Histopathological Findings after Transanal Proximal Rectosigmoid Resection for Severe Chronic Idiopathic Constipation in Children with Megarectosigmoid
- 1. Department of Surgery, West Virginia University, USA
- 2. Department of Pediatric General and Thoracic Surgery, UPMC Children’s Hospital of Pittsburgh, USA
- 3. Pathology and Laboratory Medicine, Miller School, University of Miami, USA
- 4. International Center for Colorectal and Urogenital Care, Children’s Hospital Colorado, USA
Abstract
Purpose: To describe the histopathological findings in the megarectosigmoid of pediatric patients with severe chronic idiopathic constipation (CIC) who underwent a transanal proximal rectosigmoid resection. Methods: This study included pediatric patients diagnosed with severe CIC with megarectosigmoid, who underwent transanal proximal rectosigmoidectomy at the Colorectal Center for Children at UPMC Children’s Hospital of Pittsburgh between July 2017 and May 2018. A retrospective case review was conducted. Histopathological analysis of the resected specimens was performed circumferentially at both the proximal and distal margins. Longitudinal sections throughout the entire specimen length were also assessed. Muscle thickness and nerve fiber size were compared with age-matched controls. Statistical analyses were carried out using SPSS version 21.0. Results: A total of twelve patients met the inclusion criteria. The median age at the time of surgery was 8.6 years, with a predominance of male patients. The median duration of constipation was 5.5 years. Histopathological examination revealed significant hypertrophy of both the inner and outer muscular layers of the muscularis propria, as well as thickened nerve fibers and an increased width of the lamina propria when compared to controls. The increased thickness of the lamina propria was primarily attributed to fibrosis. A significant difference (p<0.05) in the thickness of the outer muscularis propria, nerve fiber size, and lamina propria was observed when comparing the distal (rectum) with the proximal margin (sigmoid) of the specimen. Fibrosis was universally present in all cases, predominantly within the lamina propria, and was more pronounced in the distal than the proximal segment. No morphometric analysis was performed for this assessment. Conclusion: Histopathological findings in pediatric patients with severe CIC and megarectosigmoid demonstrated marked muscular hypertrophy, thickened nerve fibers, and fibrosis within the lamina propria, with the most pronounced alterations observed in the resected rectal segment. These findings suggest a more advanced disease process within the rectum. This report is the first to document fibrosis in this patient population, raising concerns regarding potential irreversible changes that may only be amenable to surgical intervention.
Keywords
• Chronic idiopathic constipation
• Megarectum
• Megarectosigmoid
• Muscular hypertrophy
• Transanal proximal rectosigmoid resection
• Children
Citation
Wehrli LA, Scholz S, Salgado CM, De La Torre L (2025) Histopathological Findings after Transanal Proximal Rectosigmoid Resection for Severe Chronic Idiopathic Constipation in Children with Megarectosigmoid. Ann Clin Pathol 12(1): 1179.
INTRODUCTION
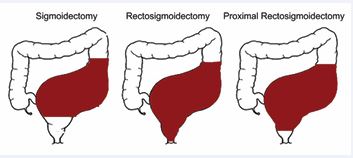
Chronic idiopathic constipation (CIC) is a prevalent condition in the pediatric population, often managed with various laxative treatments [1,2]. In cases of severe CIC, significant anatomical changes such as megarectosigmoid are commonly observed. These patients frequently require high-dose stimulant laxatives to achieve complete fecal evacuation of the megarectosigmoid. However, some patients fail to respond to laxative therapy due to inadequate efficacy or adverse side effects, necessitating surgical intervention. Various surgical approaches have been proposed for the management of severe constipation with megarectosigmoid [2–6], but the outcomes following these interventions are often variable, and complete resolution of fecal retention is not always achieved. Additionally, certain surgical procedures carry the risk of leaving the patient fecally incontinent [6,7]. Up until 2017,sigmoidectomy was the most common surgical approach for patients with CIC complicated by megarectosigmoid (Figure 1).
