Identifying Barriers and Decision Making for Breast Cancer Screening Among Black Caribbean Women by Using Clustering and Cart Methods
- 1. Department of Epidemiology, Florida International University, Robert Stempel College of Public Health and Social Work, United States
- 2. Department of Biostatistics, Florida International University, Robert Stempel College of Public Health and Social Work, United States
- 3. Department of Health Promotion and Disease Prevention, Florida International University, Robert Stempel College of Public Health and Social Work, United States
- 4. Department of Global and Sociocultural Studies, Florida International University, Steven J Green School of International & Public Affairs, United States
Abstract
Breast cancer is the most common form of cancer among women worldwide. Mammography is the only viable and effective, most used method for breast cancer screening, with recommendations being updated based on newly acquired knowledge. It is well-documented that Black women have higher incidence rates of breast cancer and are more likely to be diagnosed with late stage of the disease and worse health outcomes. Black Caribbean women especially have even more late-stage diagnoses and higher mortality rates. The purpose of this study is to identify barriers to breast cancer screening and the decision-making patterns in health-seeking behaviors among Black Caribbean women living in South Florida and using the identified needs to recommend possible solutions to address their needs. Using secondary data from a cross-sectional survey, descriptive analyses were performed, followed by Dendrograms for identifying cluster of barriers and Classification and Regression Trees for exploring the women’s decision-making process for screening. Five clusters were identified amongst the 124 self-identified Black Caribbean women: Healthcare and Cultural Beliefs, Barriers, Healthcare Seeking, Age, and Geographical Location. The Classification and Regression Trees recognized decision making in healthcare seeking practice indicating physician’s recommendations, and age as the main influencers for screening adherence. There is a need to increase awareness and knowledge about breast cancer screenings and overall female reproductive health and develop an appropriate, culturally sensitive screening programs to address these needs.
Keyword
Breast Cancer, Black Caribbean, Women, Health Disparities, Epidemiology
CITATION
Rodriguez AD, Veledar E, Rojas P, Tardanico R, Pekovic V, et al. (2023) Identifying Barriers and Decision Making for Breast Cancer Screening Among Black Caribbean Women by Using Clustering and Cart Methods. Ann Breast Cancer Res 7(1): 1023.
INTRODUCTION
Globally, over 7.8 million women live with breast cancer, making it the most prevalent cancer amongst women [1]. Recent data showed the annual incidence of breast cancer was 2.3 million new diagnoses and 685,000 deaths in 2020 [1]. In the United States, breast cancer also ranks top common cancer amongst women, besides skin cancers [2]. It is estimated that for the year 2023, there will be approximately 350,000 new cases of breast cancer and an estimated 43,000 deaths in the USA [2]. The probability of being diagnosed with breast cancer increased globally for women from 1 in 11 (9.1%) in 1975 to 1 in 8 in (12.5%) 2011 [3]. Studies have found that breast cancer incidence and mortality rates differ greatly based on race and ethnicity of the women [3]. Although Non-Hispanic White women have higher incidence rate of breast cancer when compared with Black women, mortality rates are 40% higher amongst Black women than non-Hispanic White women [4,5]. Regardless of race and ethnicity, the five-year survival rates for stage 0 or I are almost 100% compared with those diagnosed at stage IV 22% [6]. It is well-documented that higher morbidity and mortality rates along with higher late-stage diagnoses are associated with low screening rates [7].
Mammography is the only feasible and effective procedure for breast cancer screening. According to the American Cancer Society (ACS), women aged 45-54, who are of average risk for breast cancer, should undergo a mammography every year while women who are at high risk should get a breast Magnetic Resonance Imaging (MRI) along with a mammography annually starting by age 30 [8]. Early detection through screenings is one of the best approaches for prevention [9].
Since the early 2000s, breast cancer incidence rates have increased annually by 0.5% [10]. Race-ethnicity played a noticeable role in this regard. Non-Hispanic White and non Hispanic Black women have higher incidence of breast cancer when compared to women of other racial and ethnic backgrounds, and incidence of breast cancer before age 45 is higher for nonHispanic Black women than non-Hispanic White women [3,11]. Black women are disproportionally diagnosed with more aggressive forms of breast cancer as well as diagnosed at much more advanced stages than any other race/ethnicity [11,12]. Mortality rates are 42% higher in Black women than White women and, Black women have lower 5-year survival rates when compared to White women, 83% vs 92% respectively [10,11].
