The Impact of Covid-19 on the Diagnosis of Gynecological Cancers in the Post-Pandemic Era: An Integrative Review
- 1. FAMINAS-BH, Brazil
- 2. UNI-BH, Brazil
- 3. Department of Gynecology and Obstetrics, Hospital Vila da Serra, Brazil
- 4. Oncoclínicas, Brazil
Abstract
The COVID-19 pandemic has impacted the dynamics of health systems, including limiting activities to prevent and diagnose gynecological cancers in primary care. This study aims to understand the extent of the consequences of the pandemic period on gynecological cancers in terms of diagnosis and prognosis. The method in this research was an integrative review based on the search of publications in PubMed, SciELO, and BVS from January 2020 to June 2023, with three exclusion moments and a final sample of 9 articles. The results indicated avoidance of consultations due to fear of the virus, postponement of evaluation exams, interruptions of screening and vaccination procedures, establishment of non-priority staging, postponement of surgeries, priority to conservative treatments, and decline in diagnoses during the pandemic. It is concluded that the pandemic event impaired women’s health care in the context of gynecological cancers, which calls for measures to adapt to primary and secondary care.
Keywords
• Genital Neoplasms
• Female
• COVID-19
• Diagnosis
• Neoplasm Staging
• Medical Oncology
Citation
Amaral APA, de Azevedo LAR, Nunes MM, Giannecchini GV, Vieira CM (2024) The Impact of Covid-19 on the Diagnosis of Gynecological Cancers in the Post-Pandemic Era: An Integrative Review. Ann Community Med Pract 9(1): 1054.
INTRODUCTION
According to the National Cancer Institute, neoplasms are a public health issue worldwide, ranking among the leading causes of premature death [1]. As the population ages and life expectancy increases, the incidence of cancer has been on the rise, consequently leading to increased morbidity and mortality [1]. Currently, cancer staging holds significant importance in guiding treatment based on the extent of the lesion. The most commonly used system in Western countries is TNM, as recommended by the International Union Against Cancer and the American Joint Committee on Cancer [2].
The public healthcare system’s access to oncology treatment resources is limited, especially in less developed countries [3]. Another limitation is the low access to general tumor diagnostic services, which is also related to lower socioeconomic development [3-5]. When combined with the prospect that cancer will become the leading cause of death in these countries in the future, it becomes a concerning issue in Latin America [5].
The most prevalent tumors in females, excluding skin cancer, are breast cancer and cervical cancer, which fall under gynecological tumors [1,6]. Additionally, other female cancers are notable in the oncological landscape, such as uterine and ovarian cancer. This class is responsible for significant morbidity and mortality and is expected to grow even further [1]. Under the same perspective, it was expected that in Brazil, new cases of gynecological neoplasia would be around 16.35 per 100,000 women between 2020 and 202 [6].
However, at the end of 2019, a new coronavirus was identified as the cause of acute respiratory infections. It spread rapidly, resulting in a pandemic. In January 2020, the World Health Organization declared it a public health emergency of international concern [7]. From that point, it impacted healthcare systems, as resources were redirected, and internal reorganization took place to address COVID-19-related diseases. This primarily affected primary care, limiting activities and reducing the population’s access to healthcare services, especially concerning gynecological cancers, regarding prevention and diagnosis methods [6,7,8]. As for access to healthcare, the impact extended beyond that, also causing reluctance among the population to seek care at healthcare centers [6].
In seeking to quantify the direct and indirect effects of the pandemic, it became evident that there was an impact on the treatment of various types of cancer due to the reorganization of healthcare services [7,8]. Therefore, this study aims to describe the extent of the effects of COVID-19 on patients with gynecological cancer and understand the changes caused in the realm of diagnosis through an integrative review. This is to provide scientific evidence for planning women’s healthcare and mitigate the deficits caused.
METHODOLOGY
This is an integrative review of the literature on the change in the diagnostic pattern of gynecological tumors during the COVID-19 pandemic. Six stages organize the article: formulation of the research question, bibliographic search, data extraction, critical evaluation, analysis and summarization of studies, and synthesis of knowledge.
