 6: Mean difference of clinical characteristics between micral positive and micral negative respondents.
| Variable | Micral test | T | P-value | |
| Positive | Negative | |||
| WHR | 0.93±0.06 | 0.93±0.08 | 0.10 | 0.92 |
| BMI (kg/m2) | 26.84±5.76 | 26.52±4.18 | 0.45 | 0.65 |
| MAP (mmHg) | 116.18±0.78 | 109.04±1.61 | 4.69 | P< 0.001 |
| SBP (mmHg) | 161.52±1.26 | 151.47±2.09 | 4.11 | P< 0.001 |
| DBP (mmHg) | 93.51±0.75 | 87.82±1.38 | 3.61 | P< 0.001 |
| WHR: Waist-Hip Ratio; BMI: Body Mass Index; MAP: Mean Arterial Pressure; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure | ||||
DISCUSSION
The demographic distribution of participants in this study is skewed towards the elderly population as nearly half of them were over 60 years (48.9%). This observation is not in agreement with findings from most studies on hypertension where middle aged population were reported to be prevalent [14-16]. The observed difference may be explained by the age range of 25- 107 years reported in this present study. This is in contrast to previous studies where the upper level of the age range reported was a maximum of 90 years [14-16]. The varying age cut-off for different age groups used in different studies may also be responsible for this observation.
The prevalence of MAL in this study (77.5%) was high when compared with the prevalence reported in previous studies done over a decade ago which ranged between 5-40% [17-20]. As seen in this study, recent studies [9,21,22] have also reported a higher prevalence ranging between 41-71%. In the i- SEARCH global study conducted by Bohn and others in which 21,050 patients with hypertension were recruited at 1,750 centres from 26 countries, the overall prevalence was 58.4% [22]. Odili and others in Northern Nigeria also reported a MAL prevalence of 41% [9]. The wide variation in prevalence observed in both the old and recent studies may be largely attributed to the rising prevalence of hypertension and other cardiovascular diseases due to adoption of unhealthy lifestyle practices especially in developing countries.
The prevalence of MAL of 77.5% is high when compared with the prevalence rates reported in various recent studies above [9,21,22]. The higher prevalence in the present study may be attributed to the sample size of 360 respondents which is higher than sample size of less than 200 respondents in these studies [9,21]. Another possible explanation for the relatively high prevalence rate of MAL in this study could be attributed to the proportion of respondents with uncontrolled hypertension in this present study (75.3%). A large body of literature have demonstrated a direct association between MAL and uncontrolled hypertension [6,7,9,23,24]. The age distribution, presence of other cardiovascular diseases, study methodology and methods of determination of MAL are among other factors that can cause varied prevalence of MAL across and between studies [17,25].
The present study showed that less than one-third (24.7%) of the respondents had controlled blood pressure (BP). Suboptimal BP control is prevalent in Nigeria and most parts of the world [14,15,26-28]. Suboptimal control rates of 46.4% in an earlier study in South West Nigeria, [15] 24.2% in Port Harcourt South South, Nigeria [26] and 12.4% in Zaria Northern Nigeria [28] have been reported.
Age was significantly associated with UAE in the present study. The proportion of respondents who had positive MAL increased with age. The relationship between age and UAE is not clear. While this study agrees with some studies, [9,29] other studies have either reported an indirect relationship [30] or no association [31,32]. The variations may be adduced to confounders such as the severity of hypertension among the respondents and presence of other cardiovascular diseases.
Though the association between UAE and duration of hypertension was not statistically significant (P=0.568), an interesting finding in the study is that the proportion of respondents with positive micral test decreased as the duration of hypertension diagnosis lengthened. A possible explanation for this could be that most of the patients with hypertension may have died from more aggressive and earlier onset complications such as cerebrovascular disease and myocardial infarction. Therefore, the chances of dying from these complications may prevent them from reaching old age for MAL to be detected. A literature search on the association between UAE and duration of hypertension has not pointed in any specific direction. While some studies have reported no correlation/association between UAE and duration of hypertension, [31,32] other study have reported a direct relationship between UAE and duration of hypertension [30].
