Efficacy and Safety of 1470 nm Diode Laser Enucleation of the Prostate for Benign Prostatic Hyperplasia: A Systematic Review and Meta-Analysis
- 1. Department of Urology, Yantai Yuhuangding Hospital, Qingdao University, China
- 2. The Second Clinical Medical College, Binzhou Medical University, China
Abstract
Background: Benign prostatic hyperplasia (BPH) is a common urological condition in aging men, often requiring surgical intervention when medical therapy fails. The 1470 nm diode laser enucleation of the prostate (DiLEP) has emerged as a promising technique, but its efficacy and safety remain to be systematically evaluated.
Methods: A systematic literature search was conducted in PubMed, Embase, Web of Science, and Cochrane Library to identify Randomized Controlled Trials (RCTs) investigating 1470 nm DiLEP in the treatment of BPH. Primary outcomes included functional parameters such as International Prostate Symptom Score (IPSS), quality of life (QoL), maximum urinary flow rate (Qmax), and post-void residual urine volume (PVR). Secondary outcomes included intraoperative and perioperative indicators (e.g., operative time, hemoglobin decrease, catheterization duration, bladder irrigation time) and complication rates. Effect sizes were synthesized using appropriate fixed- or random-effects models based on heterogeneity, and reported as Mean Difference (MD) or Odds Ratios (OR) with 95% Confidence Intervals (CI).
Results: Four RCTs involving 533 patients were included. 1470 nm DiLEP was associated with significantly shorter operative time (MD = -24.43, P < 0.0001), reduced hemoglobin loss (MD = -2.77, P = 0.02), shorter bladder irrigation time (MD = -13.23, P < 0.0001), and reduced catheterization duration (MD = -2.29, P < 0.0001). Functional outcomes such as IPSS, QoL, and Qmax were comparable between groups, but DiLEP showed superior reduction in PVR at 6 and 12 months. No significant differences in complication rates were observed.
Conclusion: The 1470 nm DiLEP appears to be a safe and effective surgical option for BPH, with advantages in perioperative outcomes and potential mid-term functional benefits, particularly in improving bladder emptying. Further large-scale, long-term RCTs are needed to confirm these findings.
Keywords
• Benign Prostatic Hyperplasia
• Diode Laser
• Meta-Analysis
• Randomized Controlled Trial
Citation
Guo Y, Sun F, Zhang Y, Wang B, Liu C, et al. (2025) Efficacy and Safety of 1470 nm Diode Laser Enucleation of the Prostate for Benign Pros tatic Hyperplasia: A Systematic Review and Meta-Analysis. Ann Emerg Surg 9(1): 1040.
INTRODUCTION
Benign prostatic hyperplasia (BPH) is a prevalent non cancerous condition among aging men, characterized by progressive enlargement of the prostate gland [1,2]. This condition often results in lower urinary tract symptoms (LUTS), including urinary frequency, urgency, nocturia, and weak stream, which can significantly impair patients’ quality of life [3,4]. For individuals with moderate-to severe symptoms who fail to respond adequately to pharmacological therapy, surgical intervention remains the standard treatment. In recent years, diode laser enucleation of the prostate has emerged as a minimally invasive and technologically advanced surgical approach for BPH [5]. Among the various diode laser wavelengths, the 1470 nm laser has gained particular attention due to its unique biophysical properties. This wavelength offers high absorption in both water and hemoglobin, enabling precise tissue dissection and superior hemostasis during enucleation [6-8]. These advantages translate into potential clinical benefits such as reduced intraoperative bleeding, shorter catheterization time, and faster recovery, making 1470 nm diode laser enucleation of the prostate (1470 DiLEP) an increasingly adopted technique in urologic surgery [9,10]. Although several randomized controlled trials (RCTs) have evaluated the clinical outcomes of 1470 DiLEP, the results remain heterogeneous, and a comprehensive synthesis of the evidence is lacking. This meta-analysis aims to critically evaluate the efficacy and safety of 1470 nm DiLEP in the treatment of BPH, based on current evidence from RCTs. By analyzing perioperative parameters, postoperative symptom relief, and complication rates, this study seeks to provide robust clinical evidence to support the use of 1470 DiLEP as an effective surgical option for patients with BPH.
