Life Threatening Vascular Complications of Invasive Focal Sphenoidal Sinusitis: Neuroradiological Diagnostic and Therapeutic Management. A Case Report
- 1. Department of Diagnostic and Interventional Neuroradiology, University Hospital of Tours, France
- 2. Department of Otorhinolaryngology, University Hospital of Tours, France
- 3. Department of Ophthalmology, University Hospital of Tours, France
- 4. Department of Infectious Diseases, University Hospital of Tours, France
Abstract
This case report discusses the presentation, diagnosis, and treatment of a 78-year-old patient with initials symptoms of ocular discomfort, headache, and decreased visual acuity in the left eye. Bone lysis of the sphenoid sinus was initially identified without direct vascular involvement, but subsequently, there was a swift development and progression of a pseudoaneurysm of the internal carotid artery adjacent to the lesion.
Achieving an arterial occlusion of the internal carotid artery enabled the safe biopsy procedures, revealing an infection with A. fumigatus and initiating targeted antifungal therapy.
Mycotic pseudoaneurysms are uncommon, yet their potentially dire progression due to the rapid growth of these lesions necessitates swift and comprehensive management.
Keywords
• Fumigatus
• Mycotic Aneurysm
• Carotid Occlusion Vascular
CITATION
Héloïse I, Thuy-Tran T, Clémence H, Charles A, Fouzi B, et al. (2024) Life Threatening Vascular Complications of Invasive Focal Sphenoidal Sinusitis: Neuroradiological Diagnostic and Therapeutic Management. A Case Report. Ann Clin Med Microbiol 7(1): 1031.
ABBREVIATIONS
A. fumigatus: Aspergillus fumigatus; CNS: Central Nervous System; CRP: C-Reactive Protein; CT: Computed Tomography; PET: Positron Emission Tomography; TEE: TransEsophageal Echocardiography; MR: Magnetic Resonance; ENT: Ear, Nose, and Throat.
INTRODUCTION
Aspergillus species, ubiquitous fungi, can lead to invasive infections, particularly in immunocompromised individuals.
In the case of invasive aspergillosis, central nervous system involvement may be observed either through bloodstream dissemination of spores from pulmonary involvement, or through direct involvement of the skull base from paranasal sinus involvement [1]. Once Aspergillus dissemination reaches the central nervous system, the mortality rate surges from 20% to 30% [2-5]. Moreover, infectious aneurysms affecting cerebral vasculature are rare occurrences, accounting for a mere 2% to 5% of all intracranial aneurysms [6].
Lesions can also affect the intracranial vascular system, causing arteritis with ischemic complications, or mycotic aneurysms with serious hemorrhagic complications [7-10].
We present a case of focal invasive aspergillosis of the sphenoidal sinus leading to a pseudoaneurysm of the internal carotid artery with a very rapid evolution, underlining the importance of rapid angiographic explorations in case of lysis of the sinus bone wall for an adapted interventional neuroradiological therapeutic management.
CASE PRESENTATION
A 78-year-old patient with a medical history of diabetes managed with Metformin, hypertension, and dyslipidemia, who has been undergoing corticosteroid therapy for polymyalgia rheumatica since 2022, presented redness in the right eye and a gritty sensation in the left eye. Additionally, he complains of headaches that had persisted for the past four months.
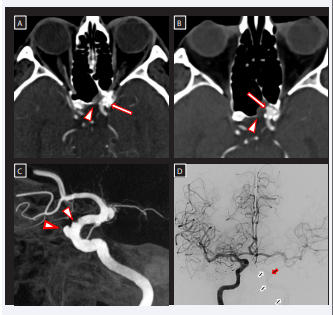
On October 2, 2023, the patient experienced a sudden decrease in visual acuity in the left eye accompanied by ocular pain and the onset of visual blurriness. Subsequently, he awoke on October 3 with complete blindness in the left eye. Upon clinical examination, the patient exhibited symptoms consistent with panuveitis with hypopyon, alongside an unvisualized retina. A diagnosis of endophthalmitis was considered, and ocular samples (aqueous and vitreous humor) were collected for bacteriological analysis. Subsequently, intra-vitreal injections of Vancomycin and Fortum were administered. A CT scan of the paranasal sinuses showed thickening of the mucosa lining the sphenoidal sinus on the left side, with lysis of the bony wall (Figure 1A). There was no apparent involvement of the cavernous sinus or orbital contents.
Figure 1 Figure 1A: Axial Contrast-enhanced CT scan, to investigate the cause of the ocular infection. The examination did not show any intraorbital expansive process but did reveal thickening of the mucosa lining the sphenoidal sinus on the left side, with lysis of the bony wall (arrowhead). There was no lesion of the carotid wall (arrow) containing a few calcifications.
Figure 1B: Postcontrast CT scan performed 4 days later to study lesion evolution. The examination revealed an increased in tissue infiltration of the sphenoidal mucosa (arrowhead) and the emergence of a pseudoaneurysm on the internal carotid artery (arrow).
Figure 1C: Arteriography performed 3 days after the last scan (left internal carotid artery, lateral view). It showed the rapid growth of the aneurysm at the level of the carotid siphon (thick arrowhead) and the appearance of irregularities in the arterial wall (thin arrowhead) testifying to the rapidly evolving invasion of the arterial wall, indicative of necrotizing vasculitis.
