Acute High Cervical Disc Herniation: A Confounding Presentation and New Algorithm to Ensure Correct Diagnosis
- 1. Department of Orthopaedic Surgery, Oregon Health and Science University, USA
- 2. Department of Orthopaedic Surgery, Broward Health Medical Center, USA
- 3. Department of Orthoapaedic Surgery, Massachussetts General Hospital, USA
- 4. Department of Orthopaedic Surgery, Maryland Spine Center at Mercy Hospital, USA
Abstract
High cervical disc herniation (C2/3 and C3/4) is a rare and potentially debilitating injury. Most cervical disc herniations occur at C5/6, or C6/7; less than 1% occurs at C2/3 and only 4% to 8% at C3/4. Patients with a high cervical disc herniation can present with headache, neck pain, and unilateral numbness and weakness. Diagnostic tests such as non-contrast computed tomography (CT) of the brain and angiogram of the neck are commonly utilized to rule out cerebral vascular accident (CVA) and/or carotid artery dissection; these pathologies can present with similar symptoms, however these commonly obtained tests will often fail to diagnose a high cervical disc herniation.
We present a review of the literature regarding the incidence of high cervical disc herniation and its clinical manifestations. Differences in the signs and symptoms of CVA, carotid artery dissection, and high cervical disc herniation are discussed. A case of a 57-year old male who presented with headache, neck pain, and left sided deficits secondary to a high cervical disc herniation is also reviewed.
Keywords
Cervical disc; Cervical spine surgery; Discectomy; Spinal decompression surgery; Cervical disc herniation; Cervical; Spine; High disc herniation; Stroke; Dissection; CTA; MRA
Citation
Kunkle WA, Ameri BJ, Madden MO, Hershman SH, Park JJ (2018) Acute High Cervical Disc Herniation: A Confounding Presentation and New Algorithm to Ensure Correct Diagnosis. Ann Emerg Surg 3(1): 1027.
INTRODUCTION
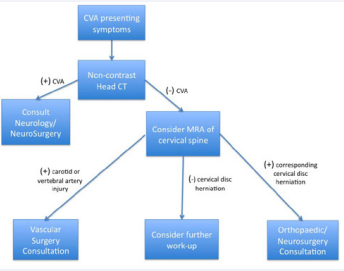
The majority of cervical disc herniations are known to occur at C5/6, and C6/7 [1], less than 1% of all cervical disc herniations are found to occur at C2/3 [2] and only 4% to 8% at C3/4 [1,3]. The presentation of high cervical disc herniations can mimic other, more common pathologies and delay a timely diagnosis. Like symptomatic disc herniations elsewhere in the cervical spine, the surgical management of C2/3 disc herniations often involves decompression of the spinal canal and stabilization of the involved motion segments. A review of the literature is presented and an algorithm (Figure 1) to aid in the diagnosis and management of this condition is proposed.
Figure 1: Proposed algorithm for the work-up of a patient with suspected CVA, carotid artery dissections, and/or high cervical disc herniation.
CASE PRESENTATION
A 57-year-old male with a history of hypertension, diabetes mellitus, and hyperlipidemia presented to the emergency department (ED) with a two day complaint of headache, neck pain, and left sided weakness and numbness. The patient noted he was ambulatory during the early morning hours, however, upon waking described a loss of motor strength and sensation in the left upper and lower extremity. Upon presentation to ED at 8am the patient was noted to have 0/5 motor strength and an absence of sensation in the left upper and lower extremities; the right sided extremities were neurologically intact. The patient did not display any facial droop, his speech was clear, and all extra ocular movements were intact. A CT of the head failed to reveal intracranial hemorrhage and MRI of the brain showed no acute abnormality. Six hours after presentation, the patient was noted to have decreased strength and loss of fine motor control in the right upper and lower extremities; the patient’s left side remained flaccid. Deep tendon reflexes were 2+ and equal bilaterally in all four extremities. Babinski sign was down-going bilaterally and plantar reflexes were intact. A computed tomography angiogram (CTA) of the neck showed no internal carotid artery stenosis or dissection; moderate degenerative changes in the cervical spine were noted. Ten hours after presentation, the patient complained of acute dyspnea and exhibited complete paralysis of all four extremities. CPR was initiated and the patient was intubated. Sixteen hours after presentation, an MRI of the cervical spine was performed which revealed a large disc herniation (Table 1)
Table 1: Cases of Cervical Intradural Disc Herniations. Intradural cervical disc herniations are rare (Iwamura). Marega was the first to report an intradural cervical disc herniation in 1959 and to date only 32 cases of intradural cervical disc herniations have since been reported in the literature (Table 1) (Marega).
