Patterns of Cervical Lymph Node Metastases from Skin Malignancies of the Head and Face
- 1. Department of Otolaryngology-Head and Neck Surgery, Gifu University Graduate School of Medicine, Gifu, Japan
- 2. Department of Head and Neck Surgery-Otolaryngology, Ogaki Municipal Hospital, Gifu-ken, Japan
ABSTRACT
Objective: This study aimed to describe the patterns of metastasis from skin cancer of the head and face to the cervical lymph nodes.
Methods: Neck dissections were performed for 18 patients with skin malignancies of the head and face. After the surgeries, we observed malignant lymph nodes in the dissected tissues as well as postoperative lymph node metastasis.
Results: The primary sites of lymph node metastases to the level I area were the temporal, the eyelid, the internal cantus, the cheek, and the lower lip. The lymph node metastases to levels II, III, and IV did not appear to tend to the primary sites. Metastases to the parotid gland were observed in 11 cases, with primary sites at the parietal for 1 case, the temporal for 1 case, the auricular for 3 cases, the forehead for 1 case, the eyelid for 4 cases, and the cheek for 1 case. Furthermore, 9 patients were diagnosed with metastases to the parotid prior to surgery. Within this subgroup, 6 patients presented with lymph nodes that metastasized to the deep lobe of the parotid and were given a total parotidectomy, and the other 3 cases received a superficial parotidectomy. Additionally, 4 cases underwent preventive superficial parotidectomy. Of these cases, 2 were found to have metastasis to the superficial lobe. Furthermore, a case with the primary site in the lower lip caused contralateral neck metastasis.
Conclusion: Determining the area of neck dissection by the location of the primary site has certain usefulness.
KEYWORDS
Metastasis; Squamous cell carcinoma; Malignant melanoma; Surgical intervention
CITATION
Okuda H, Ohnishi M, Ohashi T, Shibata H, Mori K, et al. (2022) Patterns of Cervical Lymph Node Metastases from Skin Malignancies of the Head and Face. Ann Otolaryngol Rhinol 9(4): 1294.
ABBREVIATIONS
AAO-HNS: American Academy of Otolaryngology-Head and Neck Surgery.
INTRODUCTION
Skin malignant tumors that occur in the head and facial regions often metastasize to the cervical and parotid lymph nodes, and neck dissection is performed. There are few reports regarding the appropriate range for dissections [1,2]. The most effective method to prevent recurrence of cancer in cervical lymph nodes is a radical neck dissection in all areas bilaterally. However, considering the risk of surgical invasion and adverse postoperative symptoms, the area extracted is sometimes limited. Therefore, it is necessary to predict where lymph node metastasis is likely to occur and to determine the appropriate dissection range.
Sentinel lymph node biopsies are commonly used to detect potential lymph node metastases [1]. Most of these biopsies are performed on patients with breast cancer, gynecological cancer, thyroid cancer, and malignant melanoma outside the head and neck areas [3-8]. On the other hand, there are relatively few reports of sentinel lymph node biopsy in the head and neck regions due to the complexity of lymph flow in these areas [9,10]. Herein, we examined cases of lymph node metastasis of carcinomas of the head and face and considered the appropriate range for neck dissection. In particular, we focused on the dissection range of the cervical tissue and parotid gland from the viewpoint of each primary site.
MATERIALS AND METHODS
Participants
From January 2003 to December 2021, 18 patients with malignant facial and head tumors of the skin who underwent neck dissection for cervical or parotid lymph node metastasis participated in this study. The sample consisted of 14 males and 3 females, and the range of age was 37–87 years (with an average age of 67.2 years).
The primary sites were the parietal in 2 cases, the occipital in 1 case, the temporal in 1 case, the auricle circumference in 3 case, the forehead in 1 case, the eyelids circumference in 4 case, the internal canthus in 1 case, the cheeks in 4 cases, and the lip circumference 1 case. The histological types included squamous cell carcinoma in 10 cases, malignant melanoma in 6 cases, and sebaceous adenocarcinoma in 2 cases.
