Management of Acquired Tracheoesophageal Fistula and Complete Pharyngoesophageal Stenosis as a Complication of COVID-19
- 1. Thyroid, Head and Neck Cancer (THANC) Foundation, USA
- 2. Department of Otolaryngology-Head and Neck Surgery, Icahn School of Medicine at Mount Sinai, USA
ABSTRACT
Background: Many patients experiencing severe symptoms of COVID-19 require critical care involving intubation, tracheostomy, and mechanical ventilation. These treatment interventions can result in life-threatening consequences.
Methods: We report a case demonstrating severe complications of COVID-19 and prolonged intubation. This patient developed a tracheoesophageal fistula (TEF) and complete pharyngoesophageal stenosis (PES). We detail the novel operative repair of this complex injury and review the literature regarding iatrogenic airway-injuries experienced by COVID-19 patients after prolonged intubation and mechanical ventilation.
Results: Following a year of G-tube dependence and unsuccessful attempts at repair, our patient underwent successful surgical reconstruction via tracheal resection and esophageal reconstruction with a radial forearm free flap. Two months post-operatively, the patient has a stable airway and maintains his weight by oral nutrition.
Conclusions: Head and neck surgeons must be well-versed in techniques for upper aerodigestive restoration amidst this unprecedented rise in intubation-related injuries associated with the COVID-19 pandemic.
KEYWORDS
• Tracheoesophageal fistula
• Pharyngoesophageal stenosis
• COVID-19
• Prolonged intubation
• Surgical reconstruction
CITATION
Greenberg LA, Wein LE, Dowling E, Urken ML (2022) Management of Acquired Tracheoesophageal Fistula and Complete Pharyngoesophageal Stenosis as a Complication of COVID-19. Ann Otolaryngol Rhinol 9(5): 1300.
ABBREVIATIONS
ARDS: Acute Respiratory Distress Syndrome; IMV: Invasive Mechanical Ventilation; TEF: Tracheoesophageal Fistula; PES: Pharyngoesophageal Stenosis
INTRODUCTION
The World Health Organization has reported upwards of 511 million confirmed cases of COVID-19 infections worldwide as of May 3rd, 2022 [1]. In most patients, the disease presents in a mild form with symptoms including fever, cough, nausea, vomiting and diarrhea [2,3]. However, severe complications of this disease have emerged. These include multifocal pneumonia, acute respiratory distress syndrome (ARDS), severe hypoxemic respiratory failure, and thromboembolic events [2-4]. Although rates of patients requiring critical care are low, ranging from 5% to 12%, intensive care units have been overwhelmed as a result of the high transmissibility and sheer number of COVID-19 cases [2,3,5,6].
Use of invasive mechanical ventilation (IMV) via intubation and tracheostomy to treat severe cases of COVID-19 have resulted in an array of complications, including laryngotracheal granulomas, webs, stenosis, and malacia. Less frequently, fullthickness tracheal necrosis and tracheoesophageal fistulae (TEFs) have been reported as complications [3]. Though rare, these serious conditions can be life threatening due to airway obstruction, tracheobronchial contamination and impaired deglutition, requiring alternative routes of enteral nutrition.
Herein, we review the challenge of increasingly prevalent COVID-19-related upper aerodigestive tract complications and present a case of iatrogenic TEF with complete pharyngoesophageal stenosis (PES) treated with a novel operative technique.
METHODS
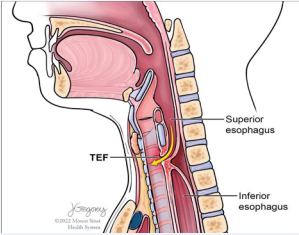
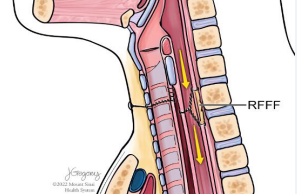
We review the case of a patient who presented to our institution after experiencing severe multisystem complications resulting from prolonged hospitalization for a COVID-19 infection that lasted for over 12 months. The patient developed a TEF with complete PES (Figure 1).
Figure 1: Illustration of the tracheoesophageal fistula with complete pharyngoesophageal stenosis in the case presented.
Multiple attempts to repair the fistula were carried out unsuccessfully at outside institutions. We outline the novel operative technique ultimately performed to successfully repair the patient’s fistula and restore oral nutrition.
