Spontaneous Intra-Cochlear Hemorrhage Leading to Sensorineural Hearing Loss
- 1. Department of Clinical Neurosciences, Service of Otorhinolaryngology, Switzerland
- 2. Departement of Radiology, Hôpitaux Universitaires de Genève, Switzerland
ABSTRACT
We hereby present the case of a 32 year old patient with sudden sensorineural hearing loss (SNHL) and an MRI compatible with acute intra-cochlear hemorrhage.
Spontaneous intra-labyrinthine bleeding is a rare cause of SNHL. Bleeding into the membranous labyrinth may lead to high concentrations of blood byproducts. Commonly affected subsites are the basal turn of the cochlea and the vestibule. Depending on the time lapse between the acute event and imaging, as well as on the concentration of the different blood products (methemoglobin), the signal intensity on T1/T2 weighted sequences may vary. Recent articles show that 3D FLAIR imaging is more sensitive than other MRI sequences for the detection of intra-labyrinthine hemorrhage.
Conclusion: Although rare, SNHL may be caused by pathologies that are visible on MRI imaging. MRI FLAIR Imaging allows not only for the detection of the hemorrhage itself but also permits a differentiation from other causes of hypersignal in MRI such as lipomas, which can also cause SSNHL.
KEYWORDS
• Intra-cochlear
• Hemorrhage
• Sensorineural hearing loss
• MRI
• Imaging
CIYTATION
Morrison M, Guinand N, Alianou A, Becker M, Senn P (2017) Spontaneous Intra-Cochlear Hemorrhage Leading to Sensorineural Hearing Loss. Ann Otolaryngol Rhinol 4(1): 1158.
ABBREVIATIONS
SNHL: Sensorineural Hearing Loss; FLAIR: Fluid-Attenuated Inversion Recovery; MRI: Magnet Resonance Imaging
INTRODUCTION
Sensorineural hearing loss (SNHL) occurs after lesions to either to the inner ear, the cochlear nerve (VIII) or the cerebral auditory centers. It can be classified as a Sudden Sensorineural Hearing Loss (SNHL) which is most often defined as the loss of 30dB or more, in at least three contiguous frequencies over a 72-hour span [1, 2]. But it can also be any hearing loss where the hearing thresholds are increased > 20 dB, without any identifiable transmissional component. The etiology is still subject to debate, with 85% of cases being classified as idiopathic [3]. The remaining 15% of cases are divided amongst infectious causes (viral), immune-mediated and finally micro-circulatory compromise [3]. A vascular etiology may be obstructive or hemorrhagic; both are rare [4,5]. Experimental animal models of venous occlusion have demonstrated hemorrhage in the perilymphatic and endolymphatic spaces [6]. There a few studies on the matter; Kaya et al. suggest a link between intralabyrinthine hemorrhage, hydrops and damage to inner ear structures. In their study, they compared the histopathological findings of temporal bones where unilateral intralabyrinthine hemorrhage had occurred with the normal contralateral side. They discovered significant decrease in the number of hair cells, spiral ganglions cells and fibrocytes in the striavascularis and spiral ligament on the side if the intra-cochlear hemorrhage [7].
MRI is frequently used in the evaluation of SNHL allowing, compared to other imaging techniques, to identify different causes of SNHL such as labyrinthitis, multiple sclerosis, cerebello-pontine angle or internal auditory canal tumors, stroke or hemorrhage. We here with present a case of non-traumatic spontaneous, intra cochlear hemorrhage in a patient with SNHL.
CASE PRESENTATION
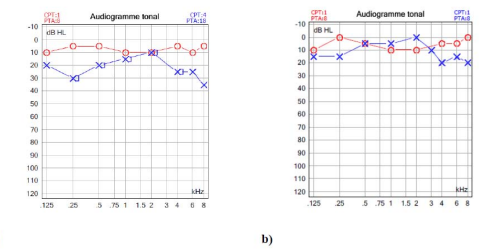
A 32 year old otherwise healthy female patient presented in August 2014 with left sudden hearing loss associated to a sensation of a blocked ear. Otherwise the history was uneventful, revealing no vestibular complaints, other co-morbidities or causative events. The physical examination revealed a lateralized tuning fork test (Weber) to the healthy, right ear and an otherwise normal neuro-otological examination. The audiogram revealed an isolated, left SNHL (Figure 1a).
Figure 1: The pure tone audiogram at initial stage (a) shows a SNHL at high and low frequencies and an almost complete normalization 3 months later (b).
