Excessive Contamination Rate in Blood Culture Obtained Within Two Days after a Prior Contamination: Possible Host Factors
- 1. Departments of Medicine and Pathology, St John Hospital and Medical Center, USA
- 2. Departments of Medicine and Pathology, University of Michigan Health System, USA
Abstract
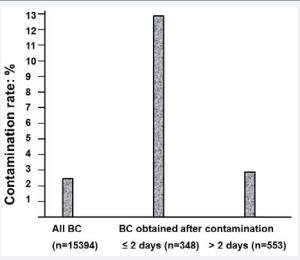
Blood cultures (BC) are often repeated when contamination with commensal organisms is suspected. Subsequent BC contamination rate (CR), however, is unknown. We compared the CR in all BC (n=15394) and BC in patients with a prior contamination (n=901). CR after a prior contamination was significantly higher (6.4% vs. 2.4%; p<0.0001), especially when BC were obtained within two days (12.9%). BC CR in patients with a prior contamination is excessive, implying a role for host factors.
Keywords
• Salvage regimen
• Multidrug resistant HIV
• Foscarnet
• Pegylated interferon
Citation
Simeunovic G, Khatib R, Sharma M, Fakih MG, Johnson LB, et al. (2015) Excessive Contamination Rate in Blood Culture Obtained Within Two Days after a Prior Contamination: Possible Host Factors. Ann Clin Med Microbio 1(1): 1004.
INTRODUCTION
Contamination of blood cultures (BCs), defined as the isolation of a commensal organism in the absence of clinical signs and a potential source, continues to occur despite improved microbiological techniques and remains a problem for the clinicians and the microbiologists [1,2]. The major reasons for BC contamination are thought to be breaches in aseptic technique [3-5]. The contamination rate is significantly lower when BCs are obtained by trained phlebotomists, suggesting that technical aspects are major contributors to contamination [6]. A recent review of the literature reported several factors that lower contamination rates including adherence to an established protocol, peripheral veni puncture, use of sterile gloves, cleaning tops of blood culture bottles with antiseptics, inoculating blood culture bottles before other tubes, samples taken by a phlebotomy team, monitoring contamination rates and providing individual feedback and retraining for those with contaminants [7]. Nevertheless, strict adherence to the guidelines reduces but does not eliminate contamination, implying other causes which may include host factors [1,8]. The median national contamination rate in BC is about 2.5% [3]. It is not clear if additional BCs in patients with contaminations have a similar or higher contamination rate. It is possible that some patients may have heavy colonization of the deeper skin layers or pores, not accessible to disinfectants. In such patients, repeated contamination by the same or different organisms may occur. In this study, we assessed BC contamination in patients with a prior contamination and compared it to the overall contamination rate. Our findings illustrate an excessive rate of subsequent contamination.
METHODS
Facility and case selection
Our hospital is an 804-bed teaching hospital in Detroit Michigan. Our microbiology laboratory receives BCs from the inpatients, the emergency department, affiliated outpatient settings, as well from other affiliated chronic and acute care facilities. We selected all cultures submitted from adult (≥18 years old) inpatients, the emergency departments and affiliated outpatient settings between February 1st 2012 and January 31st, 2013. We excluded pediatric cases (<18 years old), cultures from chronic care facilities and other hospitals. We performed a retrospective evaluation of the results of BCs.
Blood culture methods
The BC system used in our hospital during the study period was the BacT Alert with FA FAN® Aerobic and Anaerobic bottles (bioMerieux) with instructions for 10 ml blood draw/bottle. BCs are usually drawn by laboratory phlebotomists or nursing staff who follow the usual antiseptic procedures for BC drawing that include scrubbing with ChloraPrep (chlorohexidine and isopropyl alcohol; Care Fusion) for 30 seconds followed by air dry for 30 seconds.
Review method
The medical records of patients with positive BCs were retrospectively reviewed. Positive culture for a commensal organism was considered to represent contamination in the absence of a source and clinical signs of bacteremia according to current guidelines [1,9]. Commensal organisms signified organisms recognized as potential contaminants such as coagulase-negative staphylococci, viridans group streptococci, Bacillus spp., Corynebacterium spp., Propionibacterium spp., Aerococcus spp., and Micrococcus spp. Positive cultures with uncertain status (positive culture with a possible source but without clinical signs or clinical signs without a source) were considered true bacteremia. The overall contamination rate was determined. All BC obtained after the first contaminant were evaluated and the rate of subsequent contamination was compared to the overall contamination rate.
Statistical methods
Results were expressed as percentages. Chi square test was used to assess the significance of differences in contamination rates, utilizing the computer software SPSS release 20. P value <0 .05 was considered to indicate statistical significance.
The study was considered a Quality Improvement Project by the St John Hospital and Medical Center Institutional Review Board.
RESULTS
Overall contamination rate
We reviewed 18507 BCs during the study period, 3113 BC were excluded including 2311 cultures from pediatric patients, 788 from other facilities, 10 with insufficient medical records and four line draws. Of the 15394 BCs included, 5388 (35.0%) were obtained by laboratory phlebotomists. Contaminants were recovered from 367 BCs (2.4%) from 308 patients including 43 cultures with mixed contaminants and true pathogens. Contamination rate was slightly higher in cultures obtained by non-laboratory phlebotomists (253 [2.5%] vs. 114 [2.1%]; p=0.05). An additional 67 positive cultures with uncertain status were considered true bacteremia.
Subsequent contamination
Among patients with contaminations, 901 subsequent BCs were obtained from 230 patients within 0-300 days, 348 (38.6%) of which were obtained within two days of the first contaminant. Additional contaminants were recovered from 58 of 901 subsequent BCs (6.4%). Contamination rate in subsequent BCs was highest when cultures were obtained within two days of the first contamination (42/348; 12.9%; p<0.0001) and approached the overall contamination rate afterward (16/553 [2.9%] vs. 2.4%; p=0.4) (Figure 1).
Figure 1: Blood culture (BC) contamination rate: all BCs compared to BCs obtained from patients with a prior contamination within two days or afterward.
The subsequent isolates recovered within two days were identical to the first contaminant in 13/45 (28.9%) isolates recovered from the 42 BC whereas later contaminants were different.
DISCUSSION
These findings illustrate that patients with BC contamination have a high rate of subsequent contamination within two days of the first contaminant. Since the phlebotomists are likely to be diverse, host factors are probably the cause and likely to lead to subsequent contamination. These factors may include skin conditions that lead to colonization of deeper layers not accessible to disinfectants, heavy surface inoculum that may not be adequately decontaminated, or dense bio films resistant to routine disinfection. In support of this assumption, the persistence of skin organisms following the usual scrub with various disinfectants was reported in 1972, presumably protected by follicles, crevices, and lipids [10]. Furthermore, resistance of skin microflora and bio films to the bactericidal action of disinfectants used during blood donation was recently reported [11]. Additionally, the isolation of the same strain of coagulase negative staphylococci in contaminated blood cultures was reported, implying persistent colonization [12,13]. Therefore, distinguishing BC contamination should be based on the patient condition at the time of blood draw, not on the result of additional cultures.
LIMITATIONS
The limitation of our study is its retrospective nature precluding us from assessing the patient condition at the time of contamination to identify which factors contributed to the contamination. Nevertheless, our data illustrate the futility of repeating BCs to verify contamination.
ACKNOWLEDGMENT
The study was supported by St John Hospital and Medical Center Department of Medical Education.
On behalf of all authors, the corresponding author states that there is no conflict of interest.