CASE PRESENTATION
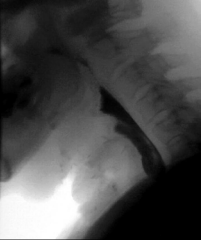
A 52-year-old male presented with a TEF more than 1.5 years following hospitalization for a severe COVID-19 infection. During this time, he required intubation and IMV for 69 days due to ARDS. His hospital course was complicated by two cardiac arrests, stroke, acute kidney injury requiring dialysis, osteomyelitis of the cervical spine, and sacral decubitus ulcers requiring colostomy diversion. Tracheostomy was performed and the patient was ultimately weaned from IMV. He made a significant recovery, but subsequently developed poor oral intake, chronic vomiting, and weight loss of 113 pounds. The patient was unable to swallow saliva and was completely dependent on his gastrostomy tube for nutrition. A modified barium swallow demonstrated a TEF with complete PES (Figure 2).
Figure 2: Modified barium swallow showing tracheoesophageal fistula with complete pharyngoesophageal stenosis and demonstrating aspiration of the entire bolus.
Multiple prior attempts to repair the fistula, including esophageal stent placement, rendezvous procedures (Figure 3),
Figure 3: Fluoroscopic image from a prior unsuccessful rendezvous procedure, indicating the location of the stenosis and the ability to perform the entire surgery through a transcervical approach.
and reconstruction with a pectoralis major myofascial flap were unsuccessful. Nearly two years after the initial COVID-19 diagnosis, the patient presented to our institution for consultation. Surgical repair was ultimately performed using a novel technique including tracheal division and esophageal reconstruction with a radial forearm free flap.
Operative technique
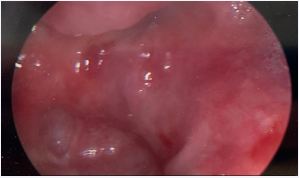
At the onset of the procedure, direct laryngoscopy, esophagoscopy, and retrograde esophagoscopy were performed to identify the location of the fistula and the site and extent of the PES. The TEF was identified immediately distal to the cricoid cartilage and was approximately 4 millimeters in diameter. The proximal and distal esophageal segments both ended in blind pouches with approximately 2 centimeters of complete stenosis between them (Figure 4).
Figure 4: Retrograde esophagoscopy demonstrating a blind pouch at the proximal extent of the distal esophageal segment, consistent with complete esophageal stenosis.
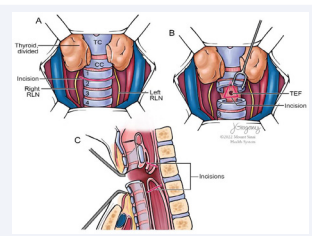
Retrograde esophagoscopy confirmed that the cervical esophagus was normal above the level of the clavicles and could be accessed through a transcervical approach. Once the location and extent of the injury was confirmed, we proceeded with open repair of the TEF and resection of the PES with reconstruction. A midline approach was used to access the anterior tracheal wall. The strap muscles were separated and retracted laterally to expose the central compartment. The recurrent laryngeal nerves were identified and lateralized from the tracheoesophageal groove. This was done with continuous neuromonitoring to ensure preservation of vocal cord function. The thyroid gland was divided in the midline and retracted laterally to expose the anterior trachea (Figure 5A).
Figure 5: (A) The recurrent laryngeal nerves were lateralized and the thyroid gland was divided at the midline to expose the anterior tracheal wall. (B) A transverse tracheotomy was performed and a wedge of tissue incorporating the tracheoesophageal fistula was resected from the posterior tracheal wall. (C) The pharyngoesophageal segments proximal and distal to the site of stenosis were incised to expose a favorable caliber of the proximal and distal esophageal segments.
The trachea was entered at the approximate level of the TEF. Once the location of the TEF was confirmed, just distal to the cricoid cartilage, the trachea was transected at this level and the TEF was exposed and excised (Figure 5B). Direct repair of the tracheal component of the TEF was accomplished with mattress sutures.
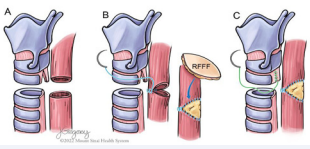
Entry into the proximal esophageal segment was then performed and the margins of the TEF were freshened (Figure 5C). The distal blind pouch of the esophagus was identified and mobilized while protecting the recurrent laryngeal nerves bilaterally. Entry into the distal esophagus demonstrated a normal caliber of the lumen. At this point, both the trachea and esophagus were in discontinuity (Figure 6A).
