An Atypical Form of Neurosyphilis
- 1. Department of Internal Medicine, First Hospital of Jilin University, China
Abstract
A 50-year-old man with weak left limb mobility was admitted in our hospital. Physical examination of the reproductive system showed no abnormalities. No skin rash or ulceration was observed in the penile anus. Head MR enhancement suggested multiple abnormal signals in the right basal ganglia/radiographic crown, Afterwards,benzathine penicillin G was administrated. The above symptoms of the patient were significantly remission, the left extremities no longer paralyse, and could walk in the ward. Three months later, the reexamination of the head MRI enhancement suggested occupying lesion fade away.
KEYWORD
- Neurosyphilis
- Cerebrospinal Fluid
CITATION
Huang Y, Zhao Y (2025) An Atypical Form of Neurosyphilis. Ann Clin Pathol 12(1): 1175.
CASE PRESENTATION
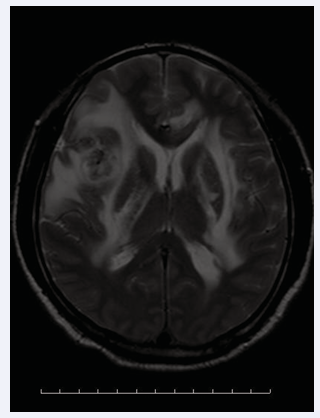
A 50-year-old man with weak left limb mobility was admitted in our hospital. Physical examination: blood pressure 140/80mmHg, clear consciousness, mixed aphasia, bilateral pupil diameter 3mm, sensitive to light reflection, muscle strength of left limb level 2, muscle strength of right limb level 5. The left Babinski sign was positive. Physical examination of the reproductive system showed no abnormalities. No skin rash or ulceration was observed in the penile anus. Head MR enhancement suggested multiple abnormal signals in the right basal ganglia/radiographic crown, considered for malignancy (Figure 1).
Figure 1: Right basal ganglia/radiographic crown occupying lesion (arrow).
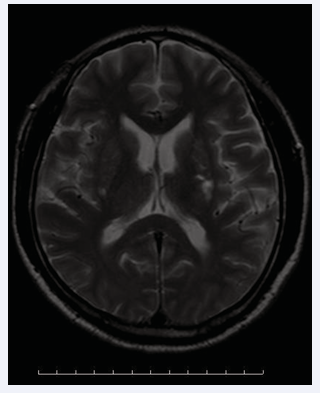
Further craniotomy was planned. However, treponema pallidum antibody (TPPA)25.75S/OO, positive. Serum RPR was 1:8. Furtherlumbar puncture, cerebrospinal fluid pressure of 230mmH2O and cerebrospinal fluid RPR of 1:2. Afterwards,benzathine penicillin G, 2.4 mIU,once a week for three times,was administrated. The above symptoms of the patient were significantly remission, the left extremities no longer paralyse, and could walk in the ward. Three months later, the reexamination of the head MRI enhancement suggested multiple abnormal signals in the right basal node/radiographic crown, which was significantly reduced than before (Figure 2).
Figure 2: Occupying lesion fade away (arrow).
The patient was eventually exempted from surgery and was diagnosed with neurosyphilis.
Therefore, patients have stroke of unknown cause, but if syphilis is highly suspected clinically [1,2], TPPA should be performed even if the reproductive system examination is negative [3]. On the other hand, if neurosyphilis is highly suspected clinically, cerebrospinal fluid examination should be performed and adequate anti-syphilis therapy is mandatory [4,5].
AUTHOR CONTRIBUTIONS
Yuanping Huang writes the manuscript,and Yanfei Zhao reviews the article.
ACKNOWLEDGEMENTS
The authors thank the First Hospital of Jilin University.
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article.
REFERENCES
- Hamill Matthew M, Ghanem Khalil G, Tuddenham Susan. State-of- the-Art Review: Neurosyphilis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2024; 78: e57-e68.
- Ropper Allan H. Neurosyphilis. The New England Journal of Medicine.2019; 381: 1358-1363.
- McAuley John, Hughes Gaenor. Neurosyphilis presenting as parkinsonism. BMJ Case Reports. 2015; 2015: bcr2015210277.
- Jum’ah Ammar, Aboul Nour Hassan, Alkhoujah Mohammad, et al. Neurosyphilis in disguise. Neuroradiology. 2021; 64: 433-441.
- Liu Hui, Zhao Zong-Bo, You Nian-Xing. Diversity in clinical manifestations and imaging features of neurosyphilis: obstacles to the diagnosis and treatment (report of three cases). The International Journal of Neuroscience. 2017; 128: 785-790.