Early Laparoscopy in the Management of Acute Non Specific Abdominal Pain: Is It Mandatory?
- 1. Department of General Surgery, Mansoura University, Egypt
- 2. Department of Gynecology and Obstetrics, Mansoura University, Egypt
Abstract
Introduction: Acute non specific abdominal pain (NSAP) is one of the most frequent indications of surgical admission. The assessment of those patients includes observation, or early laparoscopy. Observation can lead to definitive diagnosis however; complications such as peritonitis, hemorrhage, or female infertility may be linked to this method. Early laparoscopy (EL) has a higher rate of clinical diagnosis but surgical exploration can results in a considerable rate of negative exploration. The aim of this study is to evaluate the role of EL in the management of NSAP.
Patient and method: Fifty patients with NSAP were randomly distributed using closed envelops method to early laparoscopy group I, or observation group II after informed consent was obtained. Group I 24 patients was treated by early laparoscopic exploration within 12 to 24 hours of admission, while 26 patients in Group II were treated by observation frequent clinical evaluation, more investigation until definitive diagnosis.
Results: The female sex was prodominnent 75%, and 73% in group I & II respectively, and the mean age considered young 24.7 (range 18 to 49 years) versus 24.3 ( range 18 to 50 years) There was no any statistically significant values at the time of admission in the terms of age, sex, BMI, WBCs counts, and temperature in the studied groups. EL group I has a High statistical significant and P value was less than 0.001 in getting a definitive diagnosis, similar statistically significant results in the term of shorter hospital stay, and readmission rate, with a lower morbidity rate has been recorded.
Conclusion: Active observation alone is not sufficient to get a definite diagnosis, early laparoscopy is superior investigatory and therapeutic tool which must be integrated and scheduled in a time manner or scheduled protocol during admission to improve diagnostic accuracy, shorten hospital stay and decrease morbidity rate.
Keywords
Non specific abdominal pain; Laparoscopy; Observation wait and see; Acute abdomen
Citation
Abbas A, Borham W, El Ghadban H, Abdelatif ME, Samir M, et al. (2017) Early Laparoscopy in the Management of Acute Non Specific Abdominal Pain: Is It Mandatory? Ann Emerg Surg 2(5): 1023.
INTRODUCTION
Nonspecific Acute Abdominal Pain (NSAP) can be defined as acute abdominal pain for less than 7 days, while diagnosis is still uncertain instead of baseline examination and diagnostic tests [1]. NSAP is considered a significant problem in surgery and represents at least 13% to 40% of emergency surgical admissions for acute abdominal pain [2]. For the assessment of those patients different strategies have been used, including observation, and Early Laparoscopy (EL) [3]. Observation option or what is called “wait and see” by hospitalizing the patient and performing frequent examinations can lead to definite diagnosis with a predictive value of 68-92% for this method [4].
On the other hand, a “wait-and-see” policy could result in high morbidity and complication rates by delayed management [5]. Complications such as peritonitis, hemorrhage, or infertility may be linked to this method [6].
In addition 51% of patients undergoing policy of “wait-andsee” will be operated on [7], however surgical exploration on patients whose diagnosis is still doubtful can result in a high rate of negatives exploration [5].
With the modern era of video laparoscopy started in the 1980s, and by the development of the computer chip television [8]. Patients with NSAP could be managed by Early laparoscopy EL [9], laparoscopy is one of the safest and most accurate method to obtain liver biopsy [10], it is also used as a second look procedure or cancer staging, the usefulness and reliability of laparoscopy in the detection of advanced inoperable disease is also reported [11]. Patients with NSAP could be managed by EL or active observation, the decision is largely debated in the literature [9]. In this clinical randomized study we try to detect the role of early laparoscopy in the management of NSAP.
PATIENT AND METHOD
In this prospective randomized study, all cases of acute nonspecific abdominal pain admitted to our surgical department Mansoura Emergency Hospital were eligible to participate after taken an informed written consent and after exhaustion of all non-invasive baseline diagnostic methods to reach a definite diagnosis, patients were randomly assigned to early laparoscopy group (EL) or group I or to clinical observation group (OBS) or group II using closed envelop method.