The research question was based on medical observation and experience, in which it was possible to inquire about a significant and possible change in the staging and number of diagnoses of gynecological cancers in the post-pandemic era to establish a relevance aimed at alerting the population.
The search for studies took place in July 2023 in the databases that make up the Virtual Health Library (VHL), the Scientific Electronic Library Online (SciELO), Medline via PUBMED, and Google Scholar. The search for data on Medline via VHL versus PUBMED presented divergent results. For this reason, both search engines were used to analyze the results. The choice of databases considered the scope and affinity with the theme.
For a broad search in the literature, the strategies combined the controlled descriptors “Female Genital Neoplasms,” “COVID-19,” and “diagnosis” included in the latest version of the Health Sciences Descriptors (DECS), which has an interface with the Medical Subject Headings (MESH). These descriptors were used in Portuguese in the VHL search route and English in PUBMED, combined using the Boolean operator AND. In the SciELO, the same method did not present results, and thus, the strategies for the combination of the controlled descriptors “Neoplasm Staging,” “COVID-19,” and “Gynecology” and their derivatives included in the latest version of the Health Sciences Descriptors (DECS) reformulated interconnected by the Boolean operator AND and OR, respectively.
Original articles, cross-sectional or mixed-methods studies, in English/Spanish/Portuguese, published between January 2020 and June 2023, whose data collection includes the pandemic period and that dealt with the research theme, considering possible justifications and influences on the investigated change, were included.
Publications presented in the form of thesis, dissertation, book chapters, reflections, case reports, preprints, studies with intervention, as well as duplicate publications in the databases, which did not refer to the theme or population of the research or that did not answer the guiding question, were excluded.
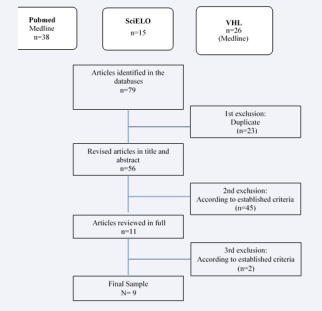
There were three moments of exclusion: first, of duplicate publications through the titles, a second stage by reading the title and abstract, and finally, after reading the texts in full. For mapping, the publications were exported to Excel ® software and organized and summarized in a table prepared by the authors. The data summary is presented in a flowchart constructed with the support of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol10 and the report of the results of the articles in tables with descriptive analysis (Table 1).
Table 1: Characterization of the studies. The table summarizes the results of the sample analyzed according to authorship, year of publication, journal, and description of the results.
|
N |
Authorship / Year of publication |
Newspaper |
Results |
|
01 |
Bourne T et al.¹º / 2020 |
Ultrasound Obstet Gynecol |
To manage resources during the pandemic, avoiding the necessary contact between medical staff and patients, and thus preventing the spread of the virus, the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) has guided the screening of gynecological ultrasound services. Postponement of 2 to 4 weeks was oriented in cases of abnormal uterine bleeding (postmenopausal and postcoital), abdominopelvic mass (high risk of malignancy according to the IOTA-ADNEX model ≥ 10%), ultrasound staging for biopsy-proven or incidentally diagnosed gynecologic malignancy if useful for management, signs of recurrent gynecologic malignancy, family history of gynecologic malignancy with genetic predisposition. In addition, could be postponed until after the end of the pandemic: Abnormal, non-severe uterine bleeding in non-postmenopausal patients (from disruption during the use of hormonal medication, menorrhagia without associated anemia, oligomenorrhea, intermenstrual or irregular bleeding and in perimenopause), non-acute pelvic pain (chronic, cyclic dyschezia, dysmenorrhea, dyspareunia), family history of gynecologic malignancy without known or identified genetic predisposition, incontinence, infertility and recurrent pregnancy loss, prolapse, revision of previously observed probably benign adnexal pathology (unilocular cyst, endometrioma, dermoid/mature cystic teratoma, hemorrhagic ovarian cyst, hydrosalpinx, low risk of malignancy according to the IOTA-ADNEX model (<10%), revision of previously observed pelvic pathology (uterine polyp, leiomyoma, adenomyosis, endometriosis), revision of the intrauterine contraceptive device and powders Treatment of gynecologic malignancy with no signs or symptoms of recurrence. Finally, any woman with probable or confirmed COVID-19 should be asked not to attend the facility. However, if assessment is necessary, they should be cared for in a designated COVID-19 area. |
