Pulmonary Edema and Hemorrhage after Aesthetic Nasal Surgery
- 1. Department of Surgery, University of Sao Paulo, Brazil
- 2. Department of Plastic Surgery, University of Sao Paulo, Brazil
- 3. Department of Otolaryngology, University of Sao Paulo, Brazil
ABSTRACT
Negative pressure pulmonary edema following tracheal extubation is an uncommon and life-threatening complication of patients undergoing endotracheal intubation and general anesthesia for surgical procedures. The common pattern in these cases is the occurrence of an episode of airway obstruction upon emergence from general anesthesia, usually caused by laryngospasm. Patients who are predisposed to airway obstruction may have an increased risk of airway complications upon extubation after general anesthesia. This paper presents the case of a young male with repaired cleft lip and palate submitted to aesthetic nasal surgery under general , who exhibited sudden respiratory insufficiency and pulmonary hemorrhage immediately after tracheal extubation. Prevention and early relief of upper airway obstruction may decrease the incidence of pulmonary edema and hemorrhage after surgery.
KEYWORDS
Pulmonary edema, Aesthetic nasal surgery, Negative pressure pulmonary
CITATION
Tonello C, Yoshida M, de Barros Baptista MAF, Alonso N (2016) Pulmonary Edema and Hemorrhage after Aesthetic Nasal Surgery. Ann Otolaryngol Rhinol 3(1): 1081.
INTRODUCTION
The negative pressure pulmonary edema (NPPE) after tracheal extubation is a relatively known condition, yet it is seldom accompanied by diffuse alveolar hemorrhage. Obstruction of the upper airway by a closed glottis, as observed in laryngospasm, may lead to marked respiratory effort with great gradient of negative intrathoracic pressure [1]. This condition may be observed after endotracheal extubation and non-cardiogenic pulmonary edema may take place, associated with laryngospasm as the main cause [2]. This paper presents the case of a young male patient submitted to aesthetic nasal surgery under general anesthesia, who exhibited sudden respiratory insufficiency and pulmonary hemorrhage immediately after tracheal extubation.
CASE REPORT
A healthy male patient, aged 17 years, with repaired cleft lip and palate, was submitted to general anesthesia for rhinoseptoplasty. Propofol and phentanyl were administered during anesthetic induction, followed by an atraumatic orotracheal intubation.
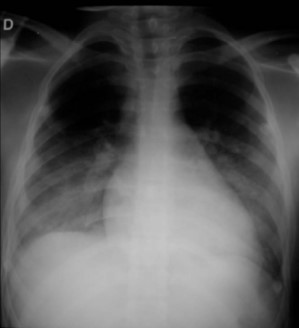
After loco-regional application of approximately 15 ml of anesthetic solution with adrenaline 1:100000 in the nose, a tampon were placed in the hypopharynx for airway protection. Approximately 300 ml of Ringer Lactate solution were injected during the trans operative period of nearly two hours. After extubation the patient presented respiratory efforts without significant airflow, desaturation and tachycardia. Notwithstanding the attempts of ventilation with supplementary oxygen using a mask, the patient did not present improvement in saturation. Immediately after a traumatic endotracheal intubation the patient exhibited outflow of a pinkish, bubbling secretion through the orotracheal tube. The endotracheal secretion progressively became overtly bloody. After partial improvement of ventilation and oxygen saturation, the patient was referred to the Intensive Care Unit (ICU), where he remained hospitalized for twodays. The thoracic radiography at admission in the ICU evidenced bilateral interstitial opacification with absence of cardiomegaly and/or apparent increase in pulmonary vascularization (Figure 1).
Figure 1: Bilateral interstitial opacification with absence of cardiomegaly and/or apparent increase in pulmonary vascularization on thoracic radiography.
The arterial gasometry revealed the following values: pH: 7.31, pCO2 : 58, pO2 : 53.9, bic: 28.3, BE: 0.9 and satO2 : 83.
After 24 hours the patient was submitted to bronchoscopy, which evidenced bilateral pulmonary bleeding, yet without a clearly identified focus. The patient was maintained in mechanical ventilation for 46hours, and then he was extubated due to the progressive improvement of clinical conditions and transferred to the inpatient unit.