Neck dissection
In principle, modified radical neck dissection was performed on all 18 of the participants, and selective neck dissection was performed depending factors such as age and general condition. The classification of the neck dissection area followed the criteria of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) [11].
At the time of initial treatment, 3 of the 18 patients had lymph node metastases, and primary lesion resection and neck dissection were performed at the same time. The remaining 15 patients had no lymph node metastasis at the time of initial treatment. Therefore, primary lesion resection was performed during the initial treatment, and neck dissection was performed for lymph node metastasis that occurred during postoperative follow-up.
Regarding the management of the parotid gland, if lymph node metastasis is suspected in the superficial parotid gland by preoperative imaging, the superficial lobe of the parotid gland was removed. If the metastasis extended to the deep lobe before or during surgery, a total excision of the parotid gland, including the deep leaves, was performed. In patients with primary tumors on the lateral part of the face, prophylactic superficial parotid gland resection was performed due to high possibility of metastasis to the parotid gland.
Follow-up
The follow-up period was six months after the initial neck dissection, and the participants were examined for possible cervical lymph node recurrence.
Areas where lymph node metastasis was observed in the tissue excised by neck dissection, and areas where lymph node recurrence was observed within the observation period were defined as sites that were at high risk of lymph node metastasis.
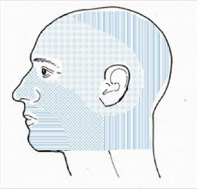
With reference to a past report on facial and head lymphatic anatomy [12], the parietal region and occipital region are region 1, the temporal, forehead, auricle circumference, and eyelid circumference (other than the internal cantus) form region 2. The primary sites were classified with the internal cantus, nose, and cheeks as region 3, and the lip circumference was considered region 4 (Figure 1).
Figure 1 Lymphatic flow of a level I lymph node.
Table 1
Table 1: Tumor resection was performed at another hospital, and the tumor invasion depth at the time of initial treatment was unknown, which is indicated as Tx.
|
Case No. |
Age |
Sex |
Histological |
TNM |
Site |
Region |
|
1 |
58 |
Male |
SCC |
T1N0M0 |
parietal |
1 |
|
2 |
78 |
Male |
MM |
TxN0M0 |
parietal |
1 |
|
3 |
52 |
Male |
MM |
T3aN2bM0 |
occipital |
1 |
|
4 |
74 |
Male |
SCC |
TxN0M0 |
temporal |
2 |
|
5 |
81 |
Male |
SCC |
T1N1M0 |
auricle circumference |
2 |
|
6 |
38 |
Male |
sebaceous adenocarcinoma |
T2N1M0 |
auricle circumference |
2 |
|
7 |
72 |
Female |
MM |
T4aN1M0 |
auricle circumference |
2 |
|
8 |
56 |
Male |
SCC |
TxN0M0 |
forehead |
2 |
|
9 |
59 |
Male |
sebaceous adenocarcinoma |
TxN0M0 |
eyelids circumference |
2 |
|
10 |
75 |
Male |
SCC |
TxN0M0 |
eyelids circumference |
2 |
|
11 |
59 |
Male |
SCC |
T1N0M0 |
eyelids circumference |
2 |
|
12 |
75 |
Female |
SCC |
T1N0M0 |
eyelids circumference |
2 |
|
13 |
50 |
Male |
MM |
T2bN0M0 |
internal cantus |
3 |
|
14 |
87 |
Male |
MM |
T4aN0M0 |
cheeks |
3 |
|
15 |
79 |
Male |
MM |
T4aN1M0 |
cheeks |
3 |
|
16 |
67 |
Female |
SCC |
T2N0M0 |
cheeks |
3 |
|
17 |
75 |
Female |
SCC |
TxN0M0 |
cheeks |
3 |
|
18 |
74 |
Male |
SCC |
TxN0M0 |
lip circumference |
4 |
|
Abbreviations: SCC: Squamous Cell Carcinoma; MM: Malignant Melanoma |
||||||
We examined the relationship between metastasis pattern and primary site.
