Use of a Whiteboard for the Surgical Time-out in a Pediatric Setting
- 1. Division of Pediatric Otolaryngology, Advocate Children’s Hospital, USA
- 2. Rosalind Franklin University of Medicine and Science, North Chicago, USA
- 3. Feinberg School of Medicine and The Graduate School, Northwestern University, USA
ABSTRACT
Introduction: In order to further improve patient safety, our goal was to evaluate the use of a whiteboard in the operating room (OR) as a means to improve the participation, effectiveness, and focus in the time-out process.
Methods: A pilot study applying the use of the whiteboard during the time-out process was conducted on a cohort of pediatric otolaryngology patients’ procedures. A survey then evaluated each OR team member as to their perceptions of the benefit or lack of benefit of the whiteboard in the time out process.
Results: Our findings suggest the use of a whiteboard in our operating rooms leads to a perceived improvement in the time-out process. The whiteboard may serve as a focal point to highlight the key features of the surgical procedure in addition to encouraging focused participation by the OR team.
Conclusion: The addition of a whiteboard in the operating room for the time-out process is a tool that may improve the time out process and potentially lead to enhanced patient safety
CITATION
Walner DL, Popova Y, Woods D, Walner EG (2022) Use of a Whiteboard for the Surgical Time-out in a Pediatric Setting. Ann Otolaryngol Rhinol 9(3): 1291.
INTRODUCTION
Communication in the Operating Room (OR) setting is essential to optimize patient safety and eliminate errors. The surgical time-out is utilized in the majority if not all operating rooms in the US with the goal to improve communication, ultimately leading to improved patient safety. However, a commonly reported problem with the surgical time-out process is the lack of engagement or attention of the OR staff. A poorly performed time-out defeats the purpose of the exercise and increases the risk of patient harm. Errors and near misses can occur if vital information is not available or mistaken.
There is a need for further improvement in the time-out process as we strive for zero harm in surgical patients. Some hospitals utilize a whiteboard in their ORs while others do not. The theoretical benefits of the whiteboard include a visually redundant reminder and rapid reference tool for all providers in the OR with regards to vital pieces of information about the patient and surgical procedure. In addition, the whiteboard serves as a focal point during the time-out process to improve attentiveness and participation. Few studies exist on the use and potential benefits of a whiteboard in the OR.
This pilot study evaluated the use of a whiteboard on the perceived attentiveness and communication of the operating room staff as an area of improvement to provide a focal point and visual representation/ reminder about key elements of the patient, procedure, potential risks, and providers.
METHODS
A comprehensive literature review of ongoing issues and barriers with the time-out process was performed. An additional literature review was performed to learn more about the previous use of whiteboards in the operating room setting, with regards to the time-out process. A pilot study was then developed at our institution to involve a workflow change in the time-out process, utilizing a whiteboard in our ORs for pediatric otolaryngology procedures (Table 1).
Table 1: Operating Room Time-Out Workflow/ Steps.
|
1. Surgeon and nurse meet with patient and family in the pre-operative area to sign off on the WHO form and sign the consent form |
|
2. Circulating nurse completes the information on the whiteboard in the operating room prior to transport |
|
3. Child enters the room and general anesthesia is induced |
|
4. Before incision a time-out is performed |
|
5. The circulating nurse announces that we will start the time-out |
|
6. All people in the operating room attend to the time-out process (without distraction) |
|
7. Each person in the operating room introduces themselves by name and title |
|
8. Everyone’s attention is focused to the whiteboard and each other |
|
9. The circulating nurse confirms the patients name from the chart and wrist band |
|
10. The surgeon verbalizes the procedure that is scheduled |
|
11. The anesthesiologist comments on any anesthetic concerns and drug allergies |
|
12. The scrub nurse or technician comments and any special supplies or equipment that are needed |
|
13. The surgeon then asks if all caregivers are in agreement and if there any additional thoughts, questions or concerns before starting the procedure |
|
14. When all are in agreement the procedure commences |
The process was evaluated with a real-time survey of operating room personnel about the use of the board and the perceived benefits or lack of benefit of the whiteboard (Table 2).