|
02 |
Martinelli F et al.¹ / 2020 |
International Journal of Gynecologic Cancer |
Despite the study's restrictions, it showed a significant postponement of the treatment of some already diagnosed conditions, mainly when patients tested positive for COVID-19. The survey received 20,836 views; 30% responded, of the total of 187 physicians surveyed in 49 countries. For most respondents (97.3% or 182/187), COVID-19 affected or changed their practices. Between 25% (26/102) (before medical treatment) and 16% (27/165) (before surgery) did not ask for any tests to rule out COVID-19 infection among patients. Most respondents said they did not change treatment indications if patients were negative for COVID-19; if patients were positive for COVID-19, they had treatment postponed. Treatments were prioritized for high-risk uterine cancer at an early stage (85/187; 45%), locally advanced cervical cancer (76/187; 41%), and newly diagnosed epithelial ovarian cancer (76/187; 41%). According to 49% (91/187) of answers, treatment for early-stage low-grade endometrial cancer was postponed, with hormonal treatment as a therapy option (31%; 56/178). The majority of the physicians ( 77% or 136/177) reported no changes in (surgical) treatment for early-stage cervical cancer in COVID-19-negative patients, while delayed treatment by 54% (96/177) of respondents if the patient tested COVID-19 positive. Uterine cancer: They considered treatment postponeable in 59%, 44%, and 41% of COVID-19-positive patients with low-grade early-stage endometrial cancer, early-stage high-risk endometrial cancer/sarcoma, and advanced- stage endometrial cancer, respectively; Epithelial ovarian cancer: On the other hand, surgery (whether with staging or diagnosis) was not considered in 41% of women with positive COVID-19 versus 8% if negative COVID-19 with early-stage epithelial ovary; Cervical cancer: treatment was delayed according to 47% and 15% of respondents among COVID-19 positive and COVID-19 negative patients, respectively. Vulvar cancer: Surgical treatment was considered postponable by 54% of respondents when at an early stage if it was positive for COVID-19, while it was considered by 78% of respondents if it was COVID-19-negative. |
|
03 |
Cohen, Megan A et al.? / 2020 |
Am J Obstet Gynecol. |
Social distancing requirements disrupt routine screening for breast and cervical cancer; patients at average risk of breast cancer can likely postpone routine mammography until the risks of pandemic conditions decrease, as suggested by experts. Screening in high-risk women, including women known to carry breast cancer genes less than 40 years of age, may be delayed, but there should be reconsideration about this if they expect a delay of more than six months. Women with BI-RADS 4 or 5 lesions that require diagnostic imaging or breast biopsy should receive priority for breast imaging. According to the American Society of Colposcopy and Cervical Pathology (ASCCP), postponement of colposcopy for patients with low-grade squamous intraepithelial lesions (SIL) for 6 to 12 months, possible postponement of diagnostic or excisional procedures for patients with suspected or known high-grade SIL for up to 3 months, and attempted evaluation of those with the alleged invasive disease within four weeks of initial pathology results, emphasizing human papillomavirus (HPV) testing for individuals over 30 years of age and the role of primary HPV testing with or without reflex cytology. Social distancing protocols reflected in the postponement of cancer screening measures even when there was considerable suspicion. |
|
04 |
Tsibulak, Irina et al.²? / 2020 |
Int J Gynecol Cancer. |
Austria observed a sharp decline in newly diagnosed gynecological tumors since the COVID-19 pandemic lockdown—two-thirds of patients diagnosed during the COVID-19 pandemic had tumor-specific symptoms. Half the patients diagnosed during the pandemic had no comorbidities compared to 35% in the period before the pandemic. During the COVID-19 pandemic, the median age of patients was lower than that of patients diagnosed with cancer in 2019. In gynecologic tumors, there were no differences in tumor stage, while in breast cancer patients, there was a decline in stage T1 besides stage T2–T4 tumors (-11% and -10%, respectively, NS). At the time of diagnosis, there was no change in the staging tumor before and after confinement. However, the observation period in this study may be too short to observe a stage change. |