Figure 6: (A) After resection of the tracheoesophageal fistula, both the trachea and esophagus were discontinuous. (B) After mobilizing the distal esophageal segment, a tension free repair of the anterior wall of the distal esophageal segment was approximated to the postcricoid mucosa. The remaining defect in the posterior esophageal wall could not be repaired without tension and was reconstructed with a radial forearm free flap. (C) The wedge defect in the posterior tracheal wall was closed vertically and did not lead to narrowing the tracheal lumen.
Through mobilization of the distal esophagus, a tension free approximation of the anterior cervical esophagus to the postcricoid mucosa was then accomplished, achieving closure of approximately 180 degrees of the cervical esophageal lumen. A radial forearm free flap was harvested for reconstruction of the remaining defect in the posterior esophageal wall (Figure 6B). A separate skin paddle of the radial forearm flap was incorporated into a suture line in the neck for postoperative microvascular monitoring.
Once the esophageal reconstruction was completed and the flap revascularized, closure of the trachea was performed. Direct repair of the tracheal component of the TEF was accomplished with mattress sutures (Figure 6C). Primary anastomosis of the trachea was performed without tension (Figure 7).
Figure 7: The tracheal segments were reapproximated with a tension-free closure. Revascularization of the radial forearm flap and exteriorization of a proximal monitor paddle led to completion of the reconstruction.
The patient remained intubated overnight with the cuff of the endotracheal tube distal to the suture line. Uneventful extubation was performed the following day in the intensive care unit. The patient remained nil per os for one week and restarted an oral diet once a modified barium swallow confirmed patency of the reconstruction without evidence of a leak (Figure 8).
Figure 8: Postoperative modified barium swallow showing a widely patent pharyngoesophageal reconstruction without evidence of a leak or fistula.
At 2 months follow-up, the patient tolerated a diet of soft solids. Swallowing assessment showed marked improvement with a widely patent pharyngoesophageal segment and closure of the TEF. The patient will continue to advance his diet as tolerated with the goal of removing his gastrostomy tube.
The patient underwent reversal of his colostomy at 2 months following TEF repair in order to restore continuity of his entire alimentary tract. At that time, tracheoscopy demonstrated a wellhealed posterior tracheal wall and a widely patient airway.
DISCUSSION
Acquired tracheoesophageal fistula is a rare complication most commonly related to prolonged IMV via endotracheal intubation or tracheostomy [7,8]. Couraud and colleagues reported tracheal and esophageal erosion in 0.3-3% of mechanically ventilated patients [7]. Laryngotracheal injury in the context of intubation has several known risk factors. High cuff pressure, high airway pressure, tube mobility, inappropriately large endotracheal tube, and prolonged intubation are risk factors related to intubation itself [9,10]. Additional risk factors include immunosuppression, hypotension, respiratory or esophageal infection, and use of a nasogastric tube [9-11].
The COVID-19 pandemic has resulted in an unprecedented increase in iatrogenic intubation-related laryngotracheal injuries due to both the volume of COVID-19 patients in the ICU who require IMV as well as the prolonged duration for which it is required [3]. Guan et al. reviewed 1,099 patients from 552 hospitals in China with confirmed COVID-19 cases between December, 2019 and January 2020. Ninety-one percent of these patients were diagnosed with pneumonia, with 3.4% progressing to ARDS [2]. Treatment of ARDS often involved prolonged mechanical ventilation with high peak pressures [12]. In another analysis of 1,591 patients referred for ICU admission within the COVID-19 Lombardy ICU Network, 88% required IMV [13]. Another study found that the median length of IMV was 10 days [13].
Tracheostomy is indicated for patients with severe cases of COVID-19 requiring prolonged mechanical ventilation [12]. Studies prior to COVID-19 have demonstrated the efficacy of early tracheostomy placement as opposed to long-term intubation in patients requiring IMV [3]. More specifically, tracheostomy placement within 1-2 weeks of intubation has shown significantly better outcomes than later tracheostomy with regard to weaning from IMV, complications, and mortality [3]. Unfortunately, patients with COVID-19 are often intubated for more prolonged periods due to a variety of clinical practice protocols including confirmation of viral load clearance and cessation of prone positioning prior to tracheostomy [3].