Figure 1D: Frontal angiography after opacification of the right internal carotid artery at the end of the neurointerventional treatment. The left sylvian axis is revascularized through the anterior communicating artery once the left carotid axis is occluded (black and white arrows), as well as the threatening pseudoaneurysm (red and white arrow)
On October 3, empiric antibiotic therapy was initiated with Imipenem and Levofloxacin, given the clinical presentation of endophthalmitis. C-reactive protein (CRP) levels were within the normal range, but the patient displayed elevated white blood cell count (15.5 g/L). Multiple specimens were collected, and antigen tests conducted on 06/10/2023, using serum and involving measurements of galactomannan and 1-3-Beta-D-Glucan, turned out to be negative.
Subsequent follow-up imaging CT 4 days later showed the development of a microaneurysm of the internal carotid artery adjacent to the bone lysis (Figure 1B). Biopsy of the pathological sphenoidal tissue was not recommended because of the risks associated with the presence of the internal carotid artery just posterior to the mucosal infiltration.
Cerebral angiography was performed 3 days after the last scan to assess therapeutic options. It showed the rapid growth of the aneurysm at the level of the carotid siphon (from 2 to 3 mm in height) and the appearance of irregularities in the arterial wall (Figure 1C), suggesting an arterial invasion and the risk of cataclysmic bleeding into the sphenoid sinus.
On October 11th, a balloon occlusion test of the pseudoaneurysm’s supporting axis was performed under local anesthesia, with a successful revascularization of the left carotid axis through both the anterior and posterior communicating arteries.
Following a collegial and multidisciplinary team discussion, an occlusion (Figure 1D), of the aneurysm and the feeding artery was subsequently carried out on October 12th.
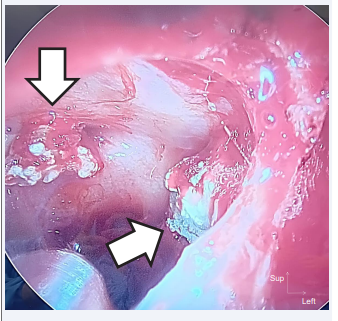
On October 13th, the patient underwent a sphenoidotomy procedure to obtain multiple biopsies. The study revealed mycelial filaments upon direct examination and fluorescence, along with the identification of an A. fumigatus in mycological cultures at 30 and 35°C (Figure 2).
Figure 2: Perioperative endoscopic view of the right sphenoidal sinus. A. fumigatus spores (black and white arrows).
A probabilistic antifungal treatment with liposomal amphotericin B was initiated immediately following the biopsy, despite the absence of documentation at that time (negative fungal cultures, serologic testing, PCR Aspergillus in blood). The diagnosis of invasive aspergillosis was only confirmed on October 15th.
Subsequently, on October 17, a vitrectomy was performed, and samples were obtained from the posterior vitreous chamber and anterior chamber. Intravitreal injections of Fortum and Amphotericin B were administered, along with subconjunctival Celestone. The patient did not show clinical improvement after the second intra-vitreal antibiotic injection. Mycological culture performed on the vitrectomy sample collected on the 17th of October also tested positive for A. fumigatus. Intraoperative findings revealed signs of retinal necrosis with retinal detachment. At this stage, progression towards functional loss was conceivable. Voriconazole was then initiated as systemic antifungal treatment [11].
To exclude endocarditis as a potential source of the infection, the patient underwent both a positron emission tomography (PET) scan and a transesophageal echocardiography (TEE), both of which did not reveal any evidence supporting endocarditis.
At three months, both clinical and biological progress showed improvement under the prescribed treatment.
DISCUSSION
Aspergillus is a common mold that typically causes morbidity and mortality in immunocompromised patients. It is also the most frequent cause of paranasal sinus mycoses [12]. These localized infections are linked to ulceration and destruction of the sinuses, involving bone erosion and spread to adjacent structures [1,12], such as the orbit and the vascular wall of the carotid.
Guidelines exist regarding the initiation of systemic treatment in addition to intra-vitreal therapy [13], as was done in our case. However, there are no established standards to guide invasive treatment for intracranial mycotic aneurysms. Therapeutic approaches for intra-cavernous mycotic aneurysms primarily involve endovascular methods [8,9,14]. This involves either occluding the pseudoaneurysm and the feeder artery using coils, which necessitates satisfactory collateral circulation via the circle of Willis or resorting to stenting in case of insufficiency of the circle of Willis. Due to the vessel’s tortuosity in cavernous segment, a less compliant covered stent cannot be deployed across the lesion. Treatment with one or more flow-diverting stents can be considered, bearing in mind the delayed artery healing, posing a risk for urgent ENT procedure, and the need for dual antiplatelet therapy, which may prove challenging to manage in this surgical setting. Additionally, any exogenous material (such as stent or coil) may lead to bacterial colonization, potentially causing a graft infection, requiring prompt sampling for the initiation of rapid anti-infective therapy.
Concern of endophthalmitis warrants investigating a sinus infection. If there’s suspicion of a sphenoidal infectious lesion, particularly of aspergillus origin, and if there’s evidence of sinus bone wall erosion near a vascular structure, urgent vascular exploration (via angioscan or angioMR) is recommended. The discovery of arterial lesions testifying to vascular invasion requires specific management in order to prevent the risk of cataclysmic arterial rupture, while in certain cases, such as ours, allowing samples to be taken for etiological purposes.