|
05 |
Leibold, Aurora et al.³ / 2021 |
Curr Treat Options Oncol |
Initial data from New York City, the initial epicenter in the U.S., shows that more than 38% of gynecologic cancer patients experienced a modification in their treatment due to COVID-19 during the peak of the New York pandemic. Regarding primary and secondary prevention of cervical cancer, COVID-19 has disrupted HPV vaccination schedules and delayed outpatient screening with HPV cytology/testing and subsequent referrals for colposcopy. While there is no routine screening for vulva, endometrial, or ovarian cancer, early studies have shown that there have been delays in diagnosis secondary to patients with early symptoms who waited longer than usual to make appointments with their doctor due to fear of contracting COVID-19. |
|
06 |
Nikolopoulos, Manolis et al.³ / 2022 |
Arch Gynecol Obstet. |
The COVID-19 pandemic has significantly affected clinical practice. The neoplasm staging is the most crucial factor in prognosis, survival, recurrence rate, and treatment decision. However, no systematic review has reached a conclusive agreement on the effect of delayed treatment on different types of cancer. While the literature is replete with expert opinions addressing the potential impact of COVID-19 on oncology practice, only little data on the effect of COVID-19 on patients affected by cancer is still available. Mortality from COVID-19 infection is higher in patients with gynecologic cancer than in patients without cancer, with two studies reporting a mortality rate of 14% [8, 12] and one reporting a rate of 38% [13]. In this latest study, which compared mortality between various types of cancer, gynecologic patients had the third-highest mortality rate after pancreatic and lung cancer. The cancer diagnosis was affected. In three identified studies, there was a statistically significant reduction in the number of patients diagnosed with gynecologic cancer during the pandemic compared to patients during the same months in 2019. They reported impact and delay in management. The percentage of patients who experience delayed treatment is consistently greater than 10% in the identified studies, with the majority of them surgical treatment. There is also a movement towards conservative management, with hormonal therapy in endometrial cancer and neoadjuvant chemoradiotherapy in cases that, before the pandemic, would be treated with primary surgery. Despite preventive measures, surgical management has changed with an increase in the rate of laparotomies compared to laparoscopies. The consensus of the published articles is that with adequate preventive and protective measures, oncological surgery is possible and does not significantly compromise patients or health professionals. A recently published systematic review estimated the increased risk of death after delayed treatment of seven main types of tumors, bladder, breast, colon, rectum, lung, cervix, and head and neck, in all three treatment modalities (surgery, systemic treatment, and radiation therapy). A delay in treatment, regardless of the modality, of more than four weeks increases the risk of death. Another retrospective review of the national cancer database of the United States of more than 200,000 patients found that a delay of more than eight weeks in surgical treatment of low-grade endometrial cancer was independently associated with worsening 5-year survival. |
|
07 |
Antunes, Dora et al.?/ 2022 |
Medicine (Kaunas) |
A study by Cancer Research United Kingdom (CRUK) reported a substantial impact of the COVID-19 pandemic on cancer diagnosis, with more than 350,000 fewer people than usual referred for suspected cancer between March and September 2020. Part of this is due to fewer people seeking primary care. In addition, a global modeling analysis suggested that about 38.0% of cancer surgeries and 82.0% of benign surgical procedures would have been canceled or postponed during the peak 12 weeks due to the COVID-19 pandemic. Although some differences were reported in this study regarding tumor histology in endometrial and ovarian cancers, with some aggressive tumors being diagnosed more frequently in the pandemic recovery group, tumor staging did not differ significantly between groups. A previous report demonstrates similar patient and tumor characteristics for cervical, endometrial, ovarian, and vulvar cancers during the pre and post-pandemic periods. However, there were more records at a higher rate of advanced- stage cervical and ovarian cancer in the pandemic period (2020). |
