Annals of Psychiatry and Mental Health
Volume 5 - Issue 6 Articles
-
ArticleJulianny Galdino Amorim Marinna de Andrade Saraiva Alberto Olavo Advincula Reis Maria Engracia Loiola Modesto Leite Rolim NetoDecember 16, 2017 | Pages : 205 - 450Abstract The story telling it has proven essential in improving patients who use the clinic, both in strengthening relations between doctor and patient, as in the understanding of the circumstances and acceptance of the sick; it is helpful in the healing .....
-
ArticleNovember 29, 2017 | Pages : 205 - 450Abstract Recently, Diagnostic and Statistical Manual of Mental Disorders (DSM-5) introduced social pragmatic communication disorder (SPCD) as a new neurodevelopmental communication disorder. There is a longstanding debate on the validity of this new commu.....
-
ArticleNovember 18, 2017 | Pages : 205 - 450Abstract It has been proposed that antisocial/borderline personality disorder (PD) might, for the purposes of classification, etiology and treatment, be considered as a single syndrome. This paper examines recent evidence relating to the epidemiology, pre.....

-
ArticleOctober 30, 2017 | Pages : 205 - 450Abstract Wernicke-Korsakoff Syndrome (WKS) results from a thiamine deficiency (vitamin B1) and is a debilitating, neurological disorder characterized by ocular abnormalities, mental health status changes, memory deficits, and ataxia.The implications of this.....

-
ArticleOctober 26, 2017 | Pages : 205 - 450Abstract Motivation and competence are both executive functions that are impaired in some ADHD patients. Based on a cross-sectional study of adult ADHD outpatients, we observed a correlation between personality dimensions (conscientiousness) and inattenti.....
-
ArticleOctober 21, 2017 | Pages : 205 - 450Abstract Women and men who conflict with exposed to gender roles and social norms are being alienated by society and experience various difficulties. The traditional use of social gender roles creates social inequality. Social inequality is the most impor.....
-
ArticleSeptember 29, 2017 | Pages : 205 - 450Abstract Bipolar disorder is a common, serious and recurrent disease with high morbidity, mortality and disability rates. Stigma is seen in bipolar disorder as it is in all mental illnesses. With stigmatization, patients can isolate themselves from societ.....
Volume 5 - Issue 5 Articles
-
ArticleSeptember 19, 2017 | Pages : 205 - 450Abstract Depression as a kind of mental illness affects huge number of population worldwide and is ranked as the fourth leading cause of disability worldwide, and is predicted to increase to the second place by 2020. Depression leads to great social burden .....
-
ArticleAugust 29, 2017 | Pages : 205 - 450Abstract Patients with conversion paralyses have the same disabilities and handicaps as patients with organic paralyses. Their treatment in physical medicine and rehabilitation is essential. Case study of four patients with conversion paralyses who have b.....
-
ArticleAugust 28, 2017 | Pages : 205 - 450Abstract Depression in older adults is a major public health problem that has received an inadequate response from medical professionals. Symptoms of depression can differ from those of younger adults and be related to cognitive changes, physical health p.....
-
ArticleAugust 05, 2017 | Pages : 205 - 450Abstract Objective: To investigate rates of shared decision-making experienced by patients treated for major depression in Australia, examining impacts of side effect profiles, efficacy profiles, and cost on agent selection. Methods: An anonymized online .....
-
ArticleJuly 21, 2017 | Pages : 205 - 450Abstract The current study presents a behavioral analysis of Israeli Prime Minister Benjamin Netanyahu and compares his behavior patterns at present with a previous study conducted in 1999.The analysis is based on the identification of recurring patterns o.....
Volume 5 - Issue 4 Articles
-
ArticleJuly 01, 2017 | Pages : 205 - 450Abstract This case reviews a patient with posttraumatic stress disorder, bipolar disorder and hypertension who experienced an acute decompensation in his mental health status while enrolled in our Veterans Treatment Court. The symptoms were attributed to h.....