RESULTS
Metastases to level I were found in 3 of 9 cases in region 2 (case 9, 10, and 13) and in 4 of 5 cases in region 3 (case 13, 14, 15, and 16). Metastasis to levels V was observed in 2 of 3 cases in region 1 (case 1 and 2) and 1 of 9 case in region 2 (case 4). Besides, Metastases to the superficial cervical lymph nodes were observed in 6 cases (case 2, 5, 9, 10, 11 and 13), and metastases to level II, III, IV were observed in 8 cases (case 2, 3, 4, 9, 10, 16, 17, and 18). None of them seemed to have a tendency toward the primary region. In Case 2, recurrence was observed in levels II, III, and IV one month after the neck dissection. One case developed contralateral level I metastasis 2.5 months after surgery in region 4 (case 18).
Metastases to the parotid lymph nodes were found in 1 of 3 cases in region 1 (case 1), 9 of 9 cases in region 2 (case 4-12), and 1 of 5 cases in region 3 (case 16), for a total of 11 cases overall. Of these 11 cases, 5 presented with superficial cervical lymph node metastasis, and all occurred in region 2 (case 5-9). Of the 4 cases in which a parotid gland superficial lobectomy was performed prophylactically (case 7, 8, 15, and 17), metastasis were found in the excised tissue in 2 cases in region 2 (case 7 and 8) (Table 2).
Table 2: Metastatic patterns and postoperative course by primary site.
|
Case No. |
Region |
Level |
superficial cervical lymph nodes |
Parotid grand |
||||
|
I |
II |
III |
IV |
V |
||||
|
1 |
1 |
? |
? |
? |
? |
? |
? |
?(Total) |
|
2 |
1 |
? |
? |
? |
? |
? |
? |
|
|
3 |
1 |
? |
? |
? |
? |
? |
? |
|
|
4 |
2 |
? |
? |
? |
? |
? |
|
?(Total) |
|
5 |
2 |
? |
? |
? |
? |
? |
? |
??superficial lobe? |
|
6 |
2 |
? |
? |
? |
|
|
|
??superficial lobe? |
|
7 |
2 |
? |
? |
? |
? |
|
|
??superficial lobe? |
|
8 |
2 |
|
|
|
|
|
|
??superficial lobe? |
|
9 |
2 |
? |
? |
? |
? |
|
? |
??superficial lobe? |
|
10 |
2 |
? |
? |
? |
? |
? |
? |
?(Total) |
|
11 |
2 |
? |
? |
? |
? |
? |
? |
?(Total) |
|
12 |
2 |
? |
? |
? |
|
? |
|
?(Total) |
|
13 |
3 |
? |
? |
? |
? |
? |
? |
|
|
14 |
3 |
? |
|
|
|
|
|
|
|
15 |
3 |
? |
? |
? |
? |
? |
? |
??superficial lobe? |
|
16 |
3 |
? |
? |
? |
|
|
|
?(Total) |
|
17 |
3 |
? |
? |
? |
? |
? |
? |
??superficial lobe? |
|
18 |
4 |
|
? |
? |
? |
? |
? |
|
? Metastatic findings in the dissection tissue
|
||||||||
No clear difference was observed in the metastatic region of each primary site by histological type.
DISCUSSION
Appropriate dissection range by primary site In neck dissection for facial and head malignancies of the skin, it is difficult to determine the appropriate dissection range in a uniform manner. Previous reports have demonstrated that the appropriate dissection range was examined for each primary site; however, there are differences among the reports regarding how to classify the primary site [1,2].
The metastatic patterns of this study were generally aligned with previous reports, although some cases were atypical.
In cases 1 and 2, where level V metastasis occurred with region 1 being the primary area of the tumor, the metastatic pattern was relatively rare. This metastasis occurred either from the primary lesion via the parotid lymph node or directly from the primary lesion. Based on the anatomy of the lymphatic flow, such metastasis is quite possible, and dissection of level V should be considered in the case of primary carcinoma in region 1.