|
08 |
Nakayama, John et al.? / 2020 |
Gynecologic oncology |
The study analyzed the responses of 331 gynecologic oncology service providers to anonymous surveys sent by email to members of the Society of Gynecologic Oncology (SGO). COVID-19 is widespread and has radically altered patterns of practice. Despite COVID-19 concerns, most gynecological cancer care continues. However, the sharp decline in clinical volume shows that many patients are exempt from diagnosis or have postponed treatment. Practice volume dropped by more than 60% due to COVID-19 – The average number of patients treated per week decreased by 61.6%, going from an average of 42.59 to 16.34 patients per week. They indicated the highest level of concern (5 out of 5) for the following: 107 (39.6%) for delay in care, 93 (34.4%) for access to medical supplies, 70 (26.0%) for access to cancer treatments, 59 (21.9%) for access to blood products, 49 (18%) for quality of care, and 30 (11.1%) for access to medicines. When asked which type of gynecologic cancer would be most affected by COVID-19, most of the interviewees answered ovarian cancer (52.8%). Next was uterine cancer (30.0%), and they considered cervical cancer to be the least affected (14.8%). The study invited the participants to choose the three biggest challenges after COVID-19 de-escalation. Surgical delay (58.6%) was the most common choice. |
|
09 |
Singh, Nilanchali, et al.³ / 2022 |
Cancer control: Journal of the Moffitt Cancer Center |
The American College of Surgeons (ACS) has argued that delaying cancer surgeries could cause more harm than good to patients. The study carried out a critical analysis of surgical procedures to determine the risks of spreading infections. Professionals must weigh the risk of laparoscopic surgery versus pneumoperitoneum in the COVID-19 pandemic against the risk of laparotomy. However, some studies advocate minimally invasive surgeries in favor of open surgeries due to fewer postoperative complications, shorter hospital stays, and less spread of COVID-19 in inpatient wards. One can consider laparoscopy if the benefits outweigh the risks, with the utmost attention to the safety of healthcare personnel. The Society of Gynecologic Oncology states that accurate triage is essential to maintain harmony between existing resources and protect staff and patients. Decisions regarding the procedure of semi-urgent and elective surgeries require the participation of the state health department and the levels of the hospital system at the primary level. During the planning of procedures with adequate documentation, there must be informed consent, mutual decision- making with patients, and counseling patients about the harms of surgical delay compared to COVID-19 cross-infection in the hospital. |
Ethical aspects were respected, with reliable citations of the authors’ sources and definitions.
RESULTS
Seventy-nine publications were identified in the databases, 38 in Medline via PUBMED, 15 in SciELO, and 26 in the VHL databases (all in Medline). In the first moment of deletion, 23 duplicate publications were removed. In the second moment, after reviewing the title and abstract, 45 articles that did not answer the research question were excluded. Finally, after reading the full article, two publications were excluded because they were not accessible completely, so the rest met the inclusion criteria. The flowchart of the selection of articles is in Figure 1.
Figure 1: The figure shows the process of searching and selecting the articles based on three moments of exclusion and the established criteria.
The sample consisted of 9 articles published between 2020 and 2022, 3 in 2022, 1 in 2021, and 5 in 2020, all in English.
DISCUSSION
The rapidly expanding COVID-19 pandemic has impacted all areas of daily life, including healthcare, directly interfering with diagnoses by disrupting primary and secondary care [8]. This leads to limited activities, the reassignment of healthcare professionals, and reduced patient access to facilities due to containment measures and fear of contagion [8].
In this context, this study sought to investigate the limitations these interferences caused in diagnosing gynecological tumors during this event. The evidence gathered pointed to a decline in the diagnosis of gynecological cancers during the study period [12,13-16]. It was reported that ovarian cancer was the most affected gynecological cancer by the pandemic [16].