|
Year |
Authors |
Patient (n) |
Sex |
Age |
Level |
Trauma |
|
1959 |
Marega |
1 |
Male |
41 |
C5-C6 |
No |
|
1977 |
Durig&Zdrojewski et al |
1 |
Female |
52 |
C5-C6 |
Yes |
|
1982 |
Roda& Gonzalez et al |
1 |
Male |
43 |
C6-C7 |
No |
|
1984 |
de Barros & de Barros et al |
1 |
Male |
24 |
C3-C4 |
Yes |
|
1985 |
Jomin&Lesoin et al |
1 |
Male |
42 |
C4-C5 |
Yes |
|
1986 |
Eisenberg & Bremer et al |
1 |
Male |
25 |
C5-C6 |
Yes |
|
1986 |
Lechowski&Urbaniak et al |
1 |
Male |
N/A |
C5-C6 |
N/A |
|
1986 |
Vernay&Rampon et al |
1 |
Male |
N/A |
C5-C6 |
N/A |
|
1988 |
Schneider & Grossman et al |
1 |
Female |
50 |
C5-C6 |
No |
|
1988 |
Parnell |
1 |
Male |
47 |
C5-C6 |
No |
|
1989 |
Lee & Cheng et al |
1 |
Female |
53 |
C6-C7 |
No |
|
1989 |
Destee&Lesoin et al |
1 |
Male |
31 |
C6-C7 |
No |
|
1990 |
Epstein &Syrquin |
1 |
Female |
38 |
C6-C7 |
No |
|
1991 |
Sprick&Fergers et al |
1 |
Female |
49 |
C6-C7 |
Yes |
|
1994 |
Ozer &Ozek et al |
1 |
Female |
36 |
C5-C6 |
Yes |
|
1995 |
Allut&Zabala et al |
1 |
N/A |
N/A |
C4-C5 |
N/A |
|
1998 |
Mihara& Ohnari et al |
1 |
Male |
N/A |
C6-C7 |
N/A |
|
2000 |
Clatterbuck& Belzberg et al |
3 |
Male |
40 |
C4-C5 |
No |
|
|
|
|
Male |
32 |
C5-C6 |
No |
|
|
|
|
Female |
52 |
C3-C4 |
No |
|
2000 |
Borm&Bohnstedt et al |
1 |
Male |
40 |
C5-C6 |
Yes |
|
2001 |
Iwamura |
1 |
Male |
45 |
C6-C7 |
No |
|
2001 |
Yang &Leng et al |
3 |
Female |
45 |
C5-C6 |
No |
|
|
|
|
Male |
39 |
C5-C6 |
No |
|
|
|
|
Male |
60 |
C5-C6 |
No |
|
2007 |
Neroni&Gazzeri et al |
1 |
Female |
52 |
C6-C7 |
No |
|
2009 |
Jie&Lijun et al |
2 |
Female |
50 |
C6-C7 |
No |
|
|
|
|
Female |
58 |
C4-C5 |
No |
|
2010 |
Hsieh & Wu et al |
1 |
Female |
61 |
C3-C4 |
No |
|
2011 |
Pan & Li et al |
2 |
Female |
50 |
C6-C7 |
No |
|
|
|
|
Female |
58 |
C4-C5 |
No |
|
2014 |
Warade&Misra |
1 |
Male |
64 |
C6-C7 |
No |
|
N/A indicates not available, Table extrapolated from Pan et al with addition of recently reported cases |
||||||
at C2/3 severely compressing the spinal cord (Figure 2),
Figure 2: A sagital T2 image of the cervical spine demonstrating near complete occlusion of the spinal canal by C2/3 disc hernination with associated myelomalecia of the spinal cord.
and the patient was taken to the operating room for emergent decompression. A posterior decompression from C2-C4 was initially performed, followed by a corpectomy of C3, placement of an interbody cage, and anterior spinal fusion from C2-C4 (Figure 3).