There was no relationship between MAL and gender. This finding agrees with the Odili and Olatunde studies in Nigeria where they also reported no association between UAE and gender [9,19]. On the contrary, Leocini et al., found male gender to be independently associated with MAL [33]. Generally, gender may not be an independent predictor of MAL. The unpredictable distribution of co-morbidities and uncontrolled hypertension across the two sexes in different studies may act as confounder.
The present study showed that MAL was directly associated with the severity of hypertension. It also found a statistically significant difference between the means of the SBP, DBP and MAP of micral positive and negative respondents (P<0.001). Similar to UAE and age, literatures on the relationship between UAE and BP have been conflicting [19,29-34]. The finding from this present study is in agreement with another study conducted by Massimo and others on 1567 adult patients with hypertension aged 45 to 64 years. They reported that isolated systolic blood pressure was significantly related to urinary albumin excretion and prevalence of MAL [29]. Contrary to this finding, Ogbu and others in South East Nigeria reported no significant difference in the mean SBP and DBP among MAL positive and MAL negative respondents in their study [32]. The observed difference may be adduced to the different study population, concomitant cardiovascular diseases and different methodologies.
There was no significant relationship between UAE and pulse pressure in this study. There are conflicting reports from studies on the association between UAE and pulse pressure. For instance, while the present study showed no association between UAE and pulse pressure, Massimo and others reported that pulse pressure is directly related to MAL independent of other correlates [29]. Pulse pressure which is calculated as systolic minus diastolic BP, tends to be more significant with high rate of isolated systolic HTN which is common in the elderly. Unlike in Massimo’s study where over 10% had systolic hypertension, [29] most of the respondents who were above 60 years of age in this study had both systolic and diastolic hypertension.
LIMITATIONS
The following limitations were considered in this study:
- The detection of MAL in the study was assessed using a semi-quantitative method (Micral test). Generally, the standard quantitative methods such as Radioimmunoassay (Gold standard), Laser immunonephelometry and Immunoturbidimetry have much higher specificity with greater reduction in false positive rate than the qualitative and semi-quantitative methods. Thus the prevalence could have been over-estimated.
- When the Micral test strip is used, two to three nonconsecutive urine samples have been recommended to increase the reliability of the result [7,35]. In this study, only one urine specimen was used in order to cut cost.
- Some of the patients that were labelled primary hypertensives might indeed have had secondary hypertension. This could have been avoided if facilities were readily available and affordable for extensive investigations.
- Lastly, the study was conducted in a health facility and cross-sectional in design. The inference drawn from the results should be taken with caution when comparing with community based survey.
CONCLUSION
It is concluded that the prevalence rate of microalbuminuria recorded in this study (77.5%) was high. The blood pressure control rate among patients with essential hypertension is still sub-optimal in this practice setting with the lowest control rate seen among the microalbuminuric respondents. UAE is directly associated with the age and severity of hypertension.
The high prevalence of microalbuminuria in this study demands establishment of a screening programme for microalbuminuria in primary care, implementation of specific interventions that focus on lifestyle modifications and education of patients with hypertension about the consequences of uncontrolled hypertension.
ACKNOWLEDGEMENT
We sincerely appreciate all our colleagues for their contributions during the preparation of this work.
REFERENCES
1. Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013; 311: 507-520.
9. Odili AN. Prevalence and clinical correlates of microalbuminuria in newly diagnosed hypertensive subjects. Nig J Med. 2008; 17: 452-456.
19. Olatunde LO, Arogundade FA, Balogun MO, Akinsola A. Microalbuminuria and its Clinical Correlates in essential hypertension. Nig J Health Sci. 2002; 2: 25-29.
20. Ulla D, Harald K, Christiana W, Andreas B, Harald H, Micheal MH. Comparing Microalbumin measurement alone with calculation of the albumin/creatine ratio for the screening of hypertensive patients. Nephrol Dial Transplant. 2002; 17: 81-85.






































































































