METHODS
The review protocol was registered with PROSPERO CRD420251056180 following the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Search strategy
We conducted a comprehensive literature search in the PubMed, Embase, Web of Science, and Cochrane Library databases, following the PRISMA guidelines. The search included studies published from database inception up to April 2025. Our strategy was developed based on the PICOS framework (Population, Intervention, Comparator, Outcomes, Study design). The primary search terms included “diode laser”, “enucleation”, and “prostate”. Two independent reviewers performed the database searches using a predefined strategy, and their results were cross checked for consistency. Disagreements regarding study selection were resolved through consultation with a third reviewer. Furthermore, reference lists of relevant articles were manually screened to identify additional eligible studies.
Inclusion criteria and data extraction
Studies were included based on the following criteria: (1) Population: Male patients diagnosed with BPH and indicated for surgical treatment; (2) Intervention: 1470nm DiLEP; (3) Comparator: Any other established surgical technique for prostate enucleation, including but not limited to transurethral resection of the prostate (TURP), holmium laser enucleation (HoLEP), thulium laser enucleation (ThuLEP), bipolar enucleation of the prostate (BEEP), 980 nm DiLEP, and open prostatectomy; (4) Outcomes: Studies that reported at least one of the following—operative time, hemoglobin loss, catheterization time, bladder irrigation time, IPSS, QoL score, Qmax, PVR, or complication rates; (5) Study design: Randomized controlled trials (RCTs). We excluded non randomized studies, retrospective or observational designs, animal studies, case reports, reviews, conference abstracts, and studies with inappropriate comparators.
Quality assessment
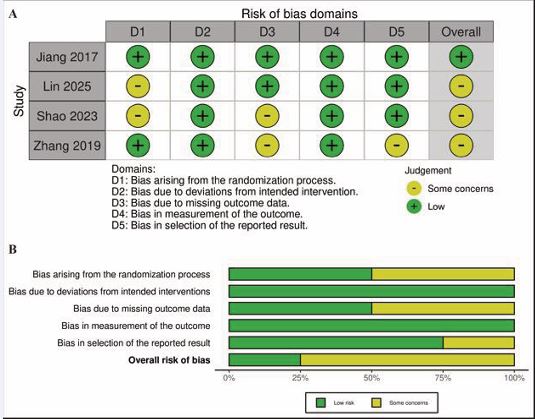
Two reviewers independently assessed the risk of bias of the included RCTs using the Cochrane Risk of Bias 2.0 tool. The evaluation focused on five domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Discrepancies between reviewers were resolved through discussion with a third investigator. Each domain was rated as having “low risk,” “some concerns,” or “high risk” of bias. The overall risk of bias for each study was determined by the highest level of risk found in any domain.
Data extraction and outcome measures
Two authors independently extracted relevant data from the selected studies, including first author, year of publication, country, sample size, surgical techniques used, follow-up duration, perioperative indicators, functional outcomes, and adverse events. The primary outcomes assessed were postoperative functional outcomes, including the International Prostate Symptom Score (IPSS), Quality of Life (QoL) score, maximum urinary flow rate (Qmax), and postvoid residual urine volume (PVR). These parameters reflect the efficacy of 1470 nm DiLEP in improving urinary symptoms and functional recovery in patients with BPH. The secondary outcomes included perioperative parameters such as operative time, hemoglobin loss, catheterization duration, and bladder irrigation time, as well as complication rates (e.g., bleeding, capsule perforation, urinary incontinence, urethral stricture). These outcomes were used to evaluate the surgical safety and procedural efficiency of 1470 nm DiLEP compared with other surgical modalities.
Statistical analyses
Statistical analysis was performed using Review Manager version 5.3 (The Cochrane Collaboration). For continuous variables, mean difference (MD) with 95% confidence interval (CI) was calculated; for dichotomous outcomes, odds ratios (OR) with 95% CI were used. Heterogeneity among studies was assessed using Cochran’s Q test and the I² statistic. Significant heterogeneity was defined as I² > 50% or p < 0.05. A fixed-effects model was used when heterogeneity was low; otherwise, a random effects model was applied. P-value of less than 0.05 was considered statistically significant.