Inclusion criteria
Adult above 18 years old have NSAP, hemodynamically stable, have no signs of sepsis or septic shock, accepted coagulation profile, fit for general anesthesia, and not known to have chronic liver disease or malignancy.
Exclusion criteria
Patients below 18 years old, or diagnosed after base line investigation, those who had clear signs of sepsis, or hemodynamically unstable. Patients diagnosed as chronic disease, decompensated liver disease, or malignancy, those with uncorrected coagulopathies, or had contraindication to general anaesthia, or pneumoperitoneum, and lastly those with uncontrolled severe psychological disorder or refusing to participate in the study.
Patient sample
selection During the period of January 2015 to June 2017 including at least 3 months of follow up, we had 563 cases of acute abdominal pain admitted to surgical ward for assessment, diagnosis was established in 432 cases (76%) after baseline clinical examination and investigations including routine laboratory work up, X ray chest and abdomen, and abdominal U.S. Eighty one patients were excluded due to variable causes, the remaining 50 cases were randomly distributed to either one of the studied groups using closed envelop method, group I patients underwent (EL) within 12 to 24 hours of admission, and group II subjected to wait and see protocol (OBS).
Group I Diagnostic and therapeutic laparoscopy
Under general anaesthia, pneumoperitonium was inducted maintaining the pressure between 12 to 14 mm Hg, and through a 10 mm umblical port camera was introduced and further ports were introduced according to surgeon’s need and pathology detected. After inspecting the port entry the whole abdomen was inspected changing table position, or introducing more port(s) whenever needed to full visualization of the abdomen’s four quadrants and detect any possible pathology. The surgical procedure was completed according to diagnosis and intraoperative finding.
Group II: Observation group
After being admitted to the surgical ward, all the patients were followed up through: detailed history taken, complete clinical examination that was repeated twice a day, baseline hematologic tests were repeated at 24 and 48 hours from admission, complementary hematologic and/or radiologic investigations were performed on the basis of patient’s clinical evaluation. Whenever a clinical diagnosis could be defined, the appropriate medical or surgical treatment was immediately undertaken.
In the presence of persistent or worsening pain or if signs of sepsis appears, surgical exploration either by a laparoscopic procedure or open technique was undertaken even in the absence of a diagnosis. On the other hand, two criteria for discharge were needed to dismissed undiagnosed patients first one was clinical improvement with asymptomatic patient (pain disappears and no local abdominal signs or systemic signs of sepsis) with second criteria was normal laboratory tests.
Follow-up visits and clinical examinations were scheduled 1 week after discharge and then at 3, 6, 9, and 12 months. All cases were followed up for at least 6 months post discharge after period of hospitalization, either through clinic visit or active phone questionnaire and reassessment if needed. All data were collected and recorded in a special sheet form and entered the computer for statistical analysis using SPSS program system versions 17.
RESULTS
Fifty patients were enrolled in this study after being fulfilled the inclusion criteria and agree to participate in the study after getting a written informed consent. A total of 50 eligible patients were randomized to either early laparoscopy (24 patients) or active clinical observation (26 patients).
There was no any statistically significant value at the time of admission in the terms of age, sex, BMI, WBCs counts, and temperature in the studied groups. The majority of cases were female 75%, and 73% in group I & II respectively, and the mean age considered young 24.7 (range 18 to 49 years) versus 24.3 ( range 18 to 50 years) See Table (1).
Table 1: Characteristic of Patients with NSAP Included in the Study.
|
|
LAP Group |
OBS Group |
P value |
|
|
24 |
26 |
|
|
No. of patients |
6/18 (75%) |
7/19 (73%) |
0.85 |
|
Male/ female ratio |
24.7 ± (7.45)
|
24.3 ± (6.14)
|
0.88 |
|
Age (year)
|
23.1 ± 5
|
22.5 ± 3
|
0.5 |
|
BMI (kg/m 2 )
|
36.9 ± 0.5 |
36.8 ± 0.6 |
0.4 |
|
Temperature (°C) |
8200 ± 1850
|
8730 ± 1600
|
0.3 |
|
WBC
|
All patients in the two groups underwent abdominal ultrasound, plain abdominal and chest radiography. More complex and specific radiological investigation were used in OBS group as intravenous I.V urography, abdominal CT and MRI with high statistical significant (p value less than 0.003) see Table (2).