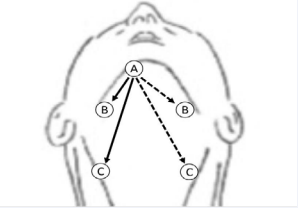
In Case 18 in region 4, contralateral cervical lymph node metastasis occurred early after surgery. The drainage tract of the submental lymph node is said to intersect in the middle [13], and it is possible that metastasis had occurred contralaterally through this tract before surgery (Figure 2).
Figure 2 A: Submental lymph node. B: Submandibular lymph node. C: Upper internal deep cervical lymph node.Solid line: Excretion route to ipsilateral cervical lymph nodes. Dotted line: excretion route to the contralateral cervical lymph node.
Furthermore, recurrence or residual malignant cells may have metastasized to the contralateral side due to the disruption or deviation of the original lymphatic flow as a result of surgery. However, the existence of this pathway should be noted when considering the appropriate dissection range. Therefore, in cases where metastasis was found in level I before surgery, or in cases in regions 2 and 3 where metastasis to level I was frequently observed, there seemed to be room for consideration of preventive search and possible dissection of contralateral level I.
Focusing on the relationship between the superficial cervical lymph node and the parotid lymph node, 4 out of 11 cases involving metastasis to the parotid gland lymph node had metastasis to the superficial cervical lymph node, and all 4 cases were in region 2 (case 5, 9, 10, and 11). Since the cases in region 2 have a higher frequency of metastasis to the parotid lymph nodes in comparison to cases in other regions, metastasis from the parotid lymph nodes to the superficial cervical lymph nodes occurs at a relatively high rate, especially in region 2. In the case of, the tendency is considered to be remarkable. Few previous reports have examined the treatment of superficial cervical lymph nodes in detail. However, results of this study demonstrate that if the primary site is in region 2 or if metastatic findings are detected in the parotid lymph nodes, the superficial cervical lymph nodes may need to be considered for dissection.
Management of parotid grand
In this study, superficial lobectomy or total resection was performed for cases with metastatic findings in the parotid gland before surgery and cases with primary facial features (parts of regions 1, 2, and 3). In this study, no metastasis was found in the postoperative parotid lymph node in the non-excised parotid gland, and dissection was performed according to our criteria was thought to be appropriate. However, when metastasis to level II occurs, it is reported that malignant cells are retrogradely poured into the parotid lymph node [2]. There are also reports that demonstrate that if metastasis is observed in the parotid grand or at level II, a potential metastasis has a 20% probability of also occurring in another area [14]. Therefore, it is necessary to consider the metastatic patterns of other regions as well.
There are various opinions about the extent of parotid gland removal. One suggested that if metastasis is found in the superficial lobes prior to surgery, patients should undergo total parotid gland removal, including the deep lobes [15]. On the other hand, many reports claim that only superficial lobe removal is sufficient for those who are not considered to have metastasized to the deep lobes [16,17]. Considering the high risks involving the total excision such as facial nerve palsy, we considered that superficial parotid gland resection should be performed if the primary site is in regions 2 or 3 and there are findings of suspected lymph node metastasis in the parotid superficial lobe. If it is thought that lymph node metastasis extends to the deep lobe of the parotid gland, it is considered appropriate to perform total parotid gland excision. As a matter of course, it is necessary to search for potential metastases and to follow up more carefully to see whether deep lobe metastases would occur after surgery.
CONCLUSION
We examined 18 cases with head and facial skin carcinomas with cervical and parotid lymph node metastasis and considered the appropriate range for neck dissection. This study suggests that there is a certain tendency for metastatic patterns to the cervical lymph nodes for each primary site. By classifying the primary site based on the anatomy of general lymphatic flow and accumulating cases, it can be expected that the tendency will become clearer. In addition, regarding the atypical metastatic mode and the management of superficial cervical lymph nodes and parotid glands, it further investigation is indicated to affirm the appropriate dissection range by accumulating cases in the same manner.
