Treatment of Invasive Fungal Disease During Therapy for Acute Lymphoblastic Leukemia: A Case Report
- 1. Pediatric Hematology Oncology, King Fahad Armed Forces Hospital, Saudi Arabia
- 2. Department of Pediatrics, Umm Al-Qura University, Saudi Arabia
- 3. Department of Pediatrics, King Fahad Armed Forces Hospital, Saudi Arabia
- 4. Medicine and Surgery, Umm Al-Qura University, Saudi Arabia
- 5. Department of Pathology, Cairo University, Egypt
ABSTRACT
Background: Invasive fungal infections (IFDs) are one of the leading causes of death in acute leukaemia patients (AL). Because of the possibility of fungal relapse, patients who survive invasive fungal illnesses may have difficulty completing the whole chemotherapy plan.
Objectives: Review Invasive Fungal Diseases in children with Acute Leukemia and present tow cases of Pre-B Acute Lymphoblastic Leukemia complicated with Invasive fungal infection with Aspergillosis.
Methods: Two 9 years old female patients diagnosed with Pre-B Acute Lymphoblastic Leukemia that was on the pre-B ALL Protocol: CALL08, Arm-C (High Risk Arm) and the supportive therapy. They were both on Arm C of the CALL08 Protocol (high Risk based on COG232). Then, the patients experienced severe febrile neutropenia. Patient A was during consolidation and patient B during Interim Maintenance I. Both experienced prolonged febrile neutropenia. As Febrile neutropenia continues > 5 days, fungal work was done including CT Sinuses, Chest, and abdomen as well as serum galactomannan, and (1-3)-β-d-glucan (BG). Caspofungin was started. Fungal work up results showed lung and liver nodules in one patient and lungs, liver and spleen in the other. There were about 4 weeks of severe fevers and neutropenia despite broad spectrum antibiotics used. A decision was taken to interrupt chemotherapy for both patients. Voriconazole was added to Caspofungin and continued on Meropenem. Biopsies confirmed the diagnosis to be severe fungal infection with Invasive Aspergillosis. After that, high fevers and neutropenia slowly recovered and repeated CT Abdomen showed good improvement in the lesions number and size. After 6-8 weeks of interruption, chemotherapy was resumed.
Results: Implementation of combination antifungal therapy with Voriconazole & Caspofungin for 6 weeks then single antifungal therapy (Voriconazole orally) for another 6 weeks, both patients recovered, became clinically stable and afebrile. Chemotherapy was on hold till they become better.
Conclusion: Primary and secondary antifungal prophylaxis are recommended for ALL patients. Chemotherapy discontinuation is decided on an individual basis according to the severity of the fungal infection and disease status.
KEYWORDS
- Invasive
- Fungal
- Infection
- ALL (Acute Lymphoblastic Leukemia)
- Case Report
CITATION
Alharbi I, Nassif A, Hennawi YB, Farhan M (2024) Treatment of Invasive Fungal Disease During Therapy for Acute Lymphoblastic Leukemia: A Case Report. Ann Clin Pathol 11(1): 1171.
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is considered the most common malignancy in children accounting for 25% of all pediatric cancers [1]. The most prevalent complication of Pre-B Acute Lymphoblastic Leukemia is infection. Furthermore, there are also gastrointestinal, neurologic, metabolic/endocrine, drug-related hypersensitivity, and severe psychological issues all result either from the disease itself or from chemotherapy complications [2]. Chemotherapy can make these children extremely immunocompromised and vvulnerable to infections.
In such immunocompromised patients, opportunistic invasive fungal infections are the leading cause of morbidity and mortality. Moreover, the presence of moulds or yeasts in deep tissues can persist and become very hard to get rid of even with optimal antifungal therapy. In addition, it is not very straightforward sometimes to diagnose these infections. We need to do biopsy or a culture obtained by a sterile procedure to prove the existence of invasive fungal disease (IFD) [3]. The most prevalent fungal infection in humans is aspergillosis, which accounts for more than 85% of invasive fungal disease [4].