Several justifications for this decrease in medical care were identified, including delays in assessment exams for lower malignancy risks, such as ultrasounds, mammograms, CT scans, diagnostic procedures, and interruptions in routine screenings and prevention measures like vaccination [9,11,13].
Patients also played a role in this event, seeking investigation only after the onset of symptoms rather than through secondary prevention strategies. There was also increased waiting time for appointments after the presence of symptoms due to the fear of contracting COVID [12,13].
Regarding treatment, various delays occurred due to the postponement of treatments in patients testing positive for COVID-19 and for stages deemed non-priority, with oncological surgeries categorized as semi-urgent and priority given to hormonal treatments over surgical procedures [10,11].
There were differences in tumor staging, with some authors reporting a higher rate of advanced-stage cervical and ovarian cancers during the pandemic period [15]. Others said similar stages to pre-pandemic levels and predicted that there would be diagnoses with more advanced stages in the future [12,16].
Some reported a decline in the diagnosis of initial stages of breast cancer, and secondary prevention measures, as mentioned earlier, were postponed [12,15].
The main factors that positively interfered with tumor staging are related to the duration of the study, as it becomes difficult to measure the consequences that are yet to come three years from the start of the pandemic [12]. Another factor relates to the acute event that occurred, leading to an emergency response that caused delays in diagnostic procedures [9, 11,13,14,16,17].
Therefore, it is inferred that the pandemic harmed the diagnosis and treatment of gynecological cancers, causing delays in both. This factor may have led to the neglect of women’s health. Future impacts are still concerning, such as the diagnosis of neoplasms in more advanced stages, which may no longer have treatment alternatives.
To mitigate these consequences, it is crucial for healthcare services, especially primary care, to increase primary prevention and screening strategies for these neoplasms and strengthen primary care to provide more significant opportunities for diagnostic investigations. Additionally, reinforcing secondary care through increased availability of diagnostic exams is essential to compensate for the delays in waiting lists caused by the pandemic.
CONCLUSION
The present study finds that social distancing requirements have hindered screening routines for breast and cervical câncer [11], HPV vaccination schedules, outpatient screening with HPV cytology/testing, and subsequent referrals for colposcopy [13], as well as procedures such as ultrasound, which determined many conditions to be postponable [9]. Regarding the queries, the practice volume dropped by more than 60%, and delays in care were reported as their biggest concern [16].
Undoubtedly, mortality from COVID-19 infection is significantly higher in patients with gynecologic cancer than in patients without câncer [14]. Due to the precautions to prevent the spread of the virus prescribed worldwide, there was a favor to postponing the surgical condition. Congruent to this panorama, the present study showed that there was, in a global scenario, a significant postponement of the treatment of some conditions already diagnosed, mainly when patients tested positive for COVID-19 [10], in addition to a tendency to prefer conservative treatment, such as hormonal treatment [9]. However, as mentioned, the risk of death increases after a delay of 4 weeks, regardless of the treatment modality, and a delay of more than eight weeks in the surgical treatment of low-grade endometrial cancer was independently associated with worsening 5-year survival [14]. With this article, we can observe the position of societies such as the American College of Surgeons (ACS), which argued that delaying cancer surgeries could cause more harm than good to patients [17], and the Society of Gynecologic Oncology which highlighted the importance of informed consent and mutual decision-making with patients, along with advising patients on the harms of surgical delay compared to COVID-19 cross-infection in the hospital [17].
With the study, it was possible to identify regions already registered with lower diagnoses of such types of cancers in the pandemic period. There was no significant difference in tumor staging compared to previous periods. Although there has been a need for further studies in the area in recent years since, as demonstrated, there are numerous factors that contribute to the diagnostic delay and, consequently, to the worse expectations of staging to the diagnosis, being a warning theme for both primary and secondary care, to mitigate the impact already constituted, but still amenable to interventions.
ACKNOWLEDGMENT
We acknowledge Dr. Carolina Martins Vieira for supporting us in drafting the manuscript.