The rationale for confirmation of viral load clearance is to diminish the risk of COVID-19 transmission to healthcare workers performing the tracheostomy, which is recognized as a highly aerosol-generating procedure [14]. In a study comparing international perioperative care protocols in 26 countries for patients with COVID-19, Bier-Laning and colleagues found that the majority of protocols directly addressing perioperative COVID-19 testing recommended delaying tracheostomy until obtaining a negative COVID-19 test [15]. These protocols often extended intubation time to 3-4 weeks or more [3]. Alternatively, there was pressure to perform tracheostomies in this patient population due to the sheer number of COVID-19 patients requiring critical care compared to the limited availability of ventilators and ICU beds in an effort to reduce the duration of patient stays in the ICU [12].
Regarding the postponement of tracheostomies to prevent coronavirus transmission, Rosano and colleagues found that only 7 out of 91 doctors and nurses (7.7%) involved in early percutaneous tracheostomies acquired COVID-19, compared to 6 out of 52 healthcare workers (11.5%) with no prior involvement in tracheostomies [16]. This data suggests that delaying tracheostomies does not necessarily result in added protection for the associated healthcare team.
Furthermore, Fiacchini and colleagues performed a study comparing the incidence of intubation-related tracheal complications in patients with and without COVID-19. This study demonstrated that significantly more patients with COVID-19 undergoing prolonged intubation suffered from fullthickness tracheal injuries or tracheoesophageal fistulae than matched controls without COVID-19 (46.7% compared to 2.2%) [17]. These results emphasize the increased risk of prolonged intubation for patients with COVID-19. The authors proposed several hypotheses regarding airway injury specific to the pathophysiology and management of severe COVID-19. The tracheal mucosa harbors actively replicating COVID-19 viruses, which can theoretically weaken the mucosa. In severe cases, COVID-19 can also produce a prothrombotic and antifibrinolytic state which results in microvascular injury and can potentially lead to necrosis of the tracheal and esophageal mucosa [17]. In addition, severe COVID-19 infections are often treated with high doses of systemic steroids which can contribute to mucosal atrophy and alteration of normal healing processes [17]. Another contributing factor is the use of pronation maneuvers to improve ventilation in COVID-19 patients with severe respiratory compromise. This position introduces significant pressure of the endotracheal tube against the tracheal wall. This pressure is also transmitted to the esophagus, especially when a rigid orogastric or nasogastric tube is in place. Additionally, Fiacchini et al., found that the ratio of partial pressure of arterial oxygen to fraction of inspired oxygen was lower for COVID-19 patients compared to matched controls, which can result in hypoxic injury to the tracheal mucosa [17]. This constellation of factors is thought to contribute to the rise in iatrogenic airway sequelae from severe COVID-19 infections.
Tracheoesophageal fistulae can be life threatening as a result of dyspnea, tracheobronchial contamination, and impaired nutrition [18]. Pharyngoesophageal stenosis occurring simultaneously with tracheoesophageal fistulae has been reported in the literature [19-24]. The patient presented in this paper required surgical repair of both a tracheoesophageal fistula and complete PES. Concurrent tracheoesophageal fistulae and stenosis required additional surgical considerations, especially in light of having an intact larynx [20]. Early identification and continued protection of the recurrent laryngeal nerves is a critical step for functional success.
Proliferating evidence linking COVID-19 to iatrogenic airway injuries substantiates the need for multidisciplinary follow-up care of COVID-19 survivors [3]. Maintaining a low threshold of suspicion for intubation-related airway injuries and increasing awareness of subclinical symptoms associated with this diagnosis is necessary. Furthermore, head and neck surgeons should be familiar with existing techniques to correct these complications. An individualized approach is needed to optimally treat upper aerodigestive tract injuries depending on the specifics of their location and nature.
CONCLUSION
COVID-19 has contributed to an unprecedented rise in iatrogenic upper aerodigestive tract injuries. While most injuries are minor, serious complications such as TEFs have occurred at an alarming rate. Herein, we present the case of a patient with a TEF with complete PES secondary to COVID-19-related complications reconstructed with a novel surgical technique.
REFERENCES
- WHO Coronavirus (COVID-19) Dashboard: World Health Organization;2022.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 382: 1708-20.