The opportunistic infection known as invasive aspergillosis (IA) is caused by Aspergillus spp. Aspergillus is a saprophytic filamentous fungus that is frequently isolated in the environment [5]. Because of difficulties in performing the invasive procedure to diagnose it, a lot of effort has gone into creating a non-invasive test for the diagnosis of Invasive Aspergillosis (IA), especially techniques to find galactomannan [6]. Aspergillus releases galactomannan, a polysaccharide cell-wall component, as it grows [6,7]. Consequently, for monitoring invasive Aspergillosis, a double-sandwich enzyme-linked immunosorbent galactomannan assay has been licenced [7], Additionally, (1→3)-β-D-glucan (BDG) is an appropriate material to screen for IFDs because it is a part of the fungal cell wall and is not present in bacteria or human cells. The G-test, which measures BDG in serum using a coagulation factor derived from horseshoe crab blood, was created initially in Japan [8].
Haematological malignancies, particularly acute myeloid leukaemia (AML), acute lymphoblastic leukaemia (ALL), and allogeneic HSCT recipients, are associated with IA in patients [3,4]. Extreme neutropenia brought on by chemotherapy (especially lasting >7 days; ANC 500 cell/mm3) continues to be the single biggest risk factor for IA [9].
Fever unresponsive to broad-spectrum antibiotics in neutropenic patients is a common early symptom that should warrant additional investigation. Coughing or chest pain with or without haemoptysis, both symptoms of pulmonary infarction caused by fungal-induced vascular blockage, have been recorded on rare occasions. The critically ill ICU patient with IA, on the other hand, is largely mechanically ventilated and may have decreasing lung function and refractory fever. Progression to disseminated disease is a common consequence that goes unnoticed, especially in individuals who have a severe or advanced underlying condition. Cerebral dispersion can reveal itself late in the form of seizures or other focal neurological symptoms. Although, it’s uncommon to have a primary extrapulmonary organ at presentation [9].
CASE PRESENTATION
Case 1
A 9 years old girl with 2 weeks history of fevers, pallor, and pancytopenia. CBC showed 2-cell line pancytopenia and CBC showed peripheral blood blasts. On Examination, the patient was afebrile, Head and Neck examination were unremarkable. CVS examination showed normal S1 & S2 with no murmur. The abdomen was soft, non-tender with bowel sounds. The liver and spleen was 2 cm below costal margin (BCM). The CNS exam was normal, and the patient’s skin was pale with no ecchymosis or petechiae. Bone marrow aspiration showed 95 % Blasts and the Flow Cytometry showed Pre-B ALL. Results were consistent with Pre-B ALL and the RUNX1 was positive. The WBC level was 6.8 on admission and become 0.7 at day 8 of induction. Hemoglobin level was 8.6, Hct volume was 24.8, platelets level was 86 and total Bilirubin was 2. LDH was 702 and went up to 4000 with the start of induction. The recommended plan for management was the pre-B ALL Protocol: CALL08, Arm-C (High Risk Arm) and the supportive therapy.
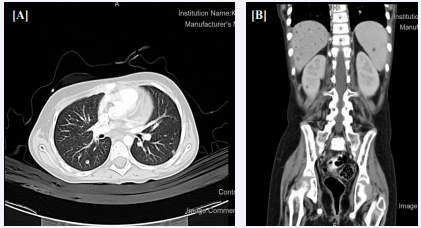
One and half year later the patient experienced severe febrile neutropenia. Initial fungal work up showed questionable lung nodules which could be fungal. Liposomal Amphotericin B was started and Caspofungin was discontinued. After about 4 weeks of severe fevers and neutropenia, a decision was made to give her G-CSF at 5 micgram/Kg/Day S/C. After 3 days her neutrophils count increased to >3000. Interim Maintenance I of Arm-C of the CALL08 Protocol started and she Vincristine IV, IT Methotrexate, IV Methotrexate and L-Asparginas was given. Two months later, the patient had severe neutropenia again with fevers and chills. CT chest, Abdomen and Sinuses showed numerous nodules of severe fungal infection with Invasive Aspergillosis in the liver, spleen and kidneys [Figure 1]. Patient also developed severe hyperbilirubinemia, but transaminases were normal. Total bilirubin increased to 464 and conjugated bilirubin was 181 & GGT to 1097.
Figure 1 (A) Chest CT scan chest showing tiny pulmonary nodules are noticed one in the left lower lung. (B) Abdominal CT with contrast of showing numerous nodules in the liver, spleen and kidneys.