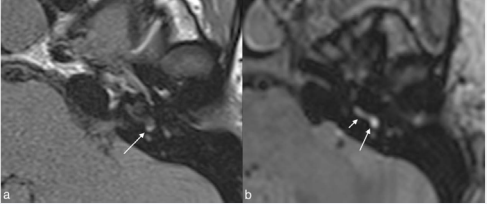
The patient received Prednisone orally for ten days. An MRI study 10 days after the onset of hearing loss showed on T1 weighted and 3D fluid- attenuated inversion recovery (FLAIR) images a 3mm large area of increased signal intensity at the inferior portion of the vestibule in vicinity of the oval window and in the basal turn of the cochlea (Figure 2).
Figure 2: Initial MRI. (a) T1- weighted image and (b) 3D FLAIR image show a high signal in the inferior vestibule (long arrows) close to the oval window and in the basal turn of the cochlea (short arrow). Note that the conspicuity of this high signal is better on FLAIR as on T1 and the degree of involvement appears to be larger on FLAIR as on T1.
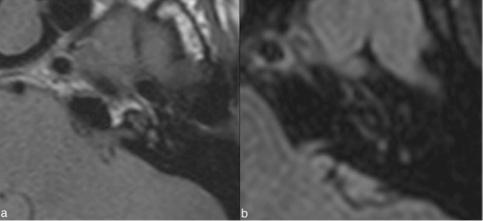
No other abnormalities were found, in particular no enhancement after IV administration of gadolinium chelates. The diagnosis of intra-cochlear hemorrhage was made and a thorough hematological analysis was performed, which turned out normal. Over the next 2 months, hearing recovered (Figure 1b) and follow-up MRI obtained 3 months after the initial MRI returned to normal (Figure 3).
Figure 3: MRI obtained 3 months later. (a) T1-weighted image and (b) 3D FLAIR image show complete resolution of the high signal intensity areas seen on the initial MRI.
DISCUSSION
Non-traumatic, spontaneous intra-labyrinthine bleeding is a rare cause of SNHL. According to Salome and al., vascular causes of SNHL can be classified into hemorrhagic or obstructive, and are frequently the expression of an underlying hematological disease or anti-coagulation [4]. Bleeding into the membranous labyrinth may lead to high concentrations of blood ageing products either at a single or at multiple subsites. The most commonly affected sub sites are the basal turn of the cochlea and the vestibule close to the oval window [4], as seen in our case. Bleeding into the semicircular canals or middle turn of the cochlea has equally been reported [4]. Depending on the time lapse between the acute event and imaging and depending on the concentration of the different blood products, in particular intracellular and extracellular methemoglobin, the signal intensity on T1 and T2 weighted sequences may vary [3,9]. T1 Hyper intensity is usually caused by presence of fat, proteinaceous materials and methemoglobinemia, of which fat can be distinguished by suppression (eg: Lipomas) [8]. Intracochlear hemorrhage is distinguished by high signal intensity in T1 and FLAIR without enhancement on gadolinium injection. In the present case, we observed a high signal on FLAIR and T1 weighted images in the symptomatic ear corresponding to extracellular methemoglobin, while the signal intensity in the non-symptomatic ear was normal. The hemorrhage appeared larger on FLAIR as on the T1.
weighted image (Figure 2). The absence of contrast enhancement suggested no associated acute inflammation. Recently, it has been shown that 3D FLAIR imaging is more sensitive than any other MRI sequence for the detection of intra-labyrinthine hemorrhage, as shown in our case [4]. Further in line with the literature [4], we found a good correlation between the clinical symptom of isolated, SNHL and the abnormal MRI signal of the basal cochlear turn. Only the small loss in the low frequencies could not be fully explained with the MR imaging, but may be related to the obstruction of the intra cochlear fluid movements due to the presence of blood clots.
CONCLUSION
weighted image (Figure 2). The absence of contrast enhancement suggested no associated acute inflammation. Recently, it has been shown that 3D FLAIR imaging is more sensitive than any other MRI sequence for the detection of intra-labyrinthine hemorrhage, as shown in our case [4]. Further in line with the literature [4], we found a good correlation between the clinical symptom of isolated, SNHL and the abnormal MRI signal of the basal cochlear turn. Only the small loss in the low frequencies could not be fully explained with the MR imaging, but may be related to the obstruction of the intra cochlear fluid movements due to the presence of blood clots.