Figure 1 Schematic diagram of the extent of surgical resection in patients with megarectum and severe chronic idiopathic constipation, with red being the resection areas.
These patients often continued to experience recurrent fecal impaction within the residual rectal pouch. In 2019, our group published the clinical results a novel technique, the transanal proximal rectosigmoidectomy, which involves leaving a small rectal pouch of 5 to 7 cm in length, sufficient to prevent recurrent fecal impaction while preserving fecal continence due to its reservoir function [7]. Preliminary results indicated favorable postoperative outcomes, with follow-up periods ranging from 6 to 13 months showing restored fecal control, daily bowel movements, a significant reduction in laxative use, and the absence of fecal impaction and abdominal pain, with preserved fecal continence. The current study aims to characterize the histopathological findings of specimens obtained from this patient population, who underwent a transanal proximal rectosigmoidectomy for severe chronic idiopathic constipation with associated megarectosigmoid.
METHODS
Patient population and age-matched control group
Pediatric patients, younger than 19 years, with severe CIC associated with megarectosigmoid, who underwent transanal proximal rectosigmoidectomy at the Colorectal Center for Children at UPMC Children’s Hospital of Pittsburgh between July 2017 and May 2018, were included in the study. A retrospective case review was performed, collecting data on demographics, medical and surgical treatment history, and age at surgery. Clinical outcomes for this cohort were previously published [4]. A matched control group was selected by reviewing the pathology archives for autopsy and surgical specimens from age- and gender-matched individuals. Cases with a clinical history of constipation and/or confirmed or suspected forms of gastrointestinal or neuromuscular pathologies were excluded.This study was approved by the Institutional Review Board (STUDY22010091).
Histopathological Workup
A standard histopathological protocol was followed for the resected rectosigmoid specimens, which included circumferential full-thickness sections taken from both, the proximal (sigmoid) and distal (rectum) margins, as well as longitudinal sections spanning the entire length of the specimen. The specimens were fixed in 10% formalin, paraffin-embedded, and cut into 4 micrometer sections, which were subsequently stained with Hematoxylin and Eosin (H&E). In addition to Masson’s trichrome staining for evaluation of fibrosis, calretinin immunostaining was performed to assess the distribution and density of the myenteric and submucosal plexuses, and GLUT-1 immunostaining was utilized to facilitate measurement of nerve fiber thickness. Immunohistochemistry was performed on the Ventana® Benchmark XT (Ventana Medical Systems, Tucson, AZ) following the manufacturer’s instructions, using the primary antibody rabbit anti calretinin (Ventana prediluted kit #790-4467; Ventana Medical Systems). All histological slides and molecular results were reviewed.
Image capture, morphometric, and statistical analysis
Whole-slide images were captured by scanning at ×40 magnification using an Aperio Scanscope (Sausalito, CA, USA). Morphometric analysis was performed with Aperio ImageScope software, with measurements of the lamina propria and muscular layers taken from well-oriented sections. Three measurements were recorded for each available slide. The thickness of the lamina and muscularis propria and the diameter of nerve fibers were compared to age-matched controls. The location and extent of fibrosis within the specimens were documented. Fibrosis was not quantitatively compared to controls since there is a lack of standardized methods for assessing fibrosis in the colonic wall. Statistical analysis was conducted using SPSS version 21.0 (SPSS, Chicago, IL, USA). Results were presented as mean (SD) or total number and percentage. The Student’s t-test was used to compare continuous variables, and the chi-square test was applied to categorical variables. Statistical significance was set at p<0.05.
RESULTS
Twelve patients met the inclusion criteria (Table 1). The majority (66.7%) were male, and the patients’ ages ranged from 1.7 to 19 years, with a mean age of 8.5 years at the time of surgery. The median duration of constipation was 5.5 years. Half of the patients had a rectal biopsy preoperatively, none had Hirschsprung disease. All patients underwent transanal proximal rectosigmoidectomy, with or without appendicostomy creation and Botox injection into the anal sphincter at the time of surgery. Resected length ranged from 5cm to 18cm, with a mean of 10.7cm. The maximal diameter of the rectum varied from 3cm to 19.4cm, with a mean of 5.4cm. Fibrosis or fibrotic thickening was seen in eight patients, and in the remaining four patients, thickened muscularis propria was found.