RESULTS
Characteristics of included studies
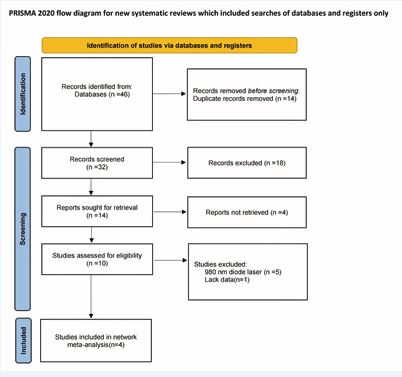
A total of 46 articles were initially identified through our systematic search. After screening titles and abstracts, 18 studies were excluded. Of the 10 full-text articles assessed for eligibility, 5 articles were excluded for not meeting the predefined inclusion criteria, and 1 additional study was removed due to insufficient or incomplete outcome data. Consequently, 4 randomized controlled trials [11-14], were included in the final analysis to evaluate the efficacy and safety of 1470 nm diode laser enucleation of the prostate for BPH. The study selection process is illustrated in Figure 1, and the detailed characteristics of the included studies are summarized in Table 1.
Figure 1 PRISMA flow diagram.
Table 1: Characteristics of included studies.
|
Study(years) |
Treatment |
Age(year) |
Patients |
IPSS baseline |
Qmax baseline |
QoL data |
PVR (ml) |
Prostate volume(ml) |
Laser power |
Postoperative follow-up period |
|
Jiang2017 |
DilEP |
71.5±9.4 |
90 |
23.4±6.6 |
7.8±2.1 |
5.1±0.7 |
57.3±36.8 |
70.3±8.7 |
NA |
1 and 3 months |
|
|
PKRP |
70.3±8.7 |
90 |
22.1±6.3 |
7.5±2.0 |
5.2±0.9 |
65.2±42.7 |
54.9±23.5 |
160W |
|
|
Lin 2025 |
DilEP |
69.2±8.7 |
41 |
24.5±3.7 |
5.2±3.5 |
4.9±0.7 |
115.6±117.9 |
75.1±35.8 |
150W |
12 months |
|
|
PKRP |
70.7±7.5 |
40 |
23.4±2.8 |
4.7±2.9 |
4.7±0.6 |
104.8±110.2 |
72.8±22.4 |
280W |
|
|
Shao2023 |
DilEP |
77.6?±3.6 |
60 |
25.3±3.0 |
6.5±1.3 |
4.9±0.8 |
221.5±80.1 |
71.8±23.0 |
150W |
3 and 6 months |
|
|
PKRP |
77.3±3.2 |
60 |
25.1±2.5 |
6.5±1.4 |
4.9±0.8 |
217.5±83.1 |
71.5±24.1 |
280W |
|
|
Zhang 2019 |
DilEP |
73.7±8.4 |
76 |
24.5±3.2 |
5.7±2.2 |
4.7±0.7 |
204.6±191.1 |
56.2±11.9 |
120W |
3,6, and 12 months |
|
|
PKRP |
71.5±8.9 |
76 |
25.2±3.0 |
6.2±2.5 |
4.9±0.7 |
199.5±186.8 |
55.5±13.1 |
180W |
Risk of bias
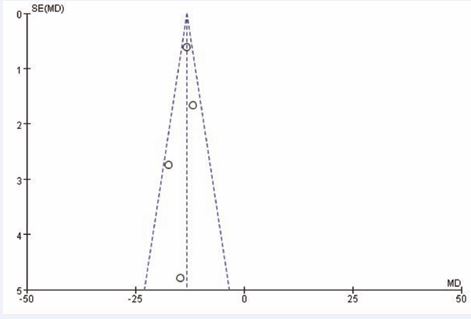
The risk of bias assessment for each study is summarized in Figure 2. Among the four included randomized controlled trials, three were judged to have some concerns, while the remaining one is considered to have a low risk of bias. The most frequent sources of potential bias were related to the randomization process and the selection of reported outcomes. The funnel plot (Figure 3), showed a relatively symmetrical distribution, suggesting a low likelihood of publication bias among the studies evaluating the efficacy and safety of 1470 nm DiLEP.
Figure 2 The assessment of risk of bias (RoB). (A) Risk of bias domain for each included study; (B) Summary of risk of bias assessment.
Figure 3 Funnel plot of the articles.
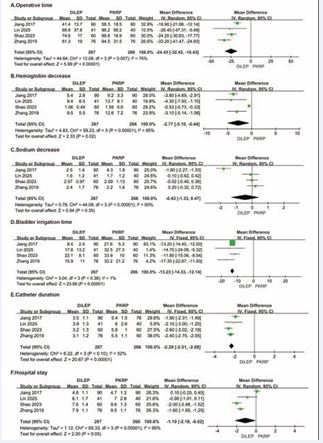
time, and catheterization duration (MD = −24.43, 95% CI (−32.42–−16.43), P < 0.0001; MD = −2.77, 95% CI (−5.10 −0.44), P = 0.02; MD = −13.23, 95% CI (−14.33–−12.14), P < 0.0001; MD = −2.29, 95% CI (−2.51–−2.08), P < 0.0001, respectively; Figure 4).