Figure 3: Demonstrates intra-operative fluoroscopic lateral cervical spine radiograph of the posterior decompression of C2-4 and C3 corpectomy with cage placement and anterior spinal fusion from C2-4.
Intraoperatively, a disc herniation was seen penetrating the posterior longitudinal ligament and the ventral dura. The disc was excised revealing contusions on the ventral spinal cord (Figure 4).
Figure 4: Demonstrates C2/3 intra-dural disc removed at the time of C3 corpectomy.
The dural defect was repaired with Dura Matrix? (Stryker, Kalamzoo, MI) in an on lay fashion, and fibrin sealant was placed between the on lay graft and the interbody cage. Post-operatively the patient failed to make any significant neurologic recovery. He was discharged to an acute rehabilitation facility four weeks after surgery and remained ventilator dependent. At one year follow-up, significant neurological improvements were seen - the patient was no longer ventilator dependent, and had regained 4/5 strength in all myotomes of the right upper extremity and the ability to adduct the right hip. He was using a motorized wheelchair but was unable to stand or ambulate as his left upper and lower extremities remained flaccid. Unfortunately he was lost to follow up thereafter and further progress is unknown.
DISCUSSION
High cervical disc herniations present a diagnostic challenge as radiculopathy above C3/4 is poorly understood and is somewhat rare [4]. In order to differentiate high cervical disc herniation, CVA, and carotid artery dissection, the clinician must be familiar with the presenting signs and symptoms differentiating these various pathologies.
CVA is far more common than either high cervical disc herniation or carotid artery dissection. The Center for Disease Control and National Institute of Neurologic Disorders and Stroke has done a tremendous job informing the public of the common presenting symptoms of stroke using the F.A.S.T. (face, arm, speech, time) acronym [5]. Rathore et al., evaluated hospitalized stroke patients from the Atherosclerosis Risk in Communities (ARIC) Study in order to describe the characteristics of incident stroke in a population-based study [6], paresis was the most common symptom, seen in just over 80% of cases, with upper extremity involvement being most common (75%), followed by lower extremity (68%) and face (55%) involvement respectively [6]. The next most common presenting signs were speech deficit (24%), followed by visual field disturbances (hemianopia 14% and diplopia 5%) [6]. Sensory deficits were also observed most often in the upper extremities (38%), followed by the lower extremities (34%), and face (20%), respectively. It is important to keep in mind that the location of ischemia or hemorrhage will have an impact on the specific presenting signs and symptoms during a cerebral vascular accident.
Carotid artery dissection is defined as an intimal tear in the vascular wall. As a result, the vessel can become occluded, develop a thrombus (which can lead to distal emboli), form an aneurysm, or rupture and hemorrhage [7]. The most common location for carotid artery dissection is at the level of C1/2 and the mean age of patients is 47 years [7,8]. Although carotid artery dissection is a rare occurrence, it is noted to be the causative factor of CVA in up to 10% of adults younger than age 50, and up to 80% are preceded by a traumatic event [9]. The average time from traumatic event to presentation is 2-3 days [10]. The presenting signs and symptoms can often mimic less morbid pathologies such as migraine headache or benign musculoskeletal pain. Non-contrast head CT is typically ordered to evaluate a new onset headache, but will often miss a dissection [7]. Historically, angiography was the only way to diagnose carotid artery dissection but given its invasive nature CTA and MRA are now favored. Levy et al showed that MRA is more sensitive in the diagnosis of carotid dissection than vertebral artery dissection [11]. Elijovich compared the ability of CTA and MRA to diagnosis a dissection and they found CTA was only marginally more effective [12,13]. In a review article for dissections of brain supplying arteries, Caplan suggested exclusive use of MRA and only advocated CTA when MR was non diagnostic [14]. However, Vertinsky et al., found MRA may be less sensitive at detecting pseudo aneurysms and long-segment stenosis when compared to CTA [13]. They also noted that CTA visualized more common features of cervical artery dissection but MRA provided complementary or confirmatory information in patients when both tests were performed [13]. More recently, Provenzale et al., compared the sensitivity and specificity of MRA and CTA against the gold standard, angiography, for detecting vertebral and carotid artery dissections - they found both modalities offered similar results at detecting vascular injuries [15].