Table 1: Patient population and specifics of resected specimen.
|
# |
Gender [f/m] |
Age at time of surgery [years] |
Length [cm] |
Diameter [cm] |
|
1 |
f |
12 |
5 |
3 |
|
2 |
f |
11 |
11 |
4 |
|
3 |
f |
8 |
10.5 |
3.5 |
|
4 |
m |
3 |
9.2 |
3.4 |
|
5 |
m |
18 |
5 |
8.6 |
|
6 |
m |
6 |
6 |
3.5 |
|
7 |
m |
19 |
18 |
19.4 |
|
8 |
m |
5 |
11.5 |
2.6 |
|
9 |
m |
10 |
9.7 |
5.3 |
|
10 |
f |
1.7 |
12.5 |
3.2 |
|
11 |
m |
4 |
18 |
4.3 |
|
12 |
m |
5 |
11.5 |
4 |
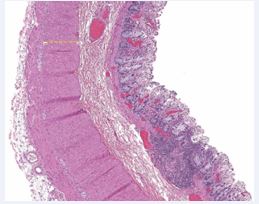
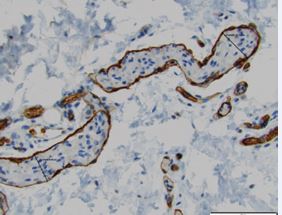
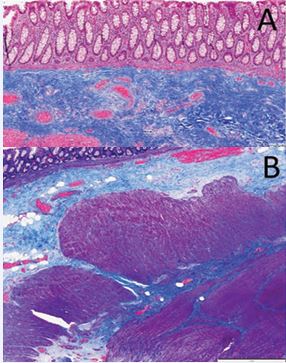
Histopathological examination revealed significant hypertrophy of both the inner and outer muscular layers of the muscularis propria, thickened nerve fibers, and increased lamina propria width in all patients compared to the control group (Table 2, Figures 2A/B, Figure 3, Figure 4, Figure 5A/B and Figure 6A/B). Notably, the increased thickness of the lamina propria was primarily attributed to fibrosis (Figures 4A and 4B). The distal portion (rectum) of the specimens exhibited more prominent fibrosis compared to the proximal portion (sigmoid), although no morphometric analysis was performed for this aspect.
Table 2: Patients with chronic idiopathic constipation who underwent transanal rectosigmoid resection compared to age and gender-matched controls. The proximal and distal segment of the specimen was compared to age and gender matched controls.
|
|
Case Group |
Control Group |
p-value |
|
Age [years] |
8.6 ± 5.6 |
8.8 ± 5.8 |
0.9 |
|
PROXIMAL MARGIN [µm] |
|||
|
Inner muscularis propria |
1071.7 ±469.7 |
481.8 ± 218 |
<0.001 |
|
Outer muscularis propria |
861.5±489.1 |
375.6±180.9 |
0.02 |
|
Nerve thickness |
34.7±11.9 |
26.3±4.6 |
0.03 |
|
Lamina propria thickness |
1089.8±386.3 |
447.9±192 |
<0.001 |
|
DISTAL MARGIN [µm] |
|||
|
Inner muscularis propria |
1205.4±463.1 |
481.8 ± 218 |
<0.001 |
|
Outer muscularis propria |
1420.6±739.6 |
375.6±180.9 |
<0.001 |
|
Nerve thickness |
45.2±13.6 |
26.3±4.6 |
<0.001 |
|
Lamina propria thickness |
1407.4±540 |
447.9±192 |
<0.001 |
Statistical comparison between the distal and proximal margins of the specimens revealed significant differences in the thickness of the outer (longitudinal) muscularis propria, nerve fiber size, and lamina propria (p<0.05) (Table 3). No significant difference was observed in the thickness of the inner muscularis propria between the proximal and distal measurements (p=0.432).