Table 2: Provider Survey.
|
Have you had experience with the use of a whiteboard in the OR in the past? (circle one) |
|
|
|
Yes |
No |
|
|
If you used a whiteboard in the OR in the past, was it helpful for patient care/ safety? (circle one) |
||
|
Yes |
No |
Never used one |
|
3. In using the whiteboard today, did you find it improved patient care / safety? (circle one) |
||
|
Yes |
No |
Somewhat |
|
4. What positives came out of using the whiteboard today? (circle all that apply) |
||
|
Improved attention in the OR to the time-out |
|
|
|
Improved accuracy of Patient ID/ Patient Weight/ Allergies/ Planned Procedure |
|
|
|
Improved teamwork |
|
|
|
Other: |
|
|
|
No positives came out of using the whiteboard today |
|
|
|
5. What negatives were involved with use of the whiteboard today? (circle all that apply) |
||
|
It wasted time |
|
|
|
It was a hassle for the circulating nurse |
|
|
|
It was not accurate |
|
|
|
Other: |
|
|
|
No negatives came out of using the White board today |
||
The project was conducted in an ambulatory surgery unit. The surgical unit performs approximately 3400 surgical cases per year; approximately 50% on children (<18 years of age). The pilot study was conducted on a cohort of randomly selected pediatric otolaryngology operative procedures over 8 weeks. The study group/ sample size included three fellowship-trained pediatric otolaryngologists, various fellowship-trained pediatric anesthesiologists, operating room nurses, certified surgical technicians (CST’s), and our pediatric otolaryngology nurse navigator who collected and compiled the data.
We implemented the use of a whiteboard and acquired data over two months for random Pediatric Otolaryngology same day procedures performed by the pediatric otolaryngology service. A survey was individually completed by all operating personnel on the day they were first participating in the new whiteboard time out process. Each person was only allowed to complete a single survey after evaluating the process on a minimum of three consecutive operating room cases. A total of 30 surgical cases were evaluated. All data from the surveys were tabulated and reviewed.
The whiteboards already existed in the ORs in our surgical unit, however, these were rarely previously utilized, so no cost was incurred. Patient demographics, operating personnel, and key items were standard on the whiteboard (Table 3).
Table 3: Whiteboard Information.
|
Patient Name: |
|
Date of Birth: |
|
Patient Weight (kg): |
|
Drug Allergies: |
|
Planned Procedure: |
|
Surgeon: |
|
Anesthesia: |
|
Scrub: |
|
Circulator: |
|
Special Equipment needed: |
|
Antibiotics needed/ given: |
|
Other pertinent information: |
IRB approval was obtained for this study.
RESULTS
Twenty-three individuals participated in our study (3 surgeons, 6 anesthesiologists, 9 circulating nurses, and 5 CST’s).
Sixteen out of 23 (70%) had prior experience with a whiteboard (likely at other institutions). Our study found an overwhelmingly positive perception benefit with the utilization of the whiteboard in the operating room (Table 4).
Table 4: Survey Response Data.
|
Question # |
Question |
Response |
Surgeon (n = 3) |
Anesthesia (n = 6) |
RN (n = 9) |
CST (n = 5) |
|
1 |
Have you had experience with the use of a whiteboard in the OR in the past? |
Yes |
3 |
6 |
5 |
2 |
|
No |
0 |
0 |
4 |
3 |
||
|
2 |
If you used a whiteboard in the OR in the past, was it helpful for patient care/safety? |
Yes |
3 |
6 |
5 |
2 |
|
No |
0 |
0 |
0 |
0 |
||
|
Never used one |
0 |
0 |
4 |
3 |
||
|
3 |
In using the whiteboard today, did you find it improved patient care/safety/ communication? |
Yes |
2 |
4 |
5 |
4 |
|
No |
1 |
1 |
2 |
0 |
||
|
Somewhat |
0 |
1 |
2 |
1 |
||
|
4 |
What positives came out of using the white board today? |
Improved attention in the OR to the time out |
2 |
4 |
3 |
5 |
|
Improved accuracy of patient ID/ patient weight/allergies/planned procedure |
3 |
3 |
6 |
5 |
||
|
Improved teamwork |
|
|
|
|
||
|
No positives came out of using the whiteboard today |
2 |
1 |
5 |
4 |
||
|
5 |
What negatives were involved with the use of the whiteboard today? |
It wasted time |
0 |
0 |
1 |
0 |
|
It was a hassle for the circulating nurse |
0 |
0 |
4 |
3 |
||
|
It was not accurate |
0 |
0 |
1 |
0 |
||
|
Redundant information |
1 |
0 |
0 |
0 |
||
|
No negatives came out of using the whiteboard today |
2 |
6 |
5 |
2 |
OR= Operating room, RN= Registered Nurse, CST= Certified Surgical Technician
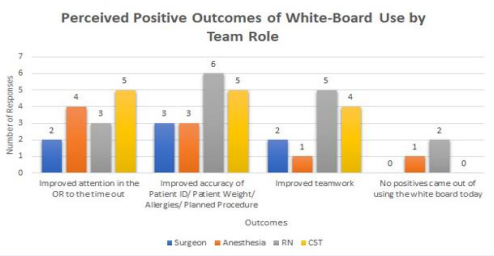
All 16 who had previously used a whiteboard in the time-out process believed the whiteboard was a helpful tool in the OR. Surgeons and anesthesiologists had greater prior familiarity with the whiteboard as compared to nurses and CST’s. After using the whiteboard in our hospital OR for a minimum of three cases, 19 out of 23 (82.6%) felt it improved or somewhat improved patient care, safety and communication. The perceived benefits include improved attention to the timeout process (61.0% of providers), improved accuracy of patient identification/ weight/ allergies/ planned procedure (73.9% of providers), and improved teamwork (52.2% of providers) (Figure 1).
