A Rare Cause of Biliary Obstruction Caused by Egg of Fasciola Hepatica Mimicking Biliary Duct Stone or Rupture of Liver Hydatid Cyst
- 1. Department of Thoracic and general Surgery, Inflammatory Lung Diseases Research Center, Guilan University of Medical Sciences, Iran
- 2. Department of internal medicin, Gastero interology, Guilan University of Medical Sciences, Iran
- 3. Arya private Hospital, Guilan University of Medical Sciences, Iran
Abstract
Fasciola hepatica is an endemic parasitic disease in Iran and some countries in the world. The humans are accidentally infected by Fasciola in the life cycle. The definitive host is sheep. When human infected, The presentations are in two shape: acute or hepatic and chronic or biliary shape. When the flukes or eggs enter the bile ducts, cholestasis and cholangitis may present. These complications can be misdiagnosed from other cause of obstructive jaundice especially biliary stones. We present cases of fascioliasis, which present with sever colicky abdominal pain, jaundice and fever and was difficult to differentiate from gallstone or ruptured hydatid cyst in this patient. A 52-year-old man from north of Iran with history of hydatid cyst of liver, presented with severe colicky abdominal pain, fever, right upper quadrant pain and jaundice. Total bilirubin was 6 mg/dl, Direct bilirubin was 4 mg/dl ,aspartate aminotransferase 65 IU/L, alanine aminotransferase 75 IU/L, alkaline phosphatase 525 IU/L, .WBC =1400O with 40% eosinophilia .U&S show distended and edematous gallbladder wall and CBD diameter was 12 mm without stone. MRCP showed distention of gallbladder and filling defect and obstruction in the distal portion of CBD. ERCP with sphenctrommy was performed and multiple eggs were removed from the choledochus. The result of an indirect hemagglutination test for F. hepatica was 1/286 .General condition of patient was improved day to day.
In conclusion: The chronic phase of fasciola hepatica infection can be misdiagnosed as multiple other cause of obstructive jaundice. Thus, in endemic areas F. hepatica and hydatid cyst should be in the differential diagnosis of common bile duct obstruction and jaundice, MRCP and ERCP can help to diagnosis and treatment.
Keywords
- Fasciola hepatica
- Obstructive jaundice
- Hydatid cyst
- Endemic zoonotic infection
- MRCP
- ERCP
Citation
Aghajanzadeh M, Pirozi A, Gelali A, Kosha A, Mashor MY, et al. (2021) A Rare Cause of Biliary Obstruction Caused by Egg of Fasciola Hepatica Mimicking Biliary Duct Stone or Rupture of Liver Hydatid Cyst. Ann Clin Cytol Pathol 7(1): 1140.
INTRODUCTION
Fascioliasis is a zoonotic infection disease; the cause of this disease is Fasciola hepatica. Sheep and cattle are infected by this trematode [1,2]. In the life cycle of this parasite humans are accidentallly infected. Fasciola hepatica, that is rarely seen in Iran and some countries of world. Western Europe. Asia, Africa, and Latin America are the most common aria which involved. It is reported that 2.5 million people have been infected in 61 countries especially from Bolivia, Peru, Egypt, Iran, Portugal, and France [1- 3], In some report, approximately 2.4 million people are infected by Fasciola hepatica and 180 million people are at risk of infection by fascioliasis [1,4-6]. Infestation with F. hepatica present with variable clinical manifestations. In acute phase (hepatic), symptoms corresponding migration of larval stage from intestine and in chronic phase (biliary) symptoms are subclinical, and only intermittent cholangitis may be the prominent sign. In reports from 61 countary, Human hepatobiliary infection presents two phases: the acute (hepatic) and chronic (biliary) phases. The signs and symptoms of fascioliasis differ in the two phases. While fever, abdominal pain, headache, pruritus, urticaria, weight loss, and eosinophilia are seen in the acute phase, the chronic phase is usually asymptomatic [1,4,5,7,8]. However, F. hepatica may occasionally cause extrahepatic obstruction and cholestasis [7,8]. In our study, we present a case of fascioliasis that was difficult to differentiate from biliary duct stone or rupture of hydatid cyst, because in our case left lobe of liver involved by calcified stage 3 to 4 stage of liver hydatid cyst [1-4].