Table 3: Patients with chronic idiopathic constipation who underwent transanal rectosigmoid resection, with comparison of the proximal and distal segment measurements within the patient population.
|
|
Distal Resection Margin [µm] |
Proximal Resection Margin [µm] |
p-value |
|
Inner muscle |
1205.36±463.1 |
1071.73 ±469.7 |
0.4 |
|
Outer muscle |
1420.55±739.6 |
861.45±489.1 |
0.03 |
|
Nerve thickness |
45.17±13.6 |
34.67±11.9 |
0.049 |
|
Lamina propria thickness |
1407.40±540 |
1089.80±386.3 |
0.04 |
Figure 2 A/B: Hematoxylin & Eosin staining: Muscular hypertrophy, demonstrated with the measurements of the inner versus outer muscularis propria as shown in a specimen of a patient with severe chronic idiopathic constipation who underwent transanal rectosigmoid resection.
Figure 3 Hematoxylin and eosin staining of control group tissue. The section demonstrates normal-appearing muscular thickness of both the inner and outer layers of the muscularis propria, with preserved overall histological architecture.
Figure 4 GLUT-1 immunohistochemical staining highlighting intrinsic nerve fibers and ganglion cells, demonstrating hypertrophic nerve fibers in a patient who underwent transanal rectosigmoid resection for severe chronic idiopathic constipation.
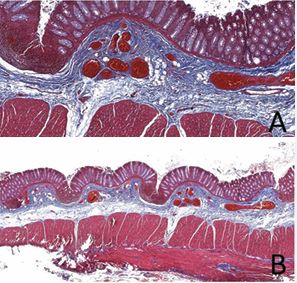
Figure 5 A/B: Masson’s trichrome staining of rectal tissue from a patient with severe chronic idiopathic constipation following transanal rectosigmoidectomy. The section demonstrates marked fibrosis within the lamina propria, characterized by an increased abundance of blue-stained collagen fibers. Cytoplasm appears pink and muscle fibers stain red, providing contrast that highlights the extent of collagen deposition and disruption of normal tissue architecture.
Figure 6 A/B: Masson’s trichrome staining of control group tissue. Collagen fibers are stained blue, cytoplasm appears pink, and muscle fibers are stained red, demonstrating normal tissue architecture without evidence of fibrosis or structural abnormalities.
|
|
Distal Resection Margin [µm] |
Proximal Resection Margin [µm] |
p-value |
|
Inner muscle |
1205.36±463.1 |
1071.73 ±469.7 |
0.4 |
|
Outer muscle |
1420.55±739.6 |
861.45±489.1 |
0.03 |
|
Nerve thickness |
45.17±13.6 |
34.67±11.9 |
0.049 |
|
Lamina propria thickness |
1407.40±540 |
1089.80±386.3 |
0.04 |
Table 3: Patients with chronic idiopathic constipation who underwent transanal rectosigmoid resection, with comparison of the proximal and distal segment measurements within the patient population.
DISCUSSION
Chronic constipation in pediatric patients is common, with an incidence rate as high as 30% [2,7–12]. Previous studies have discussed histopathological findings in gastrointestinal motility disorders associated with constipation [8,9]. Numerous surgical options have been proposed for the management of severe idiopathic constipation with megarectosigmoid [2-6,11,12], although none have reported the histopathological characteristics of resected specimens. To this date, none have compared the clinical picture with the histopathologic findings in this patient population due to a lack of tissue analyses and comparisons with a reference population. Several factors contribute to coordinated peristalsis within the colon. The proper interaction of nerve cells and nerve fibers with the muscularis propria leads to propulsive peristalsis. Disruption of this coordination can lead to gastrointestinal dysmotility resulting in constipation. This study is the first to report histopathological findings in pediatric patients with megarectosigmoid and severe idiopathic chronic constipation, revealing a progression of pathological changes, including muscular hypertrophy, nerve fiber hypertrophy, and lamina propria thickening. The most significant changes were observed in the distal rectum, suggesting that the origin of these alterations may lie within the rectum itself. The thickening of the lamina propria was mainly due to increased connective tissue, raising concerns about structural damage within the distal colon. Further studies are needed to assess the extent and reversibility of these pathological changes.