Figure 1: Graphic representation of survey results on the perceived positive aspects of the whiteboard by team role.
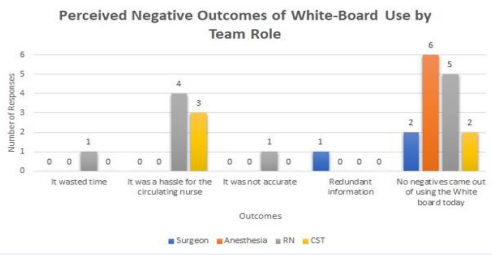
Perceived negatives from the use of the whiteboard included the following comments: it wasted time (reported by 1 nurse), was a hassle for the circulating nurse (reported by 4 nurses and 3 CST’s), was not accurate (reported by 1 nurse), and was redundant (reported by 1 surgeon). However, 15/23 (65.2%) did not identify any negatives from the use of the whiteboard (Figure 2).
Figure 2: Graphic representation of survey results on the perceived negative aspects of the whiteboard by team role.
DISCUSSION
Approximately 234 million surgical procedures are performed globally each year with about 20-50 million occurring in the United States each year [1,2]. In industrialized countries, it is estimated that the peri-operative death rate from inpatient surgery is between 0.4-0.8% or 1 in 250 with a major complication rate between 3-17% [1]. Furthermore, it is estimated that 50% of surgical complications are avoidable [3]. Based on an AHRQsupported study between 1985 and 2004 approximately 1 per 113,000 operations involved a wrong-site surgery [4].
Overall, our study results suggested that 82.6% of the providers felt that the use of the whiteboard improved patient care, safety, and communication, improved attention in the operating room toward the time-out process as well as improved the accuracy of presenting the patient demographics, allergies, and planned procedure. The majority believed it also improved teamwork in the operating room. Only 13% felt there were no positives provided by the use of the whiteboard.
In 2003, the Joint Commission’s Board of Commissioners approved the original Universal Protocol for Preventing Wrong Site, Wrong Procedure, and Wrong Person Surgery for all accredited hospitals, ambulatory care centers, and office-based facilities [5]. The Joint Commission’s Universal Protocol dictated three consistent checkpoints: 1) preoperative verification and reconciliation, 2) site marking, and 3) a time-out immediately before starting the procedure.
A systematic review of safety checklists in the operating room suggests that the checklists do improve the perceived quality of operating room personnel teamwork and communication and reduce observable errors related to poor team skills. However, the review also suggests that when used sub-optimally or when individuals have not bought into the process, the checklists may harm the function of the team [6]. The review suggests that further research should aim to better understand the relationship between how safety checklists are used and team skills in the OR using more methodological approaches and validated measures of teamwork to develop best practice guidelines.
Communication breakdown is often reported as one of the major factors and has been implicated in nearly 80% of wrongsite sentinel events [7,8]. Operating room communication and teamwork defects leading to errors in care arise from situations when distractions or rushing occur during the time-out process and when the time-out is performed without full participation leading to missing key relevant clinical and patient identification information in the care of these patients [9].
Team-based group communications using checklists are widely recommended and acknowledged to achieve improvement in the shared understanding of the surgical clinical team and to improve patient safety. Team participation in effective time-out processes depends on multiple factors including team attributes, communication strategies, and checking processes [10]. Surgical checklists have provided many benefits, however, barriers to sustained use include haphazard introductions, perceived duplication or redundancy of information, competing demands, professional identification, and team culture. The study by Gillespie highlighted how some participants saw the surgical safety checklist as a “tick-n-flick’ exercise leading to complacency because team members were simply ‘going through the motions’ without listening to or thinking about the information being collected. In other studies looking to reduce errors, the use of redundancy and a cross-team check have been found to be beneficial [11].