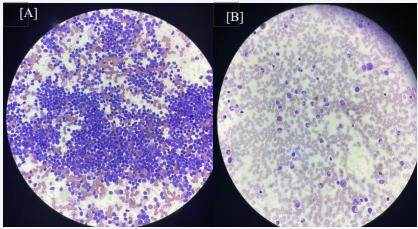
The patient started Voriconazole and Caspofungin continue combination therapy. Biopsy showed hyphae with septate (possible Aspergillus) [Figure 2]. After 9 days, the dose of Voriconazole was adjusted to 9 mg/kg/dose q 12 hours and the patient continued to improve and NG Feeding was started. After 6 weeks the patient become stable and afebrile. Hyperbilirubinemia likely secondary to chemotherapy and anti-fungal experienced before and during consolidation and resolved. Then the patient is a cases of HR ALL- in remission, on the day 16 of IM-1. Chemotherapy was on hold till she becomes better.
Figure 2 (A) Ultrasound Guided Biopsy of liver nodules showing hyphae with septate (possible Aspergillus). (B) Biopsy of liver nodules after fungal treatment..
Case 2
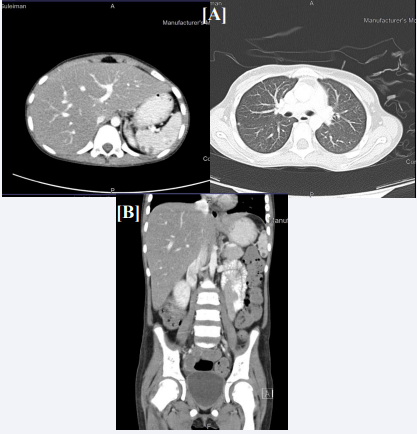
A 9 years old girl with newly diagnosed Acute Lymphoblastic Leukemia (B-ALL). She had pallor, petechiae and ecchymosis as presenting complaints. On examination, there was pallor, scattered petechiae, mild hepatomegaly, palpable spleen tip without significant lymphadenopathy. Investigations were done and the WBC count was 12.6, the Hb was 6.5 and the platelets count was 94. Bone Marrow examination showed an overall immunophenotype results that are most consistent with B lymphoblastic leukemic cells in common BALL. CT chest showed new tiny pulmonary nodules are noticed one in the left lower lung anterior measures about 3 mm the other tiny nodule in the right mid lung lobe anterior subpleural location measures about 3.5 mm while abdominal CT showed Both kidneys show bilateral scattered focal hypodensities/esons the largest seen in the left kidney measuring about 6.1 X 3.9 mm Partial opacification of the proximal small bowel lope with oral contrast with evidence of focal soft tissue density seen in the proximal jejunum could be related to intussusception however other underlying pathology cannot be ruled out, Evidence of mild intra-abdominal free fluid mainly in pelvis. The large bowel it loaded with fecal matter [Figure 3]. Follow up with cytogenetic study for further classification and diagnosis was advised. The diagnosis was a case of acute Lymphoblastic Leukemia for standard risk chemotherapy protocol. It was recommended to continue to follow up with pediatric oncology and bactrim prophylaxis together with Chlorehexidine Mouth Wash was advised.
Figure 3 (A) Chest CT scan chest showing tiny pulmonary nodules are noticed one in the left lower lung. (B) Abdominal CT with contrast showing numerous nodules in the liver, spleen and kidneys.
She was started on voriconazole 9 mg/kg as induction dose for one day and to continue 8 mg/kg given twice per day as maintenance. Reassessment showed mixed response with regressions and reappearance of some nodule. Therefore, the dose was increased to 14 mg/kg given twice per day. However, she experienced elevated liver enzymes which could attributed to the use of medications. Liposomal Amphotericin B was added IV 5mg/kg given once per day for one month, at that time she had resistant electrolytes imbalance in form of low potassium. This is hypokalemia most likely due to use of medication. As result she was shifted to oral Posaconazole 100 mg given twice per day orally, she continued to have hypokalemia, Infectious Disease and Nephrology teams consultations were done and they recommended to reduce the dose of Posaconazole to 100 mg given once per day orally which showed marked improvement of hypokalemia and fungal assessment showed static nodules. Plan was to continue chemotherapy and antifungal until the end of maintenance chemotherapy. Now she is on chemotherapy (Arm-C, delayed intensification #1 week 29), Posaconazole 100 mg given once per day orally and Bactrim 50 mg given twice per day orally two days weekly.
DISCUSSION
In these two cases, 9 years old patients were diagnosed with Pre-B Acute Lymphoblastic Leukemia (ALL) and both cases were complicated with Invasive fungal infection (Aspergillosis).
