Is Thyroid Volume a New Prognostic Factor for Voice Outcome in Patients Without Vocal Fold Immobility After Thyroidectomy?
- 1. Department of Otorhinolaryngology, Hospital da Luz, Portugal
- 2. Department of Otorhinolaryngology, Mayo Clinic Arizona, USA
- 3. Department of Otorhinolaryngology, Hospital da Luz, Portugal
- 4. Thyroid Center, Hospital da Luz, Portugal
- 5. Oncology Institute Francisco Gentil, CiiEM – Egas Moniz Interdisciplinary Research Center, Portugal
- 6. Department of Otorhinolaryngology, Hospital da Luz, Portugal
ABSTRACT
Introduction: Thyroid pathology evolves slowly but its surgery suddenly modifies structures of vocal tract, what may elicit short and long-term voice changes in these patients, even when vocal fold mobility is not compromised.
Objective: The objective of this study was to analyze possible prognostic significance of thyroid specimen volume in long term voice outcomes of patients without vocal fold immobility after thyroidectomy.
Methods: Prospective cohort study of long-term vocal function and single blinded laryngoscopy results in patients without post-thyroidectomy vocal fold immobility. Correlation was assessed between voice outcomes and thyroid specimen volume over a one-year period time frame.
Results: A total of 90 patients were preparing to undergo a thyroidectomy and were enrolled in the study. In 84 patients without post-operative vocal fold immobility, perceived dysphonia increased in the first post-operative month, but it decreased to a level inferior to pre-operative evaluation after one year. LS functional changes decreased in the first post-operative month, but then increased at 3 months followed by a reduction compared to pre-operative results one year after surgery. GRBAS – G revealed a twofold increase of dysphonia in the first post-operative month, followed by a decrease comparing favorably to pre-operative results at one year. VHI- Fi subscore changes parallel that of GRBAS-G, as does f0 /a/ and HP f0 /i/ changes. HP f0 /i/ reveals a frequency reduction one month after surgery and it does not recover pre-operative mean frequency after one year. Correlation was established between dysphonia, surgical specimen weight and echographic thyroid volume. Correlation was also established for dysphonia, F0 /a/ change and HP f 0 /i/ reduction (mean 60Hz) with p<0.01 significance at one year.
Conclusions: Voice changes in patients without post-thyroidectomy vocal fold immobility involve F0/a/ change and HP f 0 /i/ reduction (mean 60Hz). These voice changes are related to thyroid volume and weight which, in turn, are correlated to echographic pre-operative thyroid volume. Increased echographic thryoid volume should be considered a prognostic factor for vocal compromise after thyroid surgery.
CITATION
Viana Baptista SIR, Lott DG, Almeida SCC, Cid MO, Zagalo C, et al. (2022) Is Thyroid Volume a New Prognostic Factor for Voice Outcome in Patients Without Vocal Fold Immobility After Thyroidectomy? Ann Otolaryngol Rhinol 9(4): 1296.
INTRODUCTION
Over the past ten years, voice outcomes in thyroid surgery have become of central importance in thyroid surgery. The American Academy of Otolaryngology Head and Neck Surgery (AAO-HNS) Foundation’s Clinical Practice Guideline on improving Voice Outcomes after Thyroid Surgery from June 2013 [1] recommended, among others, that patients receive a preoperative laryngeal examination if the voice is impaired or in the setting of a normal voice with suspected extrathyroidal extension. These guidelines were questioned by an editorial in Surgery in April 2014 [2], where a panel of general surgeons wrote that those guidelines were inadequate because they overstate vocal dysfunction in thyroid surgery and induce anxiety in patients.
Since 2010, international research on intraoperative recurrent laryngeal nerve neuromonitoring has received high interest and has resulted in the best practice recommendation to routinely use neuromonitoring in thyroid surgery [3-9]. The importance of routinely using intraoperative laryngeal nerve neuromonitoring cannot be overstated (not only on a clinical basis but also in malpractice defense). However, even though its use is recommended by AAO-HNS and the European Laryngology Academy, many surgeons still do not have routine access to this complimentary tool and many insurance companies still don´t cover its routine use.