DISCUSSION
The reported case exhibited sudden respiratory deficiency complicated by pulmonary hemorrhage after tracheal extubation in a young patient submitted to an uneventful nasal surgery under general anesthesia. Considering this situation, the diagnosis of negative pressure pulmonary edema (NPPE) was suggested. This condition basically occurs in two situations: after immediate improvement of a chronic obstructive process, and more frequently as a result of upper airway obstruction [3].Even though laryngeal trauma, epiglottitis, hematoma and foreign body aspiration may trigger upper airway obstruction, laryngospasm remains as the most common cause [3,4]. The pathophysiological findings result basically from alterations in the transmembrane Starling forces [2] affecting the microvascularization and pulmonary alveoli. After laryngospasm, the patient continues inspiring against a closed glottis, similar to a modified Muller maneuver; this great inspiratory effort generates a marked negative intrathoracic pressure leading to an increase in venous return to the right heart and pulmonary arteries. This volume expansion causes high capillary and arteriolar pressure, which favors the accumulation of transudate in interstitial and alveolar spaces. Immediately thereafter, there is hypoxic vasoconstriction of systemic and pulmonary arterioles leading to increase in blood pressure and after-load increase in the left and right ventricles. Simultaneously, there is great concentration and increase in systemic catecholamines, worsening the peripheral vascular resistance [1,2,5,6].
Therefore, the etiology of bleeding in NPPE may probably be the rupture of these pulmonary capillaries. The increased stress in the pulmonary capillary wall may cause mechanical rupture of the alveolar-capillary membrane with subsequent damage to the barrier function, in a process called “stress failure” [1,7,8]. As demonstrated in the literature, the present case is very similar to the conditions and profile of patients affected by NPPE. The evolution of sudden respiratory impairment due to pulmonary edema is often observed in young patients, many of whom are athletes who present marked cardiopulmonary capacity, which allows them to maintain an extremely strong inspiration during a long period of apnea against an obstructed airway [9]. In addition to the male gender, age below 40 years and the muscular biotype of the patients, other potential risk factors are short thick neck, Mallampatiscore III, history of obstructive sleep apnea-hypopnea syndrome (OSAHS) and non-utilization of laryngotracheal topic anesthetics during intubation and intravenous administration of lidocaine before extubation [3]. Notwithstanding, patients submitted to surgical procedures involving.
the upper aerodigestive tract present higher risk of NPPE. Awaken patients are less prone to maintain a closed glottis after a laryngospasm event, different than general anesthesia, during which the laryngeal reflex response is usually increased. The postoperative laryngospasm presents an approximate prevalence of 0.1%; however, among patients with need of active intervention for acute airway obstruction, 11% present evolution to NPPE and death in up to 2% [3,10]. Previous animal studies demonstrated that glottic closure is a reflect of stimulation of the superior laryngeal nerve; therefore, care should be taken in situations of manipulation of the upper aero digestive tract. Thus, surgeries as rhinoseptoplasty under general anesthesia present several aspects that may predispose to NPPE and occasionally subsequent pulmonary hemorrhage, because procedures involving placement and removal of hypopharynx tampons, as well as suction of oropharyngeal secretions, among others, may trigger stimuli to the pharynx and larynx. It is believed that some maneuvers to prevent the laryngeal stimulation upon extubation may reduce the occurrence of laryngospasm, yet no measurement is demonstrably effective. These include: placement of oropharyngeal tampon before injections and careful suction of the oropharynx before tampon removal, to prevent contact with blood and other materials and laryngeal irritation, as well as gentle intubation, limitation of aggressive oropharyngeal suction and extubation in stage I plane of anesthesia [3]. The recommendation of some anesthesiologists to use topical anesthetic spray on the larynx before intubation (laryngotracheal anesthetics - LTA) in risk groups or intravenous administration of lidocaine before extubation seems to reduce the occurrence of laryngospasm and consequently of NPPE.
After establishment of NPPE, the treatment options include ventilatory support with continuous positive pressure, laryngeal mask or endotracheal intubation with ventilatory support in ICU, up to stimulation of diuresis with low doses of furosemide and use of corticosteroids [3,11]. Follow-up with serial thoracic radiographies and eventually thoracic tomography is advised to better analyze the clinical evolution. Bronchoscopy is fundamental for characterization of diffuse alveolar hemorrhage, because it allows observation of the tracheobronchial tree to rule out a specific bleeding site.