The risk of invasive fungal diseases (IFDs) is highly unpredictable due to the variability of severity of disease in children with (ALL). It seems to be the result of interactions between 3 factors; immunosuppression, organ failure and exposure to opportunistic fungi [10]. Immunosuppression is caused by corticosteroid and chemotherapy causing, cell- mediated, humoral, and phagocytic dysfunction that will result in predisposition to IFDs [11].
It was discovered that exposure to opportunistic fungi also increases the incidence of IFDs. It has been well known that Aspergillus species colonise the airways of many individuals [12]. In adult patients with newly diagnosed AML, Italian researchers found a substantial link between pre-hospitalization exposure to fungus sources and the development of IFDs within 30 days after the first session of chemotherapy [13]. Inhalation of fungal spores is critical in the development of IFDs [13]. Invasive fungal diseases (IFDs) are a leading cause of mortality and morbidly in pediatric patients with acute leukemia. It affects 5-15 % of pediatric patients with acute leukemia [14]. The majority of these cases are in Acute Lymphoblastic Leukemia. Invasive aspergillus patients are reported to have a death rate of 28-42 % three months following diagnosis [15].
Our cases showed numerous nodules of severe fungal infection with Invasive Aspergillosis in the liver as well as in the spleen and kidneys on repeated Fungal work up (CT Abdomen, Chest, and Sinuses). According to a retrospective review, nodules were the most common diagnostic radiologic finding in 48 (34.6%) out of 139 paediatric invasive aspergillosis cases [16]. Both patients initially started on Liposomal Amphotericin.
Then continued on a combination of Caspofungin and Voriconazole therapy. Because of its excellent efficacy, Voriconazole belongs to a class of antifungal called triazoles. It acts by slowing Fungal Growth. It is used to treat infections with many fungal infections including aspergillosis, candidiasis, coccidioidomycosis, histoplasmosis, penicilliosis, and infections by Scedosporium or Fusarium. It is also used as a prophylaxis to prevent IFDs. International guidelines recommend administration of Voriconazole as pyrophytic agent against IFDs (17; 19). In addition, Voriconazole is the drug of choice for aspergillosis [17,18]. About 86% of patients with invasive fungal illness who received subsequent antifungal prophylaxis would have had reduced fungal reactivation risk [19]. Antifungal prophylaxis was also advised for AML patients receiving induction chemotherapy [20]. Caspofungin is a drug that belongs to Echinocandins class. It has a broad-spectrum fungicidal activity against many fungal infections including Candida and fungistatic activity against Aspergillus species (22). It is used specifically used to treat invasive Candidiasis, like esophageal Candidiasis, and invasive Aspergillosis. It may be explored for prophylaxis against invasive fungal illness in children, adolescents, and young adults with acute leukaemia, according to Fisher et al., [21]. In a randomised trial of adolescents and adults with AML, the risk of IFDs was reduced with caspofungin prophylaxis and that was equivalent to Posaconazole prophylaxis [22]. Other trials found that voriconazole, Amphotericin B, Caspofungin, or Posaconazole, alone or in combination, were effective in treating IFDs in ALL individuals [23,24].
The chemotherapy treatment protocols of both of our cases were interrupted for more than 4 weeks. To avoid risk of relapse, patients needed to have some form of mild chemotherapy in order to keep them both in a continuous remission. Based on most recent evidence, they both received Intravenous Vincristine every 2-3 weeks as well as Intrathecal Methotrexate every 3-4 weeks.
Therefore, chemotherapy schedule in both of our cases was interrupted. According to a recent study, patients with invasive fungal disease, despite initially surviving the infections, have considerable risk of persistent infection unless alterations are carried out in their chemotherapeutic schedule. Patients who are receiving chemotherapy and had IFD wull be at risk of serious life-threatening consequences unless chemotheraoy is interrupted and Neutrophils count is allowed to normalize for a long period of time [19]. There is a high probability of persistent/ recurrent fungal infections which is believed to be around 30% in patients who survive first invasive fungal disease if not treated well. In addition, these patients may have difficulty completing the whole chemotherapy protocol [25]. Those patients frequently have delayed and/or reduction of their chemotherapy doses. Reduction of chemotherapy doses continue until IFDs is controlled [25]. According to the Even et al., study which showed that despite an initial satisfactory outcome, the appearance of invasive fungal illness during acute leukaemia treatment has led to a change in the chemotherapy protocol, either delaying the following cycle, changing the drug, or reducing the dosage [19]. The principle behind reducing the chemotherapy intensity is to allow full and prolonged neutrophils count recovery.