A second point is that, not all post-operative thyroidectomy voice outcomes are related to vocal fold mobility issues [3,10- 13]. Voice production involves other factors, such as mechanical,aerodynamic, resonance and emotional factors. Aerodynamic variables play an important role in voice production. Voluminous thyroid lesions can distort laryngotracheal anatomy by external compression, thereby altering airflow past the vocal folds. The majority of thyroid disease with surgical indication develops insidiously over time and anatomical structures in vicinity adapt to this increased volume over a long period. Surgery induces a sudden change of the involved and surrounding anatomy. This sudden change may also be perceived by the patient as a vocal change. Lastly, removal of the thyroid gland may induce irritation or cause minor damage to the external laryngeal muscles, resulting in altered phonatory function.
Baseline vocal and laryngeal conditions before surgery play a role as well. In a previous prospective study by the authors [14], vocal pre-operative quantitative scores were positive for dysphonia in 36% of patients and vocal handicap indices confirmed either slight or moderate impairment in most patients.
The primary objective of this one year long prospective cohort study in post-thyroidectomy patients was to analyze vocal function and laryngoscopy results in patients without postthyroidectomy vocal fold immobility.
Our secondary objective was to analyze if thyroid specimen volume has prognostic significance in long-term post-operative voice quality in patients without vocal fold immobility after thyroid surgery
MATERIALS AND METHODS
Patient Population
A prospective cohort study was performed on a population of 90 consecutive patients over the age of 18 who were set to undergo either hemi or total thyroidectomy. Follow up was assessed over the first post-operative year. Exclusion criteria included age less than 18 years, previous thyroid surgery, radiotherapy of the head and neck region, previous laryngeal or cervical surgery, known anatomic or functional laryngeal pathology with previous treatment, and cervical trauma.
All patients gave their informed consent. Approval for the study was obtained from the Hospital da Luz Ethics Committee (CES/017/2014/PA).
Pre-Operative and post-operative evaluation
Variables analyzed were age, gender, occupation (vocal use), fine needle aspiration (FNA) result of suspect thyroid nodule, preoperative determination of thyroid echographic volume (cm3,), type of surgery, thyroid surgical specimen histopathological diagnosis, thyroid surgical specimen volume (cm3,), total surgical thyroid specimen weight (gram), and thyroid stimulating hormone (TSH). Thyroid
Thyroid volume was determined in cm3 (based in anteroposterior, lateral and transversal section dimensions) from both ultrasound determinations (eco volume) and from thyroid surgical specimen dimensions; weight in gram was determined from surgical specimen.
FNA result was classified according to the Bethesda system for reporting thyroid cytopathology 2015
TSH was registered pre-operatively and at three, six and twelve months post-operatively (before completion of the first post-operative month these results are not routinely assessed in our clinical practice).
Symptomatology
Patient complaints relating to possible laryngeal dysfunction were assessed including dysphonia (voice change or vocal fatigue), dysphagia (limitation of swallowing or globus sensation) and dyspnea (tiredness or preferential sleeping position conditioned by breathing complaints).
Voice Evaluation
Vocal use was assessed according to the Koufman classification [15].
Voice evaluation was performed for every patient in the study by the same speech – language pathologist using 1) a headset omnidirectional microphone (PYLE PMEMI), with electric condenser, frequency response of 20Hz- 20KHz and -44dB ±3dB sensitivity, placed at a constant position of 4 cm lateral to and at a 45º angle from the speaker’s mouth (Dejonckere et al., 2001); 2) a portable digital 16 bits mono recorder (TASCAM DR-05), with a sample frequency of 44100 Hz; 3) a digital sound level meter, model Rolls SLM305m, with assurance of ambient noise bellow 50 dB (Dejonckere et al., 2001). Equipment was always tested and calibrated using a reference pure tone of 500 Hz and confirmed by acoustic analysis at the beginning of each recording day. Voice samples were recorded with the patient seated in a comfortable position.