A presenting triad of signs that should raise the physician’s suspicion of carotid artery dissection is headache, ipsilateral oculosympathetic paresis (partial Horner’s syndrome), and contralateral CVA symptoms - hemiparesis, hemisensory loss, monocular vision loss, hemineglect and/or gaze deviation [8]. A partial Horner’s syndrome can be seen in up to a third of patients with a dissection [16], while contralateral CVA symptoms affect only 8% of patients [7,8]. Dysgeusia (distortion in sense of taste) is only present in approximately 7% of patients but can be very specific for dissection [8]. The location of pain in a dissection is also important to note as it normally occurs over the anterolateral aspect of the neck and radiates to the jaw or ear [7]. These distinguishing signs should not be ignored during the evaluation of a patient presenting with headache, neck pain, and CVA symptoms.
High cervical disc herniations can present with confounding symptoms due to the general lack of radicular symptoms in the upper extremities. Chen et al., presented the largest case series to date on high cervical disc herniations [4]. They concluded ascending dysesthesia of the upper limbs, patch regions of perioral hypoesthesia, faint myelopathic findings, positive Lhermmite’s sign, and/or a history of recent trauma should lead the clinician to consider a high cervical disc herniation as the possible etiology [4]. Kotil et al., reviewed 5 cases of C2/C3 disc herniation and found the most predominate symptoms for high cervical disc herniation may be cruciate paralysis and perioral numbness [17]. They noted that patients with symptomatic C2/C3 disc herniations presented with non-focal symptoms - dizziness, tinnitus, headache and suboccipital pain rather than middle or lower axial neck pain [17]. Nishizawa et al., three patients with high cervical disc herniation all initially had sensory disturbances in the upper extremities that eventually progressed to manual dexterity and gait abnormalities [18].
High cervical disc herniations most commonly present with sensory changes involving either the perioral region and/or the upper extremities. Sensory changes in the perioral region are secondary to involvement of the descending tracts of the fibers or cell bodies of the trigeminal nerve, which originate in the pons and medulla and travel down to the approximately the C4 segment [19]. Other possible presenting symptoms include occipital headache, loss of fine motor control in the upper extremities, cruciate paralysis (upper extremity paralysis with relatively normal lower extremity function), or BrownSequard syndrome [2,4,20]. Because the most cephalad portion of the spinal canal has a large cross sectional diameter, disc herniations at this level are less likely to become symptomatic when compared to more caudal levels. However, symptomatic herniations in the upper cervical spine are more likely to cause myelopathy as opposed to radiculopathy due to the typically large and central nature of the disc herniation [17]. Because the cardio respiratory centers of the spinal cord are located from C3 to C5, it is imperative to diagnose high cervical disc herniations in a timely manner, as permanent deficits in this region can be devastating. A proposed algorithm is presented (Figure 1) to aid clinicians in the diagnosis of patients with symptoms suspicious for CVA but with confounding symptoms.
CONCLUSION
CVA and carotid artery dissection are far more common entities than high cervical disc herniation. High cervical disc herniation should be suspected when patients present with perioral numbness, cruciate paralysis, headache, progressive limb paresis, loss of fine motor control in the upper extremities, or Brown-Sequard syndrome. MRA of the cervical spine can differentiate between high cervical disc herniation and carotid artery dissection and may aid in a more timely diagnosis. Cases of symptomatic high cervical disc herniation would likely benefit from urgent surgical decompression, however further research on this topic is needed.