A reliable team must possess the ability to adapt to changes within the work environment, maintain open and flexible communication, and anticipate the needs of each team member [12]. Clinical staff members failing to speak up during a timeout increases the risk of wrong-site surgery and errors [13]. Developing a method to encourage participation and discussion from all team members is vital to improving the process. Assigning roles to ensure every team member actively participates in the time-out has been suggested to improve communication and teamwork [14].
Both the National Academy of Medicine and The Joint Commission have cited the lack of teamwork as a principal cause of inefficiency and medical error in the OR and highlighted improved communication as a major priority in this arena [15]. Other studies have suggested that compliance with surgical checklists is influenced by the perceived importance or unimportance of individual items contained in the list [16].
The whiteboard is a low-cost solution that can be implemented in any procedure-related setting. The visual representation concept can also be implemented in an electronic form separately or incorporated into an electronic medical record. The utilization of whiteboards in the OR occurs in some institutions, however, limited data has been published on the benefits of its use. In 2010, a group studied the use of a whiteboard in the operating room to determine if it improved memory retention among members of the surgical team. They found that the visual stimulus in addition to the verbal stimulus in the time-out process increased team retention of patient identifiers from 67% to 82% [17]. A team in Nashville implemented the use of an electronic whiteboard and was able to improve compliance with the time-out process from 49% to 81% [18]. Another study found that the use of the whiteboard in the OR showed improvement in operating room dynamics, flow, efficiency, involvement, and preparedness [19]. The whiteboard was also felt to “flatten” the traditional OR hierarchy creating an environment where all members of the team feel more comfortable and empowered to speak up when it is needed; a key component of improving patient safety in medicine. A study from UCLA utilized a whiteboard and an “extended surgical time-out” and found that the process resulted in improved communication without disruption of workflow. However, in this study utilizing a whiteboard as part of the timeout process did not completely eliminate wrong-site surgery [20]. The process was found to increase operating room staff’s perception of active involvement in improving patient safety from 55% to 95%. The Pennsylvania Patient Safety Authority commented on a potential flaw in the use of the whiteboard if the board was not being routinely updated between cases leading to a source of incorrect information and the potential for error [21]. A group in Tennessee created an electronic system using intraoperative electronic documentation to create and present a time-out checklist on a large operating room display. This study reported that after an implementation cost of $34,000, they found more rapid completion of checklist tasks and suggested an 84% probability of lowering wrong-site surgery [22].
A great benefit of the whiteboard involves the visual representation that is used to center the attention and encourage active participation of the entire OR team at the moment of the time-out exercise. In addition, it was found that the visual representation of the time-out was also powerful as a visual reference for the team across the entire duration of the surgical procedure; regardless of shift changes or other factors.
Team dynamics and human factors are essential to the development and sustainability of a highly functioning surgical team. Crew Resource Management (CRM) and use of the TeamSTEPPS are tools that can enhance communication and teamwork [23,24]. Team learning is an essential component to having a systems approach as a “learning organization” [25]. Simulation training is another tool that can be utilized to enhance the process. These tools and others can be utilized along with and in addition to the whiteboard concept to optimize OR safety. Based on our review of the literature and pilot study, the use of the whiteboard in the operating room setting will certainly create another barrier to the potential for patient harm, while not completely eliminating the potential for operating room errors. Further investigation of this process is warranted and can be incorporated into electronic boards as well.
STUDY LIMITATIONS
Our study was performed on pediatric patients, and thus all time-out procedures were performed after the child was asleep under general anesthesia. The process and evaluation may be different in an adult operating room setting when the initial phase of the time-out may be performed with the patient awake. In addition, the study was only performed on elective pediatric otolaryngology cases and did not include emergent or trauma cases. As a pilot study, only a small sample size was evaluated. The pediatric otolaryngology cases evaluated in our study tend to be relatively fast (<1 hour) and back to back with other procedures of similar type, so findings in our study may not apply to all surgical specialties. Evaluation of the use of the whiteboard on morbidity and mortality was not feasible in the study period.
As we move forward, potential problems identified with continued use of the whiteboard may include updating the whiteboard information between cases and assigning this task to circulating nurses who may not welcome further responsibilities. Developing a culture of safety first will help implement new processes and encourage participation. If the whiteboard program is expanded at our institution or others, it likely will require an educational program highlighting the importance of the whiteboard for patient safety and will need to include all involved providers to achieve buy-in and success.
CONCLUSION
Teamwork remains the hallmark of every successful and harmfree surgery. In the operating room, surgeons, anesthesiologists, nursing staff, and scrub technicians must continuously interact and collaborate to navigate a variety of challenges together. The team works to ensure the correct patient, site, side, and type of surgery to be performed, appropriate consents, and identification of any patient allergies, while also managing anesthetic demands, comorbidities, positioning, technical complexity, and personal safety in a time-constrained highly stressful environment. The time-out procedure using a visual representation in the form of a whiteboard is an effective tool to improve intraoperative team communication, efficiency, and workflow while verifying patient information and optimizing resource utilization which has been shown to improve patient outcome and diminish the risks of harm.