When looking at Black women living in the US, Black Caribbean women receive breast cancer screenings at much lower rates than US-born Black women [13]. Furthermore, Black Caribbean born women are more likely to be diagnosed with breast cancer at a younger age when compared to US-born Black women [14].
Numerous studies have investigated the ethnic differences amongst Blacks and Whites; however, very limited studies have studied the variations within Black subgroups, particularly Black Caribbean women. Black women should not be treated as a monolithic group as one in ten Blacks in the US is foreignborn, with the immigration population is expected to reach 36% by 2065 [15,16]. Unfortunately, in high-concentrated Black Caribbean zip codes, late-stage diagnosis and mortality statistics are significantly high too [17]. It is imperative to address the differential burdens of breast cancer screenings among Black Caribbean women, hence this study aims to identify needs and decision-making patterns in heath-seeking behaviors and beliefs of Black Caribbean women living in South Florida in relation to utilization of the mammography as a tool for breast cancer screening.
METHODS
Measures
Secondary data from a cross-sectional survey was used for this study. The survey consisted of 105 yes/no, true/false, structured multiple-choice or open-ended questions. The questionnaire was developed based on literature, focus groups, and validated questions from national surveys [13]. The questionnaires were self-administered, and no personally identifiable information was collected.
Prior to enrolling, participants were asked about their ancestry and their background, those who had Black Caribbean ancestry and/or identified as a Black Caribbean were enrolled. For this study, we analyzed questions focused on demographic and socio-economic factors, social support system, overall breast cancer knowledge, barriers to breast cancer screenings, and overall breast cancer screening practices.
Participants
The study consisted of 124 Black Caribbean women who resided in Broward County, Florida. IRB approval was obtained, and participants were provided consent forms. The participants were informed that their participation was voluntary, and any questions that they may find uncomfortable was at their discretion to answer. Participants were compensated for their time and those who declined to participate were provided an educational handout on cervical cancer prevention from the Centers for Disease Control and Prevention (CDC). The questionnaires were completed anonymously with no personally identifiable information collected.
Broward County is the second largest county and is an urban and industrialized county in Southeastern Florida. According to the US Census, Broward’s population is estimated to be 1,930,983, with 62.5% identifying as White, 32% identifying as Black or African American, and 31.1% identifying as Hispanic or Latino in 2021 [18]. West Indians (Black Caribbean) make up approximately 18% of the population, with Haitians and Jamaicans making up approximately 6% each, respectively; approximately 34% of the residents of Broward County are foreign-born [18].
Participants were recruited from community centers, such as religious centers, medical centers, medical offices, recreational centers, and other community-centered locations such as city hall in from January 2019 until April 2019.
Statistical
Methods All statistical analyses were conducted using IBM SPSS Statistics for Mac, version 27. The alpha level for statistical significance was set at 0.05. Frequencies and percentages were calculated for categorical variables, and means, medians, and standard deviations were calculated for continuous variables. Cross-tabulations and correlations were also conducted.
A dendrogram was created to visualize and comprehend screening behavior patterns amongst the study participants using clustering methods and Ward’s minimum variance methods. Classification and Regression Trees (CART) were constructed to describe any associations within the data and to provide visual representation of the decision-making patterns in relation to breast cancer screening practices and adherence. This method uses a machine learning algorithm that is used for prediction, creating a tree-like structure where each node represents a decision based on the Gini Impurity Index, a specifically identified predictor variable, and is continued for each branch tracing a possible outcome decision process [19]. The CART method is an appropriate method for this analysis not only because it is most likely to select independent variables that are different from the dependent variable, but it is best used to describe any associations within the data. Two CART were constructed for this study using the comparative variable Current vs. Not Current with Mammography, where current with mammography is defined as having undergone a mammography for the purpose of breast cancer screening within the past year.