Voice evaluation was performed and registered preoperatively (time 0), one month after surgery (1 month), three months after surgery (3 month), six months after surgery (6 month) and twelve months after surgery (12 month).
Voice evaluation included: auditory-perceptual evaluation of sustained vowel /a/ with the scale GRBAS (Hirano, 1981) [16] selfevaluation with Voice Handicap Index (VHI) [17], aerodynamic evaluation with the measurement of maximal phonation time (MPT, sec); acoustic evaluation for the parameters fundamental frequency (f 0), jitter (%) and shimmer (%) for sustained vowel /a/, vocal extension (VER, Hz) for reading the “Artur the Rat” (Guimarães, 2002) [18] and fundamental frequency for the high pitch sustained /i/ (HP f 0 /i/ or F0/i/max).
Laryngeal Stroboscopy Examination (Blinded)
LS recording was obtained using Kay Pentax RLS 9100 B. LS was performed either transoral or with a flexible endoscope according to patient choice and tolerance. LS evaluated the presence of structural abnormalities, functional changes and immobility. Examination tasks were standardized and included visualization during quiet breathing, sustained /i/, repetitive /i/ and breath, and pitch glides. Structural abnormalities included nonspecific laryngeal inflammation (NSI) and vocal fold lesions. Functional changes were assessed as present or absent and included both insufficiency (incomplete glottic closure at the onset of phonation) and squeezing (supraglottic laryngeal compression). Pitch glide was routinely assessed and registered. Pooling of secretions as an indirect sign of swallowing impairment was assessed and considered positive if present.
LS was performed and recorded pre-operatively (time 0), one month after surgery (1 month), three months after surgery (3 month), six months after surgery (6 month) and twelve months after surgery (12 month). LS examination recordings were blindly viewed and classified by a third-party fellowship-trained laryngologist reviewer from another tertiary care hospital.
Statistics
Using SPSS 20 for Windows, a descriptive analysis was conducted. Normality of variables was tested. Tested variables had a non-parametric distribution, so the Spearman test for correlation of variables was applied. More than 20 % of expected frequencies of results were less than 5 so, even though similar Chi square test results were obtained, Spearman test results IρI are presented for consistency.
Long-term results of voice variables at times 0,1,3,6,12 months were obtained for the global study population. Voice assessment results were subsequently divided and analyzed independently in the subpopulation of patients without postoperative vocal fold immobility. Long-term results for symptoms and LS at times 0,1,3,6,12 months were assessed.
Graphic representation of voice assessment, symptoms and LS results was performed in the global study population and in the subpopulation without vocal fold immobility.
Correlation was assessed using Pearson correlation test. Correlation coefficient (R2 value) interval used for low degree correlation was [0.1-0.29]; for moderate degree correlation [0.3-0.49] and for high degree correlation [0.5-1]. When applicable, significance of correlation was determined at the 0.01 level (2-tailed) or at the 0.05 level (2-tailed). Analysis was performed for the existence of possible single variable correlation between thyroid volume and voice evaluation results: dysphonia symptoms, GRBAS – G subscore positive for dysphonia in perceptive analysis, acoustic variables (f 0 IaI, HP f 0 /i/), aerodynamic variable (MPT IaI), and self-evaluation (VHIFi subscore).
RESULTS
From a total of 90 patients included pre-operatively, 84 patients returned for re-evaluation at 1 month, 81 at 3 months, 68 at 6 months and 58 completed the study at 12 months.
Demographics
The population comprised 90 patients (74 women and 16 men) with a mean age of 50 years (s.d 13.76), ranging between 27 and 85 years of age. As for vocal use, 2 (2.2%) were professional voice users, 31 (34.1%) were habitual voice users and 57 (62.6%) were sporadic voice users based on Koufman scale (data was missing for 1 patient).