Our pilot study found an overwhelmingly positive (82.6%) perception of improved patient care, safety, and cross-team communication with the use of the whiteboard in the operating room setting of our hospital.
REFERENCES
- Haynes AB, Wiser TG, Berry WR, Lipsitz SR, Breizat AS, Dellinger EP, et al. A Surgical Checklist to Reduce Morbidity and Mortality in a Global Population. N Engl J Med. 2009; 360: 391-499.
- Gaba DM. Anaesthesiology as a model for patient safety in health care. BMJ. 2000; 320: 785-788.
- Kable AK, Gibberd RW, Spigelman AD, et al. Adverse events in surgical patients in Australia. Int J Qual Health Care. 2002; 14: 269-276.
- AHRQ Patient Safety Network. 2003.
- The Joint Commission on Accreditation of Healthcare Organizations. Comprehensive Accreditation Manual for Hospitals. Glossary. Oakbrook Terrace, IL. 2017.
- Russ S, Rout S, Sevdalis N, Moorthy K, Darzi A, Vincent C, et al. Do Safety Checklists improve teamwork and communication in the Operating Room? Ann Surg. 2013; 258: 856-871.
- Dagi TF, Berguer R, Moore S, Reines HD. Preventable errors in the operating room-part 2. Curr Probl Surg. 2007; 44: 352-381.
- Cohen SP, Hayek SM, Datta S, Bajwa ZH, Larkin TM, Griffith S. Incidence and root cause analysis of wrong-site pain management procedures: a multicenter study. Anesthesiology 2010; 112: 711-718.
- Health Research and Education Trust and Joint Commission Center for Transforming Healthcare. Reducing the risks of wrong-site surgery: Safety practices from The Joint Commission Center for Transforming Healthcare Project. Chicago, IL 2014.
- Gillespie BM, Withers TK, Lavin J, Gardiner T, Marshall AP. Factors that drive team participation in surgical safety checks: a prospective study. Patient Saf Surg. 2016; 10: 3: 1-9.
- Ong MS, Coiera E. Safety through redundancy. Qual Saf Health Care, 2010; 19: e32.
- Lerner S, Magrane D, Friedman E. Teaching teamwork in medical education. Mt Sinai J Med. 2009; 76: 318-329.
- Abecassis ZA, McElroy LM, Patel RM,Khorzad R, Carroll C, Mehrotra S. Applying fault tree analysis to the prevention of wrong site surgery. J Surg Res. 2015;193: 88-94.
- Smith C. 5 Takeaways for surgical time out success. Becker’s Hospital Review. 2013.
- Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res, 2006;41: 1576-1598.
- Ziman R, Espin S, Grant RE, Kitto S. Looking beyond the checklist: An ethnography of interprofessional operating room safety cultures. Journ Interprof Care 2018;32: 575-583.
- Goodman A. White board in the OR add layer of Safety. Chest Physician, 2015.
- Mainthia R, Lockney T, Zotov A, France DJ, Bennett M, St Jacques PJ, et al. Novel use of electronic whiteboard in the operating room increases surgical team compliance with per-incision safety practices. Surgery 2012; 151: 660-666.
- Sharma K, Morgan A, Stroud J, Mackinnon SE. The Whiteboard Technique, Personalized communication to improve operating room teamwork. Ann Surg 2018; 268: 225-227.
- Lee SL. The extended surgical time out: does it improve quality and prevent wrong-site surgery? The Permanente Journal 2010; 14: 19-23.
- Clarke JR, Waddell L, et al. Quarterly update on wrong site surgery: how to do an effective time out in the dark. Pennsylvania Patient Safety Authority. 2014;11: 88-92.
- Rothman BS, Shotwell MS, Beebe R, Wanderer JP, Ehrenfeld JM, Patel N, et al. Electronically mediated time out initiative to reduce the incidence of wrong surgery. Anesthesiology. 2016; 125: 484-494.
- Wakeman D, Langham MR. Creating a safer operating room: Groups, team dynamics and crew resource management principles. Seminars in Ped Surg. 2018; 27: 107-113.
- AHRQ TeamSTEPPS. Agency for Healthcare Research and Quality. TeamSTEPPS 2.0. 2017.
- Eisenberg JM. Continuing education meets the learning organization: the challenge of a systems approach to patient safety. J Contin Educ Health Prof. 2000; 20: 197-207.