RESULTS
Demographics
The study was comprised of 124 female participants with an average age of 49 (SD = 14.2). Self-identified African American/ Black represented approximately 45% of the sample, followed by other 34%. Of those who selected other for race/ethnicity, 15% identified as Guyanese and 11% identified as West Indian. The sample consisted of 24% participants born in the United States, 22% born in Trinidad & Tobago, 21% born in Guyana, and 33% born in other Caribbean islands (Table 1).
Breast Cancer Screening Practices
When asked about the time of their last mammography, 22% of participants had never received one while 49% had received one within the past two years. 6% of those who were under the age of 39 have never undergone a mammography screening when compared to 16% of those aged 40 and older. Additionally, those aged 40 and older were more likely to have undergone a mammography screening within the past year when compared to younger participants (42% vs 7%, respectively).
Several participants (74%) said their Primary Care Physician (PCP) recommended they receive mammography. Additionally, several participants (65%) said they first heard of mammography from their PCP. Most participants identified that their insurance covered mammography as part of their annual check-ups (71% and 87%, respectively).
Breast Cancer Knowledge and Beliefs
While over half of participants (52%) did not know the cause of breast cancer, most participants were able to identify risk factors and symptoms associated with breast cancer. A large majority of participants (88%) were able to identify family history of breast cancer as a risk factor for breast cancer. Of the six possible choices, 7% of participants were unable to identify any risk factors and 71% were unable to identify all commonly known risk factors. Finding a new lump in the breast or in the underarm was the most identified symptom of breast cancer (90%). Of the eight possible choices, 9% of participants were unable to identify any symptoms while 49% were unable to identify all common symptoms.
About 22% believe that a diagnoses of breast cancer was a death sentence. When asked if they believed breast cancer was a common cancer, 81% of participants agreed. Almost half of participants (45%) had family members who were diagnosed with cancer, of which breast cancer was the most common diagnoses (30%). A vast majority of participants did not believe that mammography screenings were against their cultural beliefs or their religious beliefs (92% and 93%, respectively). When asked if they believed that early detection of breast cancer meant increased chances of being cured as well as increased chances of living longer, most participants agreed (86% and 94%, respectively). Additionally, 91% of participants believed that there were effective treatments for breast cancer.
Dendrogram Findings
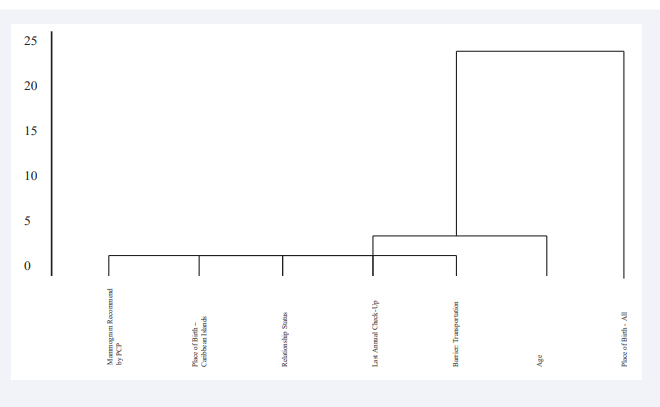
All predictor variables were included in the creation of the dendrogram, which produced five clusters with the first cluster containing the most variables (Figure 1).
Figure 1: Dendrogram of Predictor Variables.
The first cluster, Healthcare and Cultural Beliefs, consists of whether the mammography was recommended by their PCP, place of birth based on Caribbean islands, and their relationship status. The second cluster, Barriers, consists of whether transportation is a barrier to obtaining a mammography. The third cluster, Healthcare Seeking, consists of the time of their last annual check-up. The fourth cluster, Age, contains the age range. The fifth and final cluster, Geographical Location, consists of place of birth including the US and all the Caribbean islands (Table 2).