-
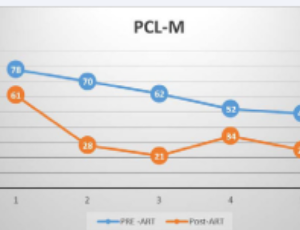
ArticleJune 29, 2017 | Pages : 205 - 450Abstract Purpose: To examine the use of Accelerated Resolution Therapy (ART) as an emerging, brief, non-invasive treatment for Military Sexual Assault-related Post-Traumatic Stress Disorder (MST-PTSD) including potential minimal dropout. Design: This was .....
-
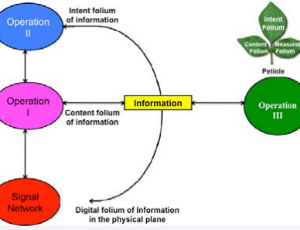
ArticleJune 17, 2017 | Pages : 205 - 450Abstract Bioinformatics of transition from signal to knowledge, experience and wisdom appears opaque. This transition has been described through four hierarchically nested specific operations to structurize the ladder of cognition. Cells could be classifi.....
-
ArticleJune 16, 2017 | Pages : 205 - 450Abstract Introduction: Mental illness is highly prevalent in the United States and approximately 43.8 million people experience mental illness in a year. The number of people seeking care for mental illness in the emergency department (ED) is increasing and.....
-
ArticleMay 25, 2017 | Pages : 205 - 450Abstract Objective: This study aims to review scientific literature about Mental Health Problems (MHP) in Indonesian population, especially children and important findings of the studies. Materials & methods: Two methods of searching were conducted; Englis.....
Volume 5 - Issue 3 Articles
-
ArticleMay 19, 2017 | Pages : 205 - 450Abstract This project evaluates the impact of having a psychiatrist present in the emergency department (ED) of a rural hospital that lacks a psychiatric unit. Using a mixed-method approach, a team of researchers examined hospital census data and surveyed.....
-
ArticleMay 05, 2017 | Pages : 205 - 450Abstract Attention-Deficit/Hyperactivity Disorder (ADHD), a disorder characterized by significant problems with attention, impulsiveness and excessive activity, is one of the most prevalent childhood psychiatric disorders and one of the most common reason.....
-
ArticleIlaria Matarazzo Federica Vellante Domenico Di Nicola Domenico De Berardis Alessandro Carano Matteo Lupi Gabriella Rapini Giovanni Martinotti Massimo di GiannantonioMay 04, 2017 | Pages : 205 - 450Abstract S.D. had a psychotic disruption after a prolonged period of apparent wellness. This disruption occurred after death of her psychotherapist. She presented bizarre delusion involving her body and her parents and she was mostly anxious. Her delusion.....
-
ArticleMay 04, 2017 | Pages : 205 - 450Abstract Bipolar disorder (BD) is a common psychiatric problem in youths and can pose a challenge in diagnosis in children and adolescents. The diagnosis of Youth Bipolar Disorders is complicated due to the various overlapping symptoms shared by other p.....
-
ArticleApril 07, 2017 | Pages : 205 - 450Abstract This study was to describe the prevalence of risky sexual behavior and identify correlates in Chinese adolescents. An anonymous self-reported survey was administered to 10,445 high-school students. The prevalence of having ever had sexual interco.....
Volume 5 - Issue 2 Articles
-
ArticleApril 06, 2017 | Pages : 205 - 450Abstract Suicidology is a social practice that sees itself as a science. Most of the research being done in suicidology draws from the positivist tradition. A key claim of the field is that over 90% of suicides have had a mental disorder. A new intellectu.....
-
ArticleApril 05, 2017 | Pages : 205 - 450Abstract n recent years, patient partnership has gained traction with regards to physical healthcare, while recovery has become the guiding principle of transformative action plans throughout the world, this time in terms of mental healthcare. Recovery-or.....
-
ArticleMarch 24, 2017 | Pages : 205 - 450Abstract Non-communicable chronic diseases including mental disorders contribute significantly to the world health burden according to World Health Organization (WHO). Common mental disorders, neurological diseases and HIV related mental disorders are u.....
-
ArticleMarch 21, 2017 | Pages : 205 - 450Abstract Intra-operative hypotension is generally responsive to decreasing anesthetic depth and/or intravenous fluid boluses. We present a 20-year-old male with multiple refractory intra-anesthetic hypotensive episodes, determined to have multifactorial .....
-
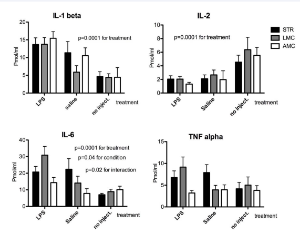
ArticleMarch 06, 2017 | Pages : 205 - 450Abstract Increased levels of pro-inflammatory cytokines and hypothalamic pituitary axis (HPA) activity are strongly associated with depression. Childhood stress and trauma predispose individuals for increased inflammatory tone and major depression in la.....
Volume 5 - Issue 1 Articles
-
ArticleFebruary 24, 2017 | Pages : 205 - 450Abstract Background: Psychotic major depressive disorder (PMDD) is complex with poor prognosis, reported in 15% to 25% of episodes with higher rates amongst older inpatients. There is little data on effective pharmacological treatment of PMDD. Method: A cr.....
-
ArticleFebruary 21, 2017 | Pages : 205 - 450Abstract A secondary analysis of data collected as part of the Massachusetts Youth Risk Behavior Survey was conducted to examine the association between gambling-related problems and the early onset of substance use among adolescents in grades 9-12. Hig.....

-
ArticleFebruary 07, 2017 | Pages : 205 - 450Abstract Addictive disorders are a significant complaint for referral to consultation-liaison (C-L) psychiatry services, as the C-L psychiatrist is specialized in consulting patients with general health conditions, as well as with psychosomatic disorders......
-
ArticleJanuary 27, 2017 | Pages : 205 - 450Abstract Studies have found a link between chronic stress and anxiety disorders as well as major depressive disorder. This article reviews literature based on that keeping in view the physiology of stress and its consequences on psychological well-being o.....
-
ArticleJanuary 19, 2017 | Pages : 205 - 450Abstract Purpose: The authors studied the impact of smoking on relapses in schizophrenics. Method: A lot of 134 schizophrenics diagnosed according to the ICD 10 was used. We looked into the number of cigarettes, association with other legal drugs, sex, p.....

Browse by Year
Author Information
X
Subscribe to Newsletters
And stay informed about our news and events