Thyroid disease related results
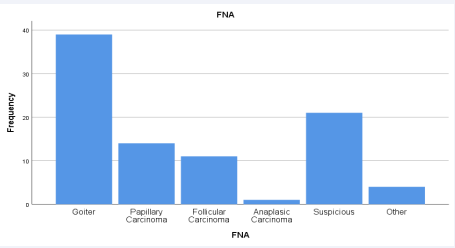
a. Pre-operative thyroid variables FNA results are presented in figure 1.
Figure 1: FNA results.
The chi-square test for gender and FNA showed that there is no significant association in this population. Mean thyroid echographic volume in cm3 , revealed 50.47 cm3 on the left (s.d. 74,15), 34.85 cm3 on the right (s.d. 38.87) and 81.52 cm3 total (s.d. 86.13).
b. Surgical procedure
From the baseline population of 90 patients, 6 did not ultimately undergo a thyroidectomy after referral to the voice clinic. Therefore, the post-operative population comprises 84 patients. Surgical procedures comprised 38 total thyroidectomies (41.8%) and 46 hemithyroidectomies (50.5%). A secondary total thyroidectomy was performed in 6 patients with a previous partial thyroidectomy for tumor.
c. Post-operative thyroid variables - surgical specimen Histopathologic diagnosis
Thyroid specimen histopathologic results demonstrated a pre-operative preponderance of goiter (45.1%), with papillary carcinoma as the second most frequent diagnosis (24.2%). Malignant diagnoses (papillary, follicular and oncocytic carcinomas) were present in 39.6% of the patients.
Thyroid volume (cm3) and weight (g)
62 subjects underwent a pre-operative echographic analysis of the left lobe volume. The mean value of was 50.48 cm3 (s.d. 74.15).
60 subjects had a right lobe volume analysis with a mean value of 34.85 cm3 (s.d. 38.871).
60 subjects had a total thyroid weight analysis with a mean value of 81.52 g (s.d. 86.135).
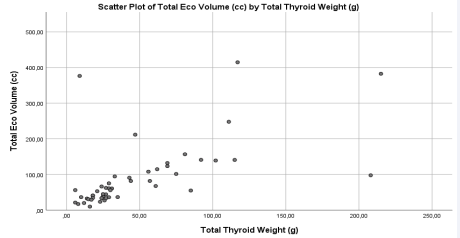
There is a positive moderate correlation between preoperative total thyroid echographic volume and total thyroid specimen volume (r = 0.603; p < 0.01). There is also a positive moderate correlation between pre-operative total thyroid echographic volume and post-operative total thyroid weight (r = 0.603, p < 0.01) – Figure 2.
Figure 2: Correlation between pre-operative ecographic volume (cm3 = cc) and thyroid weight (gram=g).
TSH determination
TSH value determination was within normal range in 92% of patients pre-operatively. In the post-operative determinations, if the TSH value was changed it was increased, consistent with a hypothyroid status. In the 3-month evaluation, TSH was within normal range in 83% of patients and this value increased to a sustained 88% of cases after 6 months. The proportion of normal thyroid status was 12:1 pre-operatively and 7:1 at 12 months post-operatively.
Voice assessment in subpopulation without postoperative vocal fold immobility
There was no diagnosis of immobility pre-operatively. From patients who returned for follow up, immobility was present in 6 out of 86 patients at 1 month, 4 out of 81 patients at 3 months, 5 out of 68 patients at 6 months (after totalization) and 3 out of 58 patients at 12 months.
In patients without post-operative immobility, we present results obtained for voice evaluation, LS functional changes (either insufficiency or squeezing) and thyroid volume.
a. Symptoms
Dysphonia reported by patients increased dramatically in the first post-operative month and then steadily reduced to a level less than pre-operative baseline condition at 12 months (Table 1).