Table 2: Radiological investigations and referral.
|
|
LAP Group |
OBS Group |
P value |
|
Intravenous urography |
0 |
3 |
0.0003
|
|
Abdominal magnetic resonance |
0 |
1 |
|
|
Abdominal CT |
0 |
4 |
|
|
Gynecological referral |
2 |
7 |
Twenty four patients underwent laparoscopy 12 to 24 hours after hospital admission (mean = 17.5 hours). Mean operative time was 60.1 ± 18.6 minutes (range 30–120 minutes). A clinical macroscopic diagnosis was possible in 21 patients (87.5%) see Table (3).
Table 3: Final Diagnosis after 48 hours in the studied Groups with sex distribution.
|
|
Group I Early Laparoscopy |
Group II Observation |
|||
|
Male 6/24 (25%) |
Female 18/24 (75%) |
Male 7/26 (27%) |
Female 19/26 (73%) |
||
|
Definitive diagnosis
Total |
5/6 |
16/18 |
4/7 |
10/19 |
|
|
21/24 (87.5%) |
14/26 (54%) P value 0.01 |
||||
|
Acute appendicitis |
2 (8.3%) |
5 (20.83%) |
2 (7.7%) |
2 (7.7%) |
|
|
Adhesions |
0 (0%) |
1 (4.1%) |
0 (0%) |
0 (0%) |
|
|
Torsion in peritoneal fold |
0 (0%) |
1 (4.1%) |
0 (0%) |
0 (0%) |
|
|
Cholecystitis |
0 (0%) |
1 (4.1%) |
0 (0%) |
0 (0%) |
|
|
Constipation |
0 (0%) |
0 (0%) |
1 (3.8%) |
0 (0%) |
|
|
Diverticulitis |
1 (4.1%) |
1 (4.1%) |
0 (0%) |
1 (3.8%) |
|
|
Peritonitis |
1 (4.1%) |
3 (12.5%) |
1 (3.8%) |
2 (7.7%) |
|
|
Pancreatitis |
1 (4.1%) |
0 (0%) |
0 (0%) |
2 (7.7%) |
|
|
Inflammatory Bowel disease |
0 (0%) |
0 (0%) |
0 (0%) |
1 (3.8%) |
|
|
PID salpingitis |
NO |
1 (4.1%) |
NO |
1 (3.8%) |
|
|
Ovarian Cyst |
NO |
2 (8.3%) |
NO |
1 (3.8%) |
|
|
Ectopic Pregnancy |
NO |
1 (4.1%) |
NO |
0 (0%) |
|
|
Undiagnosed cases Total |
1 (4.1%) |
2 (8.3%) |
3 (11.5%) |
9 (34.6%) |
|
|
3/24 (12.5%) |
12/26 (46%) P value 0.01 |
||||
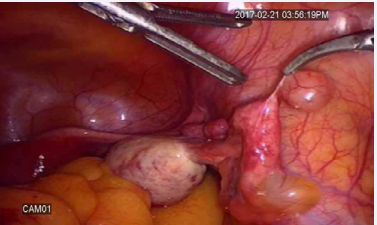
Laparoscopic appendectomy was done for eleven patients, and after histological examination was performed revealing a pathologic appendix in 7 cases (29.2%), four cases were free (16.7%), one case was diagnosed as pelvic inflammatory disease PID (4.1%), one case acute cholecystitis was detected, another single case with adhesive band (4.1%), one more interesting rare case with interaoperative diagnosis of parietal peritoneal gangernous pedunclated small fatty fold see Figure (1),
Figure 1: Pedunclated parietal peritoneal gangernous small fatty fold
one case was ectopic pregnancy, one case was early pancreatitis, and four cases thin rim of turbid fluid (pus) was noted in whom the clinical history of aggressive antibiotics were documented, and in whom two cases diagnosed as sealed perforated duodenal small ulcers, one pyosalpinx was detected and one suppurative appendicitis was suspected but not proved by histopathological evaluation ( this case referred to gynecologist and treated as salpingitis later without further complication), two cases were ovarian cyst with one had paraovarian multiple clear cysts see Figure (2),
Figure 2: Paraovarian multiple clear cysts.