Our cases experienced about 4 weeks of severe fevers and neutropenia. We had to interrupt their chemotherapy for a prolonged period of time. Regarding which acute leukemia is more likely to be associated with IFD, researchers from a single Taiwanese hospital found in 2011 that invasive fungal sinusitis (IFS) was more prevalent in AML patients with persistent neutropenia throughout a 15-year period than with ALL [26]. When considering ig duration of neutropenia is associated with the risk of IDF, Lien et al., found a ldirect ink between the length of neutropenia (more than 30 days) and significant risk of IFD [17]. When considering if there are other factors that can contribute to the risk of IFD in addition to prolonged neutropenia, a retrospective investigation by Nicolato et al. found that prolonged neutropenia, relapse of underlying illnesses, extended hospitalisation before the first fever, and allogeneic HSCT were all risk factors for IFI in ALL. These risk factors have also been seen in our case [27]. The generation of normal neutrophils decreases as leukaemia cells proliferate in the bone marrow [17]. According to another recent study, the majority of our patients (88%) were severely neutropenic at the time of diagnosis of IFD and the overall median duration of neutropenia was longer than 10 days [28].
Previous research has shown that fast and effective antifungal medication combined with sensible treatment modalities can reduce the risk of death in children with ALL and IFD. If chemotherapy is held and interrupted for neutrophils count full recovery for a sufficient period of time that allow control of IFD, then chemotherapy can be restarted after a few weeks of interruption [28]. The perfect exact timing to resume full chemotherapy doses and schedules in these patients is unknown. Although we believe the exact time is most likely when fungal lesions are resolved and disappeared on further imaging evaluation [23].
What is the optimal duration of time of chemotherapy interruption? In our cases, interruption ranged from 4 to 12 weeks. Previous data have produced similar results. According to Tüfekçi et al., 2015, the median time to stop chemotherapy was 27 days, and chemotherapy was safely restarted in 50% of the patients before 4 weeks duration. IFD was not reactivated in any of the those patients [28]. In a retrospective assessment of hematological malignancies, Nosari et al. found 61 adult instances with IFD and discovered a median period of 27 days for chemotherapy termination (range: 17-45 days) was appropriate [28].
CONCLUSION
Primary prophylaxis, empirical or preemptive antifungal medication, and secondary prophylaxis are all options for treating patients. Chemotherapy timing is usually decided on an individual basis, depending on the severity of the fungal infection and the status of the main disease.
REFERENCES
- Inaba H, Greaves M, Mullighan CG. Acute lymphoblastic leukaemia.Lancet. 2013; 381:1943-1955.
- Öztürk AP, Koç B, Zülfikar B. Acute Complications and Survival Analysis of Childhood Acute Lymphoblastic Leukemia: A 15-year Experience. Clin Lymphoma Myeloma Leuk. 2021; 21: e39-e47.
- Ascioglu S, Rex JH, De Pauw B, Bennett JE, Bille J, Crokaert F, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: An international consensus. Clin Infect Dis. 2002; 34: 7-14.
- Alastruey-Izquierdo A, Mellado E, Peláez T, Peman J, Zapico S, Alvarez, et al. Population-based survey of filamentous fungi and antifungal resistance in Spain (FILPOP study). Antimicrob Agents Chemother. 2013; 57: 3380-3387.
- Hites M, Turcott EWG, Taccone FS. The role of galactomannan testing to diagnose invasive pulmonary aspergillosis in critically ill patients. Ann Transl Med. 2016; 4: 353.
- Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: A meta-analysis. Clin Infect Dis. 2006; 42: 1417-1427.
- Leeflang MMG, Debets-Ossenkopp YJ, Wang J, Visser CE, Scholten RJPM, Hooft L, et al. Galactomannan detection for invasive aspergillosis in immunocompromised patients. Cochrane Database Syst Rev. 2015; 2015: CD007394.
- Tamura H, Arimoto Y, Tanaka S, Yoshida M, Obayashi T, Kawai T. Automated kinetic assay for endotoxin and (1-->3)-beta-D-glucan in human blood. Clin Chim Acta. 1994; 226: 109-112.