- Piazza C, Filauro M, Dikkers FG, Nouraei SAR, Sandu K, Sittel C, et al. Long-term intubation and high rate of tracheostomy in COVID-19 patients might determine an unprecedented increase of airway stenoses: a call to action from the European Laryngological Society. Eur Arch Otorhinolaryngol. 2021; 78: 1-7.
- Ribes A, Vardon-Bounes F, Memier V, Poette M, Au-Duong J, Garcia C, et al. Thromboembolic events and Covid-19. Adv Biol Regul. 2020; 77: 100735.
- Kowalski LP, Sanabria A, Ridge JA, Ng WT, de Bree R, Rinaldo A, et al. COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020; 42: 1259-67.
- Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, et al. Intensive care management of coronavirus disease 2019 (COVID-19). challenges and recommendations. Lancet Respir Med. 2020; 8: 506-17.
- Couraud L, Ballester MJ, Delaisement C. Acquired tracheoesophageal fistula and its management. Semin Thorac Cardiovasc Surg. 1996; 8: 392-9.
- Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003; 13: 271-89.
- Wolf M, Yellin A, Talmi YP, Segal E, Faibel M, Kronenberg J. Acquired tracheoesophageal fistula in critically ill patients. Ann Otol Rhinol Laryngol. 2000; 109: 731-5.
- Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994; 111: 453-9.
- Pacheco-Lopez PC, Berkow LC, Hillel AT, Akst LM. Complications of airway management. Respir Care. 2014; 59: 1006-19.
- Caputo MP, Aziz S, Mifsud M. Early Tracheostomy in Morbidly Obese COVID-19 Patients: A Case Series and Discussion of Institutional Practices. Cureus. 2021; 13: e14345.
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020; 323: 1574-81.
- Delides A, Maragoudakis P, Nikolopoulos T. Timing of Tracheotomy in Intubated Patients With COVID-19. Otolaryngol Head Neck Surg. 2020; 163: 328-9.
- Bier-Laning C, Cramer JD, Roy S, Palmieri PA, Amin A, Anon JM, et al. Tracheostomy During the COVID-19 Pandemic: Comparison of International Perioperative Care Protocols and Practices in 26 Countries. Otolaryngol Head Neck Surg. 2021; 164: 1136-47.
- Rosano A, Martinelli E, Fusina F, Albani F, Caserta R, Morandi A, et al. Early Percutaneous Tracheostomy in Coronavirus Disease 2019: Association With Hospital Mortality and Factors Associated With Removal of Tracheostomy Tube at ICU Discharge. A Cohort Study on 121 Patients. Crit Care Med. 2021; 49: 261-70.
- Fiacchini G, Trico D, Ribechini A, Forfori F, Brogi E, Lucchi M, et al. Evaluation of the Incidence and Potential Mechanisms of Tracheal Complications in Patients With COVID-19. JAMA Otolaryngol Head Neck Surg. 2021; 147: 70-6.
- Chauhan SS, Long JD. Management of Tracheoesophageal Fistulas in Adults. Curr Treat Options Gastroenterol. 2004; 7: 31-40.
- Thomas AN. The diagnosis and treatment of tracheoesophageal fistula caused by cuffed tracheal tubes. J Thorac Cardiovasc Surg. 1973; 65: 612-9.
- Marzelle J, Dartevelle P, Khalife J, Rojas-Miranda A, Chapelier A, Levasseur P. Surgical management of acquired post-intubation tracheo-oesophageal fistulas: 27 patients. Eur J Cardiothorac Surg. 1989; 3: 499-502.
- Bibas BJ, Cardoso PFG, Minamoto H, Pego-Fernandes PM. Surgery for intrathoracic tracheoesophageal and bronchoesophageal fistula. Ann Transl Med. 2018; 6: 210.
- Poissonnet V, Culie D, Rouanet C, Bozec A. Tracheoesophageal fistula and pharyngoesophageal stenosis repair by double skin paddle radial forearm flap. Eur Ann Otorhinolaryngol Head Neck Dis. 2021.
- Machado RA, Moubayed SP, Urken ML. Repair of pharyngoesophageal stenosis and a tracheoesophageal fistula using a dual-paddled radial forearm free flap: Flap design and surgical technique. Laryngoscope. 2017; 127: 2081-4.
- Calvo Medina V, Galan Gil G, Sales Badia G, Morcillo Aixela A, Garcia Zarza A, Tarrazona Hervas V, et al. [Benign acquired tracheoesophageal fistulas]. Arch Bronconeumol. 1997; 33: 577-81.