Table 1: Dysphonia frequency and percent in patients without post-operative vocal fold immobility.
|
|
Pre-operative (n=90) |
1 month (n=80) |
3 months (n=77) |
6 months (n=63) |
12 months (n=55) |
|
Frequency |
53 |
62 |
58 |
49 |
41 |
|
Percent |
25% |
53% |
41% |
31% |
17% |
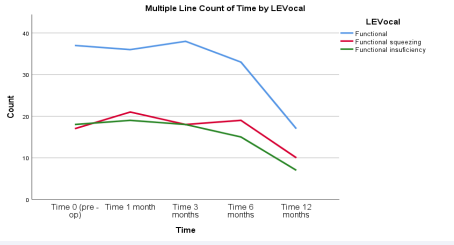
b. LS examination
Functional changes were analyzed for either squeezing or insufficiency. Global functional changes decreased at 1 month, slightly increased at 3 months, followed by an eventual decrease below the pre-operative condition at 6 months, and then revealed a dramatic decrease at 12 months to a functional status much better than pre-operative condition (Figure 3).
Figure 3: Functional changes in LS examination over time.
c. Voice evaluation
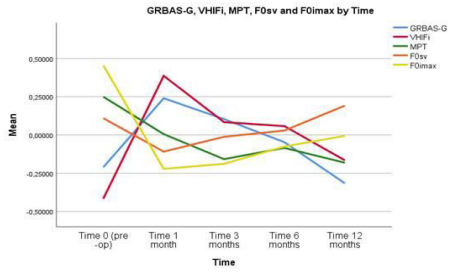
We analyzed G grade from the GRBAS scale, Fi subscore from the VHI questionnaire, MPH, f0/a/ and HPf0/i/.
Analyzing GRBAS-G grade of dysphonia results, the number of patients with dysphonia almost doubled at 1 month, followed by a sharp decrease at 3 and 6 months. There was a steadier but continuous descent at 12 months to a lower incidence of dysphonia at 12 months compared to pre-operative evaluation.
Subscore Fi from the VHI index relates to physical effort in vocal production self-perceived by the patient. Its behavior postoperatively, even though its score was within normal value, parallels that of GRBAS G grade with a sharp self-perceived increased effort in the first post-operative month followed by a steady decrease to a better Fi mean subscore compared to preoperative mean value.
Regarding MPT /a/, its variation over time did not reveal significant changes. Variable f0/a/ did not show variation over time as well. Conversely, when analyzing HPf0/i/, there was a sharp decrease in its value in the first post-operative month in line with patients’ complaints of dysphonia, GRBAS G grade and physical effort revealed by Fi subscore of VHI. Afterwards, itsvalue slowly and steadily increases but it does not recover to the pre-operative value, maintaining a decrease of 60 Hz in its mean value.
Multiple lines Figure 4
Figure 4: Multiple line graphic of GRBAS -G, VHI-Fi, f0/a/, HP f0/i/ over time.
clearly demonstrates intra and intervariable changes of these factors over time.
Correlation essay in the subpopulation without postoperative vocal fold immobility
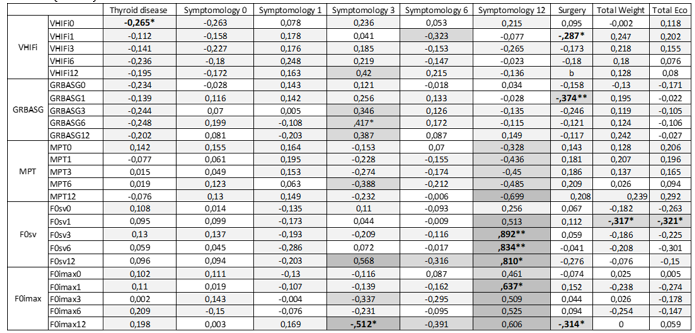
Pearson correlation coefficient was determined to identify possible correlations of VHIFi, GRBAS-G grade higher than 1, MPT, F0 /a/ (F0sv) and HPf0/i/ with self-perceived dysphonia over the first year, and total pre-operative echographic thyroid volume. Correlations are detailed in Table 2.
Table 2: Pearson correlation of variables. R2 value intervals: [0.1-0.29] - low degree correlation (light gray); [0.3-0.49] - moderate degree correlation (medium gray); [0.5-1] - high degree correlation (dark gray); *correlation is significant at the 0.01 level (2-tailed); ** correlation is significant at the 0.05 level (2-tailed).