REFERENCES
- Bucciero A, Vizioli L, Cerillo A. Soft Cervical Disc Herniation. An analysis of 187 cases. J Neurosurg Sci. 1998; 42:125-130.
- Antich PA, Sanjuan AC, Girvent FM, Simó JD. High cervical disc herniation and Brown-Sequard syndrome. A case report and review of the literature. J Bone Joint Surg Br. 1999; 81: 462-463.
- Sayer FT, Vitali AM, Paquette S, Honey CR. Isolated C3-C4 disc herniations present as a painless myelopathy. Spine J. 2008; 8: 729-731.
- Chen TY. The clinical presentation of uppermost cervical disc protrusion. Spine. 2000; 25: 439-442.
- National Institute of Neurological Disorders and Stroke. Brain Basics: Preventing Stroke. Updated June 22, 2015.
- Rathore SS, Hinn AR, Cooper LS, Tyroler HA, Rosamond WD. Characterization of incident stroke signs and symptoms: findings from the atherosclerosis risk in communities study. Stroke. 2002; 33: 2718-2721.
- Peterson A. Focus On: Headache and Neck Pain - When to Suspect Cervical Artery Dissection.
- Shea K, Stahmer S. Carotid and vertebral arterial dissections in the emergency department. Emerg Med Pract. 2012; 14:1-23.
- Stahmer SA, Raps EC, Mines DI. Carotid and vertebral artery dissections. Emerg Med Clin North Am. 1997; 15: 677-698.
- Biousse V, D'Anglejan-Chatillon J, Touboul PJ, Amarenco P, Bousser MG. Time course of symptoms in extracranial carotid artery dissections. A series of 80 patients. Stroke. 1995; 26: 235-239.
- Levy C, Laissy JP, Raveau V, Amarenco P, Servois V, Bousser MG, et al. Carotid and vertebral artery dissections: three-dimensional time-of-flight MR angiography and MR imaging verus conventional angiography. Radiology. 1994; 190: 97-103.
- Elijovich L, Kazmi K, Gauvrit JY, Law M. The emerging role of multidetector row CT angiography in the diagnosis of cervical arterial dissection: preliminary study. Neuroradiology. 2006; 48: 606-612.
- Vertinsky AT, Schwartz NE, Fischbein NJ, Rosenberg J, Albers GW, Zaharchuk G. Comparison of multidetector CT angiography and MR imaging of cervical artery dissection. AJNR Am J Neuroradiol. 2008; 29: 1753-1760.
- Caplan LR. Dissections of brain-supplying arteries. Nat Clin Pract Neurol. 2008; 4: 34-42.
- Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR Angiography, and CT Angiography in the diagnosis of carotid and vertebral artery dissection: A review of the medical literature. AJR Am J Roentgenol. 2009; 193: 1167-1174.
- Dziewas R, Konrad C, Dräger B, Evers S, Besselmann M, Lüdemann P, et al. Cervical artery dissection--clinical features, risk factors, therapy and outcome in 126 patients. J Neurol. 2003; 250: 1179-1184.
- Kotil K, Sengoz A. The management in the C2-C3 disc herniations: a clinical study. Turk Neurosurg. 2011; 21: 15-21.
- Nishizawa S, Yokoyama T, Yokota N, Kaneko M. High cervical disc lesions in elderly patients--presentation and surgical approach. Acta Neurochir (Wien). 1999; 141:119-126.
- Scheinder RC, Crosby EC, Russo RH, Gosch HH. Traumatic spinal cord syndromes and management. Clin Neurosurg. 1973; 20: 424-492.
- Sayer FT, Vitali AM, Low HL, Paquette S, Honey CR. Brown-Sèquard syndrome produced by C3-C4 cervical disc herniation: a case report and review of the literature. Spine. 2008; 33: 279-282.