CART Findings
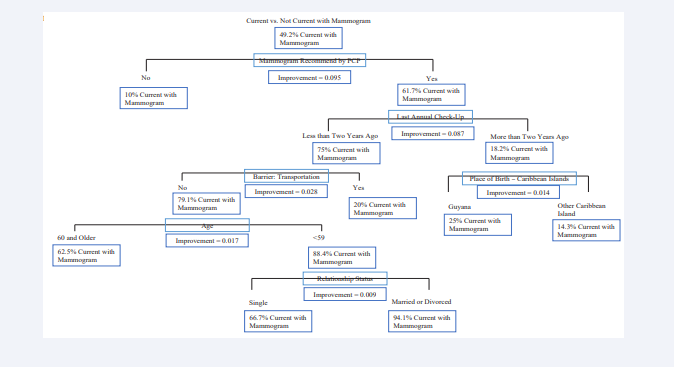
Two CARTs were constructed for this study using the same outcome variable, Current vs. Not Current with Mammography. The first CART included all the predictor variables (Figure 2).
Figure 2: Classification and Regression Tree using current vs. Not current with Mammogram as the Predictor Variable.
In this CART, the first variable of influence is whether their PCP recommended they undergo a mammography. For those who responded yes, time of their last annual check-up was most influential. Those who had an annual check-up more than two years ago were influenced by their place of birth in the Caribbean islands. For those who had an annual check-up less than two years ago, the barrier of transportation was most influential. For those who did not identify transportation, or lack thereof, as a barrier, their age was most influential. For those who were younger than 59, their relationship status was most influential.
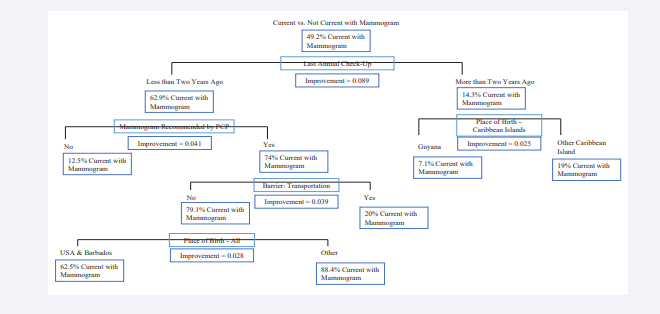
The second CART (Figure 3) included all the predictor variables, with the variable Age selected as the influencer variable.
Figure 3: Classification and Regression Tree using Current vs. Not current with Mammogram as the Predictor Variable, with Age as Influence
Time of last annual check-up was most influential. For those who had an annual check-up more than two years ago, place of birth in the Caribbean islands was most influential. For those who had an annual check-up less than two years ago, whether their PCP recommended they undergo a mammography was most influential. Those whose PCPs did recommend they undergo a mammography were influenced by whether they believed transportation to be a barrier. For those who did not identify transportation, or lack thereof, as a barrier, their place of birth overall was most influential.
DISCUSSION
The goal of this study was to contribute to the promotion of screening strategies for breast cancer among Black Caribbean women in the US. By examining demographic and socio-economic factors, social support system, overall breast cancer knowledge, barriers to mammography for breast cancer screening, and overall breast cancer screening practices, our results highlighted three themes: healthcare beliefs and utilization, age, and place of birth.
As previously mentioned, mammography is one of the methods for breast cancer screenings. It has been used to detect breast cancer since the mid-1960’s and has been associated with a 15-25% reduction in breast-cancer related deaths [14,20]. Using mammography as a screening tool for breast cancer targets to detect the disease at an earlier, more curable stage [21]. Many of the study participants believed that using mammography for early detection of breast cancer meant that there were increased chances of being cured and increased chances of living longer. Over time, however, recommendations have been updated to reflect changes in incidence and prevalence of breast cancer. Ultimately, the decision of when to start mammography is up to the physician. Most participants said that they first heard about mammography and their importance from their healthcare providers, most of which first heard of mammography from their primary care physician.
Risk factors for breast cancer have been extensively studied and identified, which include gender, age, family history, physical activity, obesity, and hormone influences such as age of first period and age of onset of menopause [22-24]. Hormonal influences have been shown to increase the probability of breast cancer development, particularly increased exposure to progesterone [25]. Most participants were able to identify that having family history of breast cancer as a risk factor, as well as not being physically active, being overweight, taking hormones and oral contraceptives, and being pregnant at a later age.