VHIFi, as a score for physical effort perceived by the patient in voice production, had a low/moderate correlation with total echographic volume and self-perceived dysphonia, more evident from the pre-operative evaluation up to the 6th month evaluation.
Dysphonia confirmed by a GRBAS G score than 1, had a low correlation with weight and total echographic volume.
MPT as an aerodynamic variable of voice had a low/moderate correlation with self-perceived dysphonia from the first up to the sixth post-operative month and a low correlation with weight and total echographic volume.
F0 /a/ (F0sv) had a high-degree of correlation (significance level 0.01) with self-perceived dysphonia in the 12th month. F0 /a/ (F0sv) in the first post-operative month had a moderate degree of correlation (significance level 0.01) with total weight and echographic volume.
HP f 0 /i/ had a low/moderate degree of correlation with selfperceived dysphonia after the third month and this correlation was high in the 12th post-operative month (significance level 0.05). HP f 0 /i/ in the 12th month also had a moderate degree correlation with surgery (significance level 0.01).
DISCUSSION
When analyzing patients without post-operative vocal fold immobility, variable correlations are concordant with our hypothesis of weight and echographic volume playing a role in dysphonia. VHIFi and GRBAS G grade both revealed a low/ moderate correlation with weight and total echographic volume. F0 /a/ (F0sv) is an objective measure of voice and correlated with self-perceived dysphonia in all study patients without immobility. Interestingly this correlation was stronger at the 12th post-operative month. These results strongly suggest F0 /a/ (F0sv) plays a role in the dysphonia perceived by these patients and it is a confirmation that the symptom is effectively related to a change in voice quality.
HP f 0 /i/ was included as a measure of vocal behavior in the falsetto range. Anatomic change induced by surgery in the prelaryngeal muscles with resultant fibrous deposition (promoting reduced elasticity) and superior laryngeal nerve lesion are two possible reasons for cricothyroid muscle function compromise. It would be reasonable to assume that HP f 0 /i/, a measure of voice in the high pitch range, may be compromised after thyroid surgery because vocal extension for high pitch production derives both from cricothyroid muscle function and the superior laryngeal nerve´s innervation of this muscle. Effectively, in patients without post-operative vocal fold immobility, HP f 0 /i/ had a low/moderate correlation with self-perceived dysphonia after the 3rd month with a high degree of correlation showing a significance level 0.05 in the 12th month. HP f 0 /i/ in the 12th month also has a moderate correlation with surgery with 0.01 significance.
These results of our study demonstrate a compromise in voice throughout the first post thyroidectomy year in patients without vocal fold immobility. Patients perceive dysphonia and the symptom are confirmed by self-perceived scores of effort in voice production and objective perceptive analysis of voice.
According to the results of our study, dysphonia in patients without vocal fold immobility is related to weight of the surgical specimen and echographic thyroid volume. It is related to F0 /a/ change and HP f 0 /i/ reduction (mean 60Hz). HP f 0 /i/ changes may be a reason for singing limitations perceived by patients in the long-term. Based on the results of this study in patients without vocal fold immobility, we propose echographic thyroid volume as a new pre-operative prognostic factor for post-operative dysphonia relating to F0 /a/ change and HP f 0 /i/ reductions in the first post-operative year.
Further research is needed to assess the criteria for thyroid volume significance in voice compromise without vocal fold immobility. Multivariate analysis for the significance of echographic volume in this subpopulation would be beneficial to determine whether or not it could be considered an independent risk factor. Further study is also needed to assess whether increased echographic thyroid volume may also be an independent risk factor for post-operative vocal compromise in patients with post-operative vocal fold immobility. This would help to stratify the risk of muscular and nervous structures damage in patients with increased thyroid volume prior to surgery.
CONCLUSIONS
Vocal compromise in the first year after thyroid surgery is present in patients without vocal fold immobility. Voice changes in these patients involve F0/a/ change and HP f 0 /i/ reductions (mean 60Hz). These voice changes are related to thyroid volume and weight which, in turn, are correlated to pre-operative echographic thyroid volume. Increased echographic thyroid volume should be considered a pre-operative prognostic factor for vocal compromise after thyroid surgery in patients without post-operative vocal fold immobility.
