Temporomandibular Joint Ankylosis after a Preauricular Abscess in a Young Child: A Case Report
- 1. Department of Otorhinolaryngology Head and Neck Surgery, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Malaysia
- 2. Department of Oral & Maxillofacial, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Malaysia
- 3. Institute of Ear, Hearing and Speech (Institute-HEARS), Universiti Kebangsaan Malaysia (UKM), Malaysia
ABSTRACT
Introduction: Retronagthia is a condition in which either or both jaws recede with respect to the frontal plane of the forehead. One of the causes of retronagthia is temporomandibular joint (TMJ) ankylosis that might results from trauma, infection and inadequate surgical treatment of the condylar area.
Report: We report a case of 3year- 8month old girl presented with progressively worsening retronagthia with the underlying history of left preauricular abscess without preauricular sinus or ear infection at 1 week of life. It was treated by needle aspiration and antibiotic in another centre. Upon clinical assessment, she had severe retronagthia, malocclusion and limited mouth opening with maximum 2mm interincisal distance. CT scan shows left temporomandibular joint ankylosis. Further assessment revealed she had moderate obstructive sleep apnea that required Non-invasive Continous Positive Airway Pressure (CPAP) support at home. Two-stage surgery was performed by Oral & Maxillofacial surgeons. The first stage included mandibular distraction osteogenesis, and second stage included left TMJ interpositional arthroplasty. Tracheostomy was performed by Otorhinolaryngology team concomitant during the first stage. One month after the second stage surgery, her mouth opening gradually improved to 20mm. Successful decannulation was achieved 2 months after the second surgery. Clinically her symptom of obstructive sleep apnea also improved and she did not require CPAP postoperatively.
Conclusions: Follow up for patient who had history of infection around the TMJ is necessary in order to detect TMJ ankylosis and provide appropriate management and early intervention.
KEYWORDS
Temporomandibular joint ankylosis, Preauricular abscess, Young child
CITATION
Ng R, Kong MH, Nabil S, Goh BS (2014) Temporomandibular Joint Ankylosis after a Preauricular Abscess in a Young Child: A Case Report. Ann Otolaryngol Rhinol 2(1): 1017.
ABBREVIATIONS
TMJ: Temporomandibular Joint; CPAP: Continuos Positive Airway Pressure; ORL: Otorhinolaryngology; Ukmmc; Universiti Kebangsaan Malaysia Medical Centre; OMS: Oral & Maxillofacial Surgeons; OSA: Obstructive Sleep Apnea; AHI: Apnea-Hyponea Index.
INTRODUCTION
Temporomandibular joint (TMJ) ankylosis can result from local or systemic infection and trauma. Congenital TMJ ankylosis usually arises from birth injuries [1]. Trauma is the commonest cause of TMJ ankylosis, which has the incidence ranges between 13% and 100%, and infective causes, can range from 0 to 53% [2]. Infection around the TMJ may lead to ankylosis of the joint [3]. Consequently, retrognathia of the mandible may develop in patients who are still growing. We report a case of left TMJ ankylosis of a 3year-8month old girl with neonatal history of ipsilateral preauricular abscess.
CASE PRESENTATION
A 3year-8month old girl, presented with worsening limited mouth opening since the age of 2 year-old and she required a longer time to complete each meal. Her mother also complained that her mouth opening becomes progressively limited over time. She also was noted to snore when sleeping and this worries her parents
Antenatal history was uneventful. She was born spontaneous full term via virginal delivery without instrumental aid. On 1 week of neonatal life, she developed left preauricular abscess and confirmed by ultrasound scan. There were no signs which suggestive of ear infection, no preauricular sinus opening seen. Needle aspiration was performed by Otorhinolaryngology (ORL) team in other medical centre and 3 cc of pus was drained and intravenous Benzyl Penicillin and Gentamycin were prescribed. No documentation was found regarding the condition of the Stensen’s duct opening, any systemic infection and also the culture and sensitivity results. She was discharged from ward with oral cloxacillin after 2 weeks of stay.
On subsequent follow up, she was noted to have reduced mouth opening, retrognathia and malocclusion at the age of two and half year old. After further investigation, she was then diagnosed to have left temporomandibular joint ankylosis. She was eventually referred to Oral & Maxillofacial Department Universiti Kebangsaan Malaysia Medical Centre (UKMMC) for further management at the age of 3year-8month.
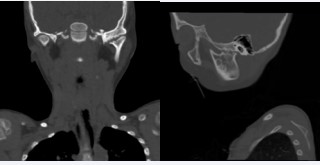
Upon assessment by oral & maxillofacial surgeons (OMS), she had severe retrognathic mandible, mandibular asymmetry, limited mouth opening with maximum of 2 mm interincisal distance and dental malocclusion. CT scan of head and neck was performed and showed left temporomandibular joint ankylosis. (Figure 1)
Figure 1: Pre-operative CT scan of the left temporomandibular joint (TMJ) ankylosis. Coronal view (left) and sagittal view (right) of CT scan showed obliteration of interarticular space and irregular articulating surface of left TMJ.
Besides that, she was assessed by ORL team and paediatric team, UKMMC and was found to have moderate Obstructive Sleep Apnea (OSA) with Apnea-Hyponea Index (AHI) of 8.9, adenoid hyperthrophy grade IV and bilateral tonsillar hypertrophy grade II. Non-Invasive Continuous Positive Airway Pressure was started every night until the first surgery.
Subsequently, two-stage surgery was performed. The first surgery was performed when the patient’s age was 5years and 3months. Tracheostomy under sedation was performed by ORL team prior to bilateral mandibular distraction osteogenesis operation by OMS. Four months later, left gap arthroplasty with interpositional temporalis myofascial flap, bilateral coronoidectomy and removal of mandibular distrator was performed by OMS. In the same sitting, ORL team performed adenoidectomy.
One month after the second stage surgery, her mouth opening gradually improved to 20mm interincisal distance (Figure 2).
Figure 2: Post-operative picture with good mouth opening.
Her tracheostomy was successfully decannulated 2 months after the second surgery. Clinically her symptom of obstructive sleep apnea also improved and she did not require CPAP postoperatively.
DISCUSSION
Temporomandibular joint ankylosis in children is rare, infection around the joint is one of the common cause. In this patient, preauricular abscess during neonatal period is most likely the contributing factor. A few case reports had been published in neonatal onset of preauricular abscess [4-6]
Zurina et. al. had reported parotid abscesses in neonates at the age of seventh day. Needle aspiration was required with concurrent intravenous antibiotic [4] Akgun et.al. and Schwab et. al. had also reported suppurative parotitis in neonates at the age of day three and day eight of life respectively. Both patients responded well to intravenous antibiotic and required no aspiration [5,6].
Septic arthritis of TMJ and knee joint in a neonate had been reported by Parmar et al [7]. Pus was drained from both joints and patient also required longer period of intravenous antibiotic compared to the above reported parotid abscess patient [7].TMJ ankylosis is one of the complication of TMJ septic arthritis [8]. In our case, the exact aetiology for the preauricular abscess was unable to be determined. However, both pathologies are possible. Infection around the TMJ area may lead to TMJ ankylosis as reported in this case.
CONCLUSION
Follow up for patient who had history of infection around the TMJ is necessary in order to detect TMJ ankylosis and provide appropriate management and early intervention. This action can reduce morbidity and also allow normal growth and development of a child.