and two cases were diagnosed as diverticulitis in diagnosed as the following: two cases were dismissed with a diagnosis of PID, two case were diagnosed as endometriosis (7.7%) , one case (3.8%) was developed a picture sub acute adhesive intestinal obstruction and improved with conservative management and gastrograffin follow through, four cases (15.4%) were readmitted early in the next few days after being discharged based on criteria of discharge as a consequence of recurrent abdominal pain and they underwent a delayed laparoscopic procedure . Lastly three cases (11.5%) discharged undiagnosed, unfortunately they still complain of bouts of abdominal pain until nowadays see Table (4).
Table 4: Early follow up of non diagnosed cases in observation group
|
|
NO (%) |
|
Subacute adhesive intestinal obstruction |
1 (3.8%) |
|
PID |
2 (7.7%) |
|
Endometriosis |
2 (7.7%) |
|
Readmission and Laparoscopy
|
4 (15.4%)
2 (7.7%) 1 (3.85) 1 (3.8%) |
|
Undiagnosed cases |
3 (11.5) |
|
Total |
12 (46%) |
Hospital stay was significantly higher in observation group II (4.7 ±2.4 days) versus (3.7 ± 0.8 days) in EL group I, also, three month recurrence of pain was significantly more in observation group II see Table (5).
Table 5: Hospital stay, and readmission in the studied groups.
| LAP Group | OBS Group | P value | |
| Hospital stay (days) Range | 3.7 ± 0.8 2–5.5 | 4.7 ± 2.4 2–11 | 0.004 |
| Analgesic therapy (days) Range | 1.3 ± 0.7 1–4 | 1.2 ± 1.0 0–5 | 0.6 |
| Number of Mortality Morbidity Readmission | 0 2 (8.3%) 0 | 0 3 (11.5%) 4/26 (15.4%) | 0.18 0.05 |
| Three month recurrence (%) | 1/24 (4.1 %) | 12/26 (42.2%) | 0.001 |
Group I (EL) showed no mortality, and morbidity was limited to two cases: one case (3.1%) urinary tract infection and another one of trocar site infection. Group II observation group (OBS) had no mortality, but there were a significant morbidity by delayed diagnosis in three cases (11.5%) who developed signs and symptoms of sepsis, also, abdominal pain persisted in 12 of 26 patients (46%) with a high significant differences between the studied two groups. Readmission was significantly higher in OBS group, and delayed laparoscopy was needed in 15.4%. In addition three patients 11.5% never diagnosed and still suffering of abdominal pain see Table (5).
DISCUSSION
Acute non specific abdominal pain is one of the most frequent indications of admission to emergency beds; the estimated prevalence of NSAP from the population varies from 42 to 69% [12]. NSAP is still the main differential diagnostic problem in the emergency [13]. In this study the prevalence was about 24% from all surgical admission for acute abdominal pain; other series suggested the prevalence between 13% to 40% of acute abdominal pain [2]. The majority of cases of NSAP are female up to two third and they usually young in child bearing period with average age of 26 years [14], these finding are similar in the two studied groups. Different strategies to assess those patients have been used, including observation, imaging methods, and early laparoscopy (EL) [3]. Observation protocols management including repeated clinical examination, radiological investigation, and a gynecologic opinion carry the risk of delayed surgical intervention and may increase morbidity or prolong the hospital stay. In addition, a definitive clinical diagnosis can’t be reached in a good percentage of patients, who leaved the hospital unsatisfied after a prolonged stay [15].In some series percentage of unreached diagnosis was about 40% in the active observation group [3,16]. Suggestions like structured questionnaires and diagnostic programs on computers may increase proportion of correct diagnoses, although these programs are still unpopular [2].
In this study the percentage of failure to reach definite diagnosis was similar to other reports reaching up to 46% after using different clinical or radiological modalities within 48 hours of admission. More time loss and delay is needed in those patient to get definitive diagnosis with more hospital cost, and more risk to get a complication which sometimes difficult to be documented like developed adhesion or affect fertility especially in females [6]. We believe that, standardization of observation time is urgently needed; there is no defined time for observation, which considered as the main value of hospital stay and varied from 2 days [16] to 7.3 days [5].