REFERENCES
- Martins M, Co-Autoras: T, De A, Bezerra De Melo B, Alice M, Guedes S. Instituto De Medicina integral Prof. Fernando Figueira Qualidade De Vida Em Pacientes Idosas Com Neoplasias Ginecológicas E De Mama Como Fator Preditivo De Óbito Precoce: Estudo De Coorte Prospectiva Quality of life in elderly Women with Gynecological and Breast Tumors as Predictive Factor of early Death: Prospective Cohort Study. 2023.
- Paulo M, Sanches R, Matsubara A, Aurélio M, Grande A, Luiz, et al. Lavado peritoneal em neoplasias ginecológicas Peritoneal washing in gynecological neoplasias. 2019; 55: 20-31.
- Vieira CM, Diniz PHC, Dizon DS, Nogueira-Rodrigues A. Patient navigation (PN) support to timely access to radiotherapy in the Brazilian public health system. Support Care Cancer. 2023; 31: 182.
- Seoud M, Lundqvist E, Fujiwara K. Terapia-alvo em neoplasias ginecológicas: pronto para o horário nobre?. 2015.
- Ferrara P, Dallagiacoma G, Alberti F, Gentile L, Bertuccio P, Odone A. Prevention, diagnosis and treatment of cervical cancer: A systematic review of the impact of COVID-19 on patient care. Prev Med. 2022; 164: 107264.
- Nutrición Hospitalaria - Arán Ediciones, S.L.
- UpToDate. www.uptodate.com.
- Cruz-Castellanos P, Ortiz-Cruz E, Sánchez-Méndez JI, Tapia M, Morera R, Redondo A. Impacto de la primera ola de la pandemia de COVID-19 en la atención a pacientes oncológicos en un hospital terciario. Rev Esp Patol. 2022; 55: 77-84.
- Bourne T, Leonardi M, Kyriacou C, Al-Memar M, Landolfo C, Cibula D, et al. ISUOG Consensus Statement on rationalization of gynecological ultrasound services in context of SARS-CoV-2. Ultrasound Obstet Gynecol. 2020; 55: 879-885.
- Martinelli F, Garbi A. Change in practice in gynecologic oncology during the COVID-19 pandemic: a social media survey. Int J Gynecol Cancer. 2020; 30: 1101-1107.
- Cohen MA, Powell AM, Coleman JS, Keller JM, Livingston A, Anderson JR. Special ambulatory gynecologic considerations in the era of coronavirus disease 2019 (COVID-19) and implications for future practice. Am J Obstet Gynecol. 2020; 223: 372-378.
- Tsibulak I, Reiser E, Bogner G, Petru E, Hell-Teutsch J, Reinthaller A, et al. Decrease in gynecological cancer diagnoses during the COVID-19 pandemic: an Austrian perspective. Int J Gynecol Cancer. 2020; 30: 1667-1671.
- Leibold A, Papatla K, Zeligs KP, Blank SV. COVID-19 and Gynecologic Oncology: What Have We Learned? Curr Treat Options Oncol. 2021; 22: 117.
- Nikolopoulos M, Maheshwari MK, Doumouchtsis SK, CHORUS: An International Collaboration for Harmonising Outcomes, Research and Standards in Urogynaecology and Women’s Health. Impact of COVID-19 in gynaecological oncology care: a systematic rapid review. Arch Gynecol Obstet. 2023; 305: 555-565.
- Antunes D, Mendonça L, Melo Â, Gonçalves S, Nogueira Martins F, Nogueira Martins N. Impact of the COVID-19 Pandemic on Diagnosis and Management of Gynecological Cancer: A Single-Center Analysis. Medicina (Kaunas). 2023; 58: 1862.
- Nakayama J, El-Nashar SA, Waggoner S, Traughber B, Kesterson J. Adjusting to the new reality: Evaluation of early practice pattern adaptations to the COVID-19 pandemic. Gynecol Oncol. 2020; 158: 256-261.
- Singh N, Mishra N, Jayraj AS, Ghatage P. Management of Gynecologic Cancer During COVID-19 Pandemic: South Asian Perspective. Cancer Control. 2022; 29: 107327482211193.