- Schmiedel Y, Zimmerli S. Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Wkly. 2016; 146: w14281.
- Elias J Anaissie, Michael R, McGinnis MAP. Clinical Mycology. 2nd edition. Churchill Livingstone/Elsevier; 2009.
- Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: Clinical practice guidelines of the infectious diseases society of America. Clin Infect Dis. 2008; 46: 327-360.
- Nucci M, Anaissie E. How we treat invasive fungal diseases in patients with acute leukemia: the importance of an individualized approach. Blood. 2014; 124: 3858-3869.
- Haleem Khan AA, Mohan Karuppayil S. Fungal pollution of indoor environments and its management. Saudi J Biol Sci. 2012; 19: 405- 426.
- Pagano L, Caira M, Candoni A, Offidani M, Martino B, Specchia G, et al. Invasive aspergillosis in patients with acute myeloid leukemia: A SEIFEM-2008 registry study. Haematologica. 2010; 95: 644-650.
- Reboli AC, Rotstein C, Pappas PG, Chapman SW, Kett DH, Kumar D, et al. Anidulafungin versus Fluconazole for Invasive Candidiasis. N Engl J Med. 2007; 356: 2472-2482.
- Burgos A, Zaoutis TE, Dvorak CC, Hoffman JA, Knapp KM, Nania JJ, et al. Pediatric invasive aspergillosis: a multicenter retrospective analysis of 139 contemporary cases. Pediatrics. 2008; 121: e1286-e1294.
- Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002; 347: 408-415.
- Cordonnier C, Rovira M, Maertens J, Olavarria E, Faucher C, Bilger K, et al. Voriconazole for secondary prophylaxis of invasive fungal infections in allogeneic stem cell transplant recipients: Results of the VOSIFI study. Haematologica. 2010; 95: 1762-1768.
- Even C, Bastuji-Garin S, Hicheri Y, Pautas C, Botterel F, Maury S, et al. Impact of invasive fungal disease on the chemotherapy schedule and event-free survival in acute leukemia patients who survived fungal disease: A case-control study. Haematologica. 2011; 96: 337-341.
- Lien MY, Chou CH, Lin CC, Bai LY, Chiu CF, Yeh SP, et al. Epidemiology and risk factors for invasive fungal infections during induction chemotherapy for newly diagnosed acute myeloid leukemia: A retrospective cohort study. PLoS One. 2018; 13: e0197851.
- Fisher BT, Zaoutis T, Dvorak CC, Nieder M, Zerr D, Wingard JR, et al. Effect of Caspofungin vs Fluconazole Prophylaxis on Invasive Fungal Disease Among Children and Young Adults With Acute Myeloid Leukemia: A Randomized Clinical Trial. JAMA. 2019; 322: 1673-1681.
- Cornely OA, Maertens J, Winston DJ, Perfct J, Ullmann AJ, Walsh TJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007; 356: 348-359.
- Katragkou A, Roilides E. Best practice in treating infants and children with proven, probable or suspected invasive fungal infections. Curr Opin Infect Dis. 2011; 24: 225-229.
- Maertens J, Groll AH, Cordonnier C, de la Cámara R, Roilides E, Marchetti O. Treatment and timing in invasive mould disease. J Antimicrob Chemother. 2011; 66: 37-43.
- Sipsas NV, Kontoyiannis GP. Clinical issues regarding relapsing aspergillosis and the efficacy of secondary antifungal prophylaxis in patients with hematological malignancies. Clin Infect Dis. 2006; 42: 1584-1591.
- Chen CY, Sheng WH, Cheng A, Chen YC, Tsay W, Tang JL, et al. Invasive fungal sinusitis in patients with hematological malignancy: 15 years experience in a single university hospital in Taiwan. BMC Infect Dis. 2011; 11: 250.
- Nicolato A, Nouér SA, Garnica M, Portugal R, Maiolino A, Nucci M. Invasive fungal diseases in patients with acute lymphoid leukemia. Leuk Lymphoma. 2016; 57: 2084-2089.
- Tüfekçi Ö, Y?lmaz Bengoa ?, Demir Yenigürbüz F, Simsek E, Karapinar TH, Irken G, et al. Management of Invasive Fungal Infections in Pediatric Acute Leukemia and the Appropriate Time for Restarting Chemotherapy. Turkish J Haematol. 2015; 32: 329-337.