On contrary, most of reports denoting a higher rate of clinical diagnosis achieved by EL when compared with active observation [16,17], EL performs better in establishing a final diagnosis, with rates ranging from 79.2 to 96.9% for EL vs. 28.1% to 78.1% compared with OBS [18]. The reports described complication rates to be higher in the active observation group compared to that found in the early laparoscopy group [2,5,16].
One recent study focusing on role of EL and confirm the superiority of EL in the matter of getting definitive diagnosis reaching efficacy of 85% [14], another study suggesting much more accuracy reaching more than 95% [19], this study confirm the high accuracy level of diagnosis by EL.
Few reports included both sex in the study design, female pathology as PID, ovarian cysts or endometriosis presenting about 31.2% of total diagnosed cases [20], but it didn’t reach 16% in another study [14], in this work gynecological diagnosis in EL group was five cases 21%, and two cases only 7.7% in observation group II in the diagnosed cases which raising up to seven cases 27% after full observation and exploration.
Some reports also, consider a higher rate of readmission in OBS group [5,16]. This study easily confirms all these reports about EL in the terms of early established diagnosis less complication rate, and less percentage of readmission. Instead of these facts, levels of comparison didn’t reach significant statistical values in many reports in the terms of complication rates or readmission, but still statistically significant in establishing early diagnosis, and short hospital stay [1,2,5,17], it could be suggested that observation method is less efficient way to get a definite diagnosis, and it had a considerable risk for getting more complications or morbidities, and this leads to prolongation of hospital stay, or a higher incidence of readmission.
Furthermore, the baseline radiological examinations is a matter of contra verse, a study did not include abdominal ultrasound [20], on contrary, CT has become the primary imaging technique for the evaluation of a confused clinical picture in the patient with acute abdominal pain in other center [18]. Thermography, peritoneal cytology, and more recently spiral computer tomography had been suggested by others [21]. However, none of these techniques seems to have been determinant in improving the clinical management of NSAP [2]. A recent study suggest the physicians’ pre-CT diagnostic confidence as the only significant factor in diagnosis of ANSAP, omitting or denied other factors as patient’s age, sex, physicians’ years of experience; and physicians’ pre-CT admission decision [22].
An understanding of the benefits and limitations of different radiologic techniques is needed to avoids multiple procedures and for the usage of appropriate investigation for the patient and estimate the cost- effectiveness [18].
We think that the additional cost of these investigations, the longer hospital stay, beside the risk of delayed diagnosis, can guide us for getting attention to the active observation period, and the beneficial time of admission during which definitive diagnosis should be reached depending upon using the ideal investigatory tool during this period to decrease the cost, lessen the morbidities, and shorten the hospital stay, otherwise to establish EL as a good solution after failure of reaching definite diagnosis.
The need of a time scheduled protocol of admission, non invasive investigation, and laparoscopy is mandatory, more clinical studies with larger sample size comparing the periods of observation, and the timing of laparoscopy are essential to guide such protocols.
On Conclusion, Active observation alone is not sufficient to get a definitive diagnosis in patients suffering NSAP or to treat those patients, other non invasive investigation must be used during the period of observation within a limited period to lessen the hospital stay, decrease the morbidity rate, and improve the diagnostic accuracy. EL is superior investigatory and therapeutic tool which must be integrated and scheduled in a time manner during admission of patients with ANSAP.
REFERENCES
- Dom?nguez LC, Sanabria A, Vega V, and Osorio C. Early laparoscopy for the evaluation of nonspecific abdominal pain: a critical appraisal of the evidence. Surg Endosc. 2011; 25: 10-18.
- Morino M, Pellegrino L, Castagna E, Farinella E, and Mao P. Acute Non-specific Abdominal Pain: A Randomized Controlled Trial comparing Early Laparoscopy versus Clinical observation. Ann Surg. 2006; 244: 881-888.
- Driffield T, Smith P. A real options approach to watchful waiting: theory and an illustration. Med Decis Making. 2007; 27: 178-188.
- Raheja SK, McDonald P, Taylor I. Non-specific abdominal pain an expensive mystery. J R Soc Med. 1990; 83: 10-11.