ACKNOWLEDGEMENTS
Patrícia Lagarto Martins, PhD, ISEG, University of Lisbon, for statistical support
REFERENCES
- Chandrasekhar SS, Randolph GW, Seidmain MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013; 148: S1-37.
- Hodin R, Clark O, Doherty G, Grant C, Heller K, Weigel R. Voice issues and laryngoscopy in thyroid surgery patients. Surgery. 2014; 154: 46- 47.
- Caroline M, Joglekar S, Mandel S, Sataloff R, Heman-Ackah Y. The predictors of postoperative laryngeal nerve paresis in patients undergoing thyroid surgery: a pilot study. J Voice. 2012; 26: 263-6.
- Lorenz K, Abuazad M, Sekulla C, Schneider R, Thanh P, Dralle H. Results of intraoperative neuromonitoring in thyroid surgery and preoperative vocal cord paralysis. World J Surg. 2014; 38: 582-91.
- Stevens K, Stojadinovic A, Helou L, Solomon N, Howard R, Shriver C, et al. The impact of recurrent laryngeal neuromonitoring on multi- dimensional voice outcomes following thyroid surgery. J Surg Oncol. 2012; 105: 4-9.
- Fontenot T, Randolph G, Setton E, Alsaleh N, Kandil E. Does intraoperative nerve monitoring reliably aid in staging of total thyroidectomies? Laryngoscope. 2015; 125: 2232-5.
- Lin Y, Dionigi G, Randolph G, Lu IC, Chang PY, Tsai SY, et al. Electrophysiologic monitoring correlates of recurrent laryngeal nerve heat thermal injury in a porcine model. Laryngoscope. 2015; 125: E283-E290.
- Randolph G, Kamani D. Intraoperative electrophysiologic monitoring of the recurrent laryngeal nerve during thyroid and parathyroid surgery: experience with 1381 nerves at risk. Laryngoscope. 2017; 127: 280-6.
- Schneider R, Randolph G, Dionigi G, Barczynski M, Chiang FY, et al. Prospective study of vocal fold function after loss of the neuromonitoring signal in thyroid surgery: the international neural monitoring study group´s POLT study. Laryngoscope. 2016; 126: 1260-1266.
- Grover G, Sadler G, Mihai R. Morbidity after thyroid surgery: patient perspective. Laryngoscope. 2013; 123: 2319-2323.
- ?Siegel B, Ow TJ, Abraham SS, Loftus PA, Tassler AB, Smith RV, et al. How Radiologic/Clinicopathologic Features Relate to Compressive Symptoms in Benign Thyroid Disease. Laryngoscope. 2017; 127: 993- 7.
- Yomaza R, Tagliarini J, Rodrigues S, Tavares E, Martins R. Laryngeal and vocal alterations after thyroidectomy. Braz J Otorhinolaryngol. 2019; 85: 3-10.
- Al-Qurayshi Z, Randolph G, Srivastav S, Aslam R, Friedlander P, et al. Outcomes in thyroid surgery are affected by racial, economic, and healthcare system demographics. Laryngoscope. 2016; 126: 2194- 2199.
- Sara IR Viana Baptista, David G. Lott, Sancha CC Almeida, Maria Olimpia Cid, Paulo S. Vera-Cruz, Carlos Zagalo. Preoperative voice characteristics in thyroid patients. J Voice. 2021; 35: 809.
- Koufman JA, Isaacson G. The spectrum of vocal dysfunction. Otolaryngol Clin North America. 1991; 24: 985-8.
- Hirano M. Clinical Examination of Voice. Vienna: Springer-Verlag; 1981.
- Guimarães I, Abberton E. An investigation of the voice handicap index with speakers of Portuguese: preliminary data. J Voice. 2004; 18: 71- 82.
- Guimarães I. An electrolaryngographic study of dysphonic Portuguese speakers. Dissertação de Doutoramento. University of London. 2002.