REFERENCES
- Sadahiro K, Kenjiro N, Arata T, Ryota T, Junji K, Naoya Y. Sentinel Node Biopsy and Neck Dissection for Cutaneous Head and Neck Malignant Melanoma (Part 2: Neck Dissection). Nichihikaishi. 2013; 123: 1051- 1057. (in Japanese)
- P Suton, I Luksic, D Muller, M Virag. Lymphatic drainage patterns of head and neck cutaneous melanoma: does primary melanoma site correlate with anatomic distribution of pathologically involved lymph nodes? Int J Oral Maxillofac Surg. 2012; 41: 413-420.
- Qiu SQ, Zhang GJ, Jansen L, de Vries J, Schröder CP, de Vries EGE, et al. Evolution in sentinel lymph node biopsy in breast cancer. Crit Rev Oncol Hematol. 2018; 123: 83-94.
- Rossi EC, Tanner E. Controversies in Sentinel Lymph Node Biopsy for Gynecologic Malignancies. J Minim Invasive Gynecol. 2021; 28: 409- 417.
- Morrison S, Han D. Re-evaluation of Sentinel Lymph Node Biopsy for Melanoma. Curr Treat Options Oncol. 2021; 22: 22.
- Mok CW, Tan SM, Zheng Q, Shi L. Network meta-analysis of novel and conventional sentinel lymph node biopsy techniques in breast cancer. BJS Open. 2019; 3: 445-452.
- Zhang X, Bao B, Wang S, Yi M, Jiang L, Fang X. Sentinel lymph node biopsy in early stage cervical cancer: A meta-analysis. Cancer Med. 2021; 10: 2590-2600.
- Albers MB, Nordenström E, Wohlfahrt J, Bergenfelz A, Almquist M. Sentinel Lymph Node Biopsy in Thyroid Cancer. World J Surg. 2020; 44: 142-147.
- Sharma D, Koshy G, Grover S, Sharma B. Sentinel Lymph Node Biopsy: A new approach in the management of head and neck cancers. Sultan Qaboos Univ Med J. 2017; 17: e3-e10.
- Roman Kia Rahimi-Nedjat, Bilal Al-Nawa, Andrea Tuettenberg, Keyvan Sagheb, Stephan Grabbe, Christian Walter. Sentinel lymph node biopsy in malignant melanoma of the head and neck. Craniomaxillofac Surg. 2018; 46: 1027-1031.
- Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW. Standardizing neck dissection terminology. Official report of the Academy’s Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg. 1991; 117: 601-5.
- Yukihide T, Osamu F, Shigeo I. Radical neck dissection and simultaneous parotid gland resection for skin malignancy of the head and face. Nichikeikaishi. 1991; 11: 384-392.
- Yohei S, Kaori I, Soga F, Eiichiro U, Hideya T, Norito K, et al. A case of squamous cell carcinoma on the apex of the nose with bilateral submandibular lymph node metastases. Skin Cancer. 2007; 22: 303- 306.
- Sydney Ch’ng, Aloka Maitra, Robert S Allison, John M Chaplin, Reinhold T Gregor, Rodney Lea, et al. Parotid and cervical nodal status predict prognosis for patients with head and neck metastatic cutaneous squamous cell carcinoma. J Surg Oncol. 2008; 98: 101-105.
- Joshua J Thom, Eric J Moore, Daniel L Price, Jan L Kasperbauer, Sidney J Starkman, Kerry D Olsen. The Role of Total Parotidectomy for Metastatic Cutaneous Squamous Cell Carcinoma and Malignant Melanoma. JAMA Otolaryngol Head Neck Surg. 2014; 140: 548-554.
- JAD Jol, MLF van Velthuysen, FJM Hilgers, RB Keus, H Neering, AJM Balm. Treatment results of regional metastasis from cutaneous headand neck squamous cell carcinoma. Eur J Surg Oncol. 2003; 29: 81-86.
- Theodore S Hong, Kevin J Kriesel, Gregory K Hartig, Paul M Harari. Parotid area lymph node metastases from cutaneous squamous cell carcinoma: implications for diagnosis, treatment, and prognosis. Head Neck. 2005; 27: 851-856.