Age plays a major role in both breast cancer screening behavior and disease development. Prior studies have concluded that the risk for developing breast cancer increases with age [26]. As previously stated, the ACS recommends women undergo a mammography starting at age 40 unless they present greater risk for developing the disease. Several studies have identified that women are more likely to develop the disease after menopause, which can occur between 45 to 55 years of age [27]. Additionally, women who have their first period at a young age and women who are older than 50 at the start of menopause, are of increased risk for breast cancer [28]. Studies have found that Black women are diagnosed with breast cancer at an earlier age when compared to White women, 54 vs 61[29]. Additionally, Black women were found to be diagnosed at later stages of disease, regardless of age [30]. Our results showed that women aged 20-39 were more likely to have never received a mammography, while women who were 60 and older were both more likely to have received a mammography and to be following recommendations set forth by the governing bodies.
In addition to age, place of birth also appears to play a role in breast cancer knowledge and screening behaviors. When it comes to overall cancer knowledge and beliefs, one study found that Caribbean women were likely to have ill-perceived notions on breast cancer as well as incomplete knowledge on overall breast cancer risk factors [31]. Additionally, this study also found that misconceptions about breast cancer, including risk factors, negatively affected screening behavior [31]. Our study found that participants who were born in the US were more likely to have received a mammography at least once in their lifetime compared to Caribbean-born women. Our study also found that while most participants were able to correctly identify at least one risk factor for breast cancer, they were unable to identify the cause of breast cancer.
There are a few limitations associated with this study. Given the cross-sectional design of the study, follow-up with the participants to measure if the questionnaire prompted any new behaviors, such as more consistent screening practices or even improved communications with their healthcare providers was not feasible. The questionnaires were self-complete, which can lead to non-response bias as some questions may be uncomfortable for some participants to respond to, however, the anonymity and privacy provided to participants makes this unlikely. Furthermore, this is a convenient, snowball sample. The participants were recruited at local community centers where selection bias may have impacted recruitment and may not adequately represent the desired population. However, efforts had been made to recruit sample from ethnic grocery stores and low-income clinics to lower the bias. Despite possible limitations, these findings may stand as a useful contribution to addressing the gap in literature.
Our methods identified areas requiring improved intervention including increasing knowledge and awareness, understanding cultural influences, and sympathizing with age. This study has shown how healthcare seeking behavior and beliefs, along with age, and place of birth all play an active role in breast cancer screening behavior and overall breast cancer knowledge. Some studies have suggested incorporating intervention strategies at various levels including policy and healthcare such as promoting early detection [32,33]. However, few studies have researched the complexity of the social and cultural differences within racial and ethnic backgrounds and the role it plays when it comes to healthcare seeking behavior, this study can serve as the catalyst for further investigation.
CONCLUSION
Our study has found points of intervention when interpreting breast cancer screening behaviors amongst Black Caribbean women. Increasing awareness and knowledge as well as understanding how age affects behavior were observed as areas for improvement. Understanding healthcare-seeking patterns and promoting annual visits with primary care physicians also revealed to be imperative in promoting and increasing breast cancer screenings.
There is a need to create and implement appropriate, culturally sensitive screening programs and campaigns to increase awareness and knowledge about breast cancer screenings and overall female reproductive health. A user-friendly, multi-level approach is necessary to reach underserved women, all focusing on at-risk women, the clinicians that attend to them, and local public health officials. With the immigrant population expected to continue to rise exponentially, it is imperative that we create the tools and the proper environment for women of all cultural and social backgrounds to become informed about breast cancer and perhaps start to bridge the gap.
Funding Source
The seed funding was received from the Dean of Stempel of College of Public Health & Social Work (FIU Grant #2430020008). The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
REFERENCES
1. World Health Organization. Breast Cancer. 2023.
2. American Cancer Society. How Common Is Breast Cancer? 2023.
6. Fadi M Alkabban, Troy Ferguson. Breast cancer. Statpearls. 2022.
10. American Cancer Society. Cancer Facts & Figures 2023. 2023.
18. US Census Bureau quick facts: Broward County, Florida. United States Census Bureau. 2022.