CONCLUSION
Histopathological findings in pediatric patients with severe chronic idiopathic constipation and megarectosigmoid revealed significant muscular hypertrophy, nerve fiber thickening, and fibrosis of the lamina propria, with the most pronounced changes observed in the rectal segment. These findings suggest that the rectum may be the primary site of pathological changes. This report is the first to document fibrosis in this patient population, raising concerns about the potential irreversibility of these changes, which may only be addressed through surgical intervention. Further studies are necessary to evaluate the full extent of the disease process in chronic constipation among children.
AUTHORS AND ROLES
LAW: Conceptualization, drafting the work, reviewing the manuscript, final approval of the version to be published. SS: critically reviewed the manuscript, final approval of the version to be published. CMS: Conceptualization and Data analysis, critically reviewed the manuscript, final approval of the version to be published. LDLT: Conceptualization, Interpretation of data for the work, reviewed the manuscript, final approval of the version to be published.
REFERENCES
- Bischoff A, Brisighelli G, Dickie B, Frischer J, Levitt MA, Peña A. Idiopathic constipation: A challenging but manageable problem. J Pediatr Surg. 2018; 53: 1742-1747.
- Bokova E, Svetanoff WJ, Rosen JM, Levitt MA, Rentea RM. Review: State of the Art Bowel Management for Pediatric Colorectal Problems: Functional Constipation. Children. 2023; 10, 1078.
- Wood RJ, Yacob D, Levitt MA. Surgical options for the management of severe functional constipation in children. Curr Opin Pediatr. 2016; 28: 370-379.
- De la Torre L, Cogley K, Cabrera-Hernández MA, Frias-Mantilla JE, Wehrli LA. Transanal proximal rectosigmoidectomy. A new operation for severe chronic idiopathic constipation associated with megarectosigmoid. J Pediatr Surg. 2019; 54: 2311-2317.
- De La Torre L, Cogley K, Calisto J, Nace G, Correa C. Primary sigmoidectomy and appendicostomy for chronic idiopathic constipation. Pediatr Surg Int. 2016; 32: 767-772.
- Levitt MA, Martin CA, Falcone RA, Peña A. Transanal rectosigmoid resection for severe intractable idiopathic constipation. J Pediatr Surg. 2009; 44: 1285-1291.
- De la Torre L, Zornoza-Moreno M, Cogley K, Calisto JL, Wehrli LA, Ruiz-Montañez A, et al. Transanal endorectal approach for the treatment of idiopathic rectal prolapse in children: Experience with the modified Delorme’s procedure. J Pediatr Surg. 2019; 54: 857–861.
- Feichter S, Meier-Ruge WA, Bruder E. The histopathology of gastrointestinal motility disorders in children. Semin Pediatr Surg. 2009; 18: 206-211.
- Meier-Ruge WA, Bruder E. Pathology of chronic constipation inpediatric and adult coloproctology. Pathobiology. 2005; 72: 1-106.
- Koppen IJ, Di Lorenzo C, Saps M, Dinning PG, Yacob D, Levitt MA, et al. Childhood constipation: Finally something is moving! Expert Rev Gastroenterol Hepatol. 2016; 10: 141-155.
- Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: A systematic review. Best Pract Res Clin Gastroenterol. 2011; 25: 3-18.
- Vilanova-Sanchez A, Levitt MA. Surgical Interventions for FunctionalConstipation: An Update. Eur J Pediatr Surg. 2020; 30: 413-419.