CASE PRESENTATION
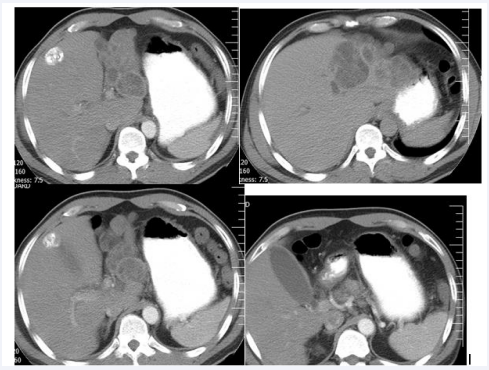
A 52-year-old man with history of previously hydatid cyst of left lobe of liver calcified stage 3 to4 stage presented to hospital with a two-day history of sever colicky abdominal , right upper quadrant pain and vomiting. Four year earlier, he had hydatid cyst of liver which treatment with albendasol and not increased the size of cyst but mild calcified present in the wall of cysts. On examination, he was alert and with scleral icterus. On abdominal examination, right upper quadrant and epigastric tenderness present. Patient complaint of dark urine. Other examination was normal. Laboratory liver tests showed , aspartate transaminase 153 [normal < 40] U/L, alanine transaminase 318 [normal < 41] U/L, alkaline phosphatase 554 [normal 38-126] U/L , amylaseand lipase were in normal range , total bilirubin was 6mg /li,direc bilirubin was 4mg mm /lt ,indirect was mm/lt 2.WBC=13500 with 40% eosinophilia. Abdominal ultrasonography showed a distended and edematous of gallbladder without stone, common bile duct was dilated (diameter was 12 mm). A computed tomography scan of the abdomen without contrast also showed multiple cyst with calcification of cysts wall and all were intact in left lobe of liver, gallbladder was distend without stone (Figures 1-4).
Figure 1-4: Show calcified hydatid cyst of left of liver with distended gall bladder (Albendazol therapy 5 and 3 years ago).
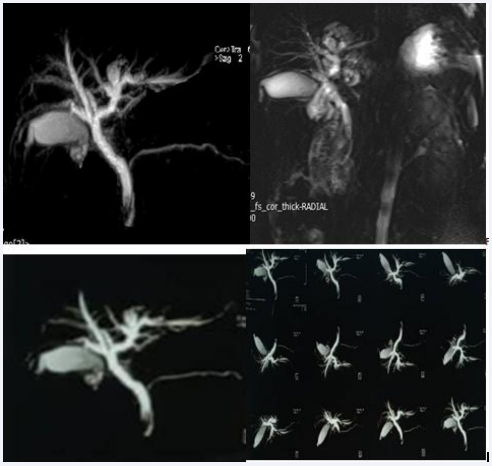
A MRCP scan suggested distal obstruction in the common bile duct and gallbladder was distending without stone (Figures 5-8).
Figure 5-8: MRCP which show dilatation of gallbladder and obstruction with dilatation of CBD.
Endoscopic retrograde cholangiopancreatography (ERCP) was performed and showed a normal papilla without any stone. The cholangiogram showed an irregular defect in the common bile duct. A sphincterotomy was performed and with a balloon the common bile duct was sweep and showed multiple eggs of fasiola hepatica CBD (Figure 9).
Figure 9: Show of fasiola eggs after sphencterctomy.
The eggs were removed using a net basket, and the gross specimen was sent to pathology. Praziquantel (25 mg/kg, three times daily for two days) was prescribed after the procedure at the recommendation of the infectious disease service. The patient was discharged without complications, and he had immediate symptomatic relief after Endoscopic Retrograde Cholangiopancreatogray (ERCP). The specimen was subsequently identified as Fasciola hepatica eggs (Figure 9) and treatment with triclabendazole was started. After two week laparoscopic cholecystectomy was performed .On follow-up examination three weeks later, he remained asymptomatic and test results showed that his liver enzyme levels were normal.