- Schietroma M, Cappelli S, Carlei F, Pescosolido A, Lygidakis NJ, Amicucci G. Acute abdomen: early laparoscopy or active laparotomic–laparoscopic observation. Hepatogastroenterology. 2007; 54: 1137-1141.
- Olsen JB, Myrén CJ, Haahr PE. Randomized study of the value of laparoscopy before appendectomy. Br J Surg. 1993; 80: 922-923.
- Gaitan H, Angel E, Sanchez J, Gomez I, Sanchez L, Agudelo C. Laparoscopic diagnosis of acute lower abdominal pain in women of reproductive age. Int J Gynaecol Obstet. 2002; 76: 149-158.
- Mc Kernan JB, Saye WB.Laparoscopic general surgery. J Med Assoc Ga. 1990; 79: 157-159.
- Gaitán HG, Reveiz L, Farquhar C . Laparoscopy for the management of acute lower abdominal pain in women of childbearing age. Cochrane Database Syst Re. 2011.
- Chen L and Minkes RK: Diagnostic Laparoscopy, Ch 14 In: Jones DB, Wu JS, Soper NJ, eds. Laparoscopic Surgery: Principle And Practice. 2nd ed. Marcel Dekker, Inc. 2006: 121-127.
- Saptarshi B, McDonald K, Gleeson N, Lme F. Laparoscopy as a Diagnostic Tool in the Diagnosis of (Nsap) Nonspecific Abdominal Pain. Internet J Surg. 2006; 8: 21-26.
- Maggio AQ, Reece-Smith AM, Tang TY, Sadat U, Walsh SR. Early laparoscopy versus active observation in acute abdominal pain: systematic review and meta-analysis. Int J Surg. 2008; 6: 400-403.
- Fagerström A, Paajanen P, Saarelainen H, Ahonen-Siirtola M, Ukkonen M, Miettinen P, et al. Non-specific abdominal pain remains as the most common reason for acute abdomen: 26-year retrospective audit in one emergency unit. Scand J Gastroenterol. 2017; 52: 1072-1077.
- Ahmad MM, Dar HM, Waseem M, Wani H, Nazir I, Jeelani A. Role of laparoscopy in nonspecific abdominal pain. Saudi Surg J. 2014; 2: 71-74.
- Onur OE, Guneysel O, Unluer EE, Akoglu H, Cingi A, Onur E, Denizbasi A. ‘‘Outpatient follow-up’’ or ‘‘Active clinical observation’’ in patients with nonspecific abdominal pain in the Emergency Department. A randomized clinical trial. Minerva Chir. 2008; 63: 9-15.
- Decadt B, Sussman L, Lewis MP, Secker A, Cohen L, Rogers C, et al. Randomized clinical trial of early laparoscopy in the management of acute non-specific abdominal pain. Br J Surg. 1999; 86: 1383-1386.
- Champault G, Rizk N, Lauroy J, et al. Right iliac fosse in women: conventional diagnostic approach versus primary laparoscopy. A controlled study (65 cases). Ann Chir. 1993; 47: 316-319.
- Gupta H, Dupuy DE. Advances in imaging of the acute abdomen. Surg Clin North Am. 1997; 77: 1245-1263.
- Rubbia A, Faryal GA, Javeria I, and, Roohul M. Role of Diagnostic Laparoscopy in Patients with Acute or Chronic Nonspecific Abdominal Pain; World J of Lap Surg. 2015; 8: 7-12.
- Biswas S, McDonald K, Gleeson N, and Falke L. Is NSAP A Myth In Today's World? Laparoscopy As A Diagnostic Tool In The Diagnosis Of (Nsap) Nonspecific Abdominal Pain: A Peripheral County Hospital Experience. The Internet Journal of Surgery. 2005; 8, 2; 1-8.
- Rao PM, Rhea JT, Novelline RA, Mostafavi AA, and Mc Cabe CJ .Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998; 338: 141-146.
- Eisenberg JD, ReisnerAT, BinderWD, Zaheer A, Martin L. GunnML, et al. Role of CT in the Diagnosis of Nonspecific Abdominal Pain: A Multicenter Analysis. AJR Am J Roentgenol. 2017; 208: 570-576.