DISCUSSION
Although fascioliasis is endemic zoonotic disease and mainly common in developing countries, in the past decade, because of the increase in worldwide traveling and immigration the number of this cases increased in the worldwide ,now in 61 countries this disease is common [1-3,9]. In the north of Iran Fascioliasis is endemic in Guilan and Mazandran and the incidence is higher than other region [1]. In north of Iran (Guilan and Mazandran) provinces, global prevalence of fascioliasis in sheep and cattle showed 7.3 and 25.4% respectively [1]. Some Studies show that sheep and cattle may be the main reservoir of animal for fascioliasis [3]. Literature revive show that the most case reported article are from this area [3,10]. People usually infected by drinking water in sheep keeping areas [3]. Unboiled water drinking containing viable metacercariae occasionally or by eating poor - cooked liver of sheep can infect the peoples [3,4,9]. When eating infected material, metacercariae pass through duodenum and larvae emerge [1-4]. The larvae penetrate the wall of the proximal portion of small intestine and fall into the peritoneal cavity, then penetrate the gilison capsule of liver, and enter the liver tissue and enter into the biliary ducts [3,9,10]. Typical symptoms fascioliasis can be divided in three phases which including the acute or liver fascioliasis, the chronic or biliary phase, and ectopic or pharyngeal fascioliasis [1,3,4,5,6]. Hepatic phase present with fever, pruritus, abdominal pain, urticaria, headache, weight loss, and eosinophilia. Liver tests (transaminase and bilirubin levels are in normal range or only minimally elevated [1,3,6,9]. Biliary stage is usually asymptomatic, but rarely it can lead to extra hepatic biliary duct obstruction and cholestasis and cholangitis as our case [11,12]. In a report, only 19 cases were to have had CBD obstruction during the 10 years [13]. In another reported five cases with complaints of icterus and pain in the right upper quadrant of the abdomen and in the ERCP showed the Fasiola hepatica in the CBD [14]. In our case after U&S we did MRCP which show obstruction of CBD with distension of gallbladder. Secondary fibrosis and stricture formation can be seen during chronic stage [15]. The diagnosis can be made by stool exam and finding fasiola ova in, duodenal aspiration by endoscopy, or bile specimens [9]. During the first 3-4 months of acute stage of disease, immunologic test is very important tool in the diagnosis of this stat age of disease and ELISA has a sensitivity of 100% and a specificity of 97.8% [1,2,3,4,9]. Our case was in chronic stage with obstruction of CBD. In pats history of our case was hydatid cyst of left lobe of liver with calcification but no history of fasiola hepatica, eosinophilia was 40 %. Our diagnosis with lab date, U&S and MRCP was obstruction of CBD by stone or intra biliary rupture of hydatid csyt, ERCP was performed, after sphentrectomy a lot of fasiola eggs were removed from CBD. Post sphenterctomy all label date and pain of patient gradually decreased, after 24 hour post-operative Triclabendazole was start as a single oral dose of 10 mg/kg. A first-line treatment is with a single dose of triclabendazole, a well-tolerated and that is highly effective against mature and immature flukes [16-19]. Triclabendazole with food should be used to increase its bioavailability [17-20].
CONCLUSION
Because of the immigration of people from a endemic area to another city and worldwide, and especially in endemic area such as Iran and other country, fasiola hepatica , physicians should be aware of this disease and should keep in mind the F- hepatica should be in differential diagnosis of obstructive picture. Also, MRCP is a good tool for diagnosis and ERCP is still important instrument for diagnosis and treatment of the disease and can be used safely with low complications.
REFERENCES
5. Mas-Coma S. Epidemiology of fascioliasis in human endemic areas. J Helminthol. 2005; 79: 207-216.
7. Kim YH, Kang KJ, Kwon JH. Four cases of hepatic fascioliasis mimicking cholangiocarcinoma. Korean J Hepatol. 2005; 11: 169-175.
10. Sezgin O, Altintas E, Disibeyaz S. Hepatobiliary fascioliasis: clinical and radiologic features and endoscopic management. J Clin Gastroenterol. 2004; 38: 285-290.
11. Caprino P, Ferranti Passa G, Quintiliani A. A rare case of obstructive jaundice and cholecystitis in hepatic fascioliasis in Italy. Chir Ital. 2007; 59: 891-894.