Figure 4 Forest plots showing the pooled results of operative time, hemoglobin decrease, sodium decrease, bladder irrigation time, catheterization duration and hospital stay between 1470 nm DiLEP and PKRP group. (A) operative time; (B) hemoglobin decrease; (C) sodium decrease; (D) bladder irrigation time; (E) catheterization duration; (F) hospital stay; MD, mean difference; CI, confidence intervals.For serum sodium decrease and hospital stay, no statistically significant differences were observed between the two groups. These findings suggest that 1470 nm DiLEP may offer superior perioperative outcomes, with reduced surgical trauma, faster recovery indicators, and potentially improved patient tolerance compared to PKRP.
Postoperative Outcomes
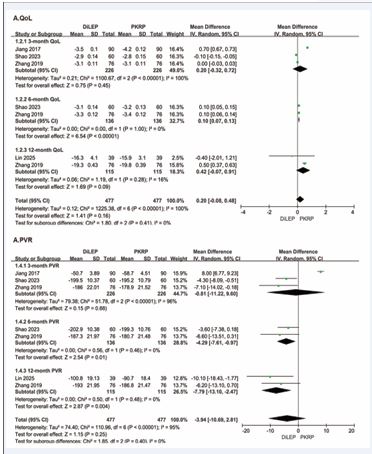
Functional outcomes including symptom scores (IPSS, QoL) and voiding parameters (Qmax, PVR) were reported preoperatively and postoperatively across all included studies. We extracted follow-up data at 3, 6, and 12 months postoperatively for analysis. Overall, no significant differences were observed between groups in most follow-up outcomes (Figures 5 and 6); however, 1470 nm DiLEP was associated with significantly better PVR at both 6 and 12 months (MD = −4.29, 95% CI (−7.61 -−0.97), P = 0.01; MD = −7.79, 95% CI (−13.10–−2.47), P = 0.004, respectively; Figure 6).
Figure 6 Forest plots showing the pooled results of QoL and PVR between 1470 nm DiLEP and PKRP group. (A) QoL; (B) PVR; QoL, Quality of Life; PVR, postvoid residual urine volume.
These results indicate that although both techniques yield comparable functional recovery overall,1470 nm DiLEP may provide additional benefit in mid- and long-term bladder emptying efficiency.
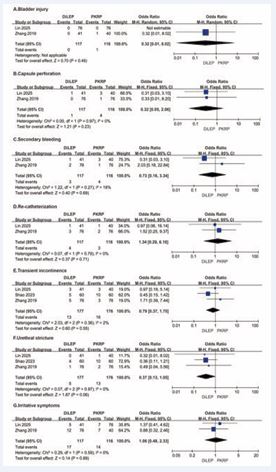
Perioperative Complication
Perioperative complications, including TUR syndrome, bladder injury, capsule perforation, secondary bleeding, re catheterization, transient incontinence, urethral stricture, and irritative symptoms, were documented in all included studies. The pooled results revealed no statistically significant differences between the two procedures in the incidence of any of the assessed complications (Figure 7).
Figure 7 Forest plots showing the pooled results of bladder injury, capsule perforation, secondary bleeding, re-catheterization, transient incontinence, urethral stricture, and irritative symptoms between 1470 nm DiLEP and PKRP group. (A) bladder injury; (B) capsule perforation; (C) secondary bleeding; (D) re-catheterization; (E) transient incontinence; (F) urethral stricture; (G) irritative symptoms.
These findings suggest that 1470 nm DiLEP is comparable to PKRP in terms of perioperative safety, with a similar risk profile for both minor and major adverse events (Supplementary Materials).
DISCUSSION
BPH is a common condition among aging men and often leads to LUTS that impair quality of life [15,16]. For patients with moderate-to-severe symptoms who do not respond well to medical therapy, surgical intervention remains the primary treatment [17,18]. TURP has long been considered the gold standard for treating BPH in men with prostate volumes between 30 and 80 ml [19]. Despite its high clinical success rate, concerns remain regarding perioperative complications, particularly bleeding, which limit its applicability in patients with large prostates or those on anticoagulation therapy [20,21]. To address these limitations, various alternative surgical techniques have been developed. PKRP was introduced as an advancement over monopolar TURP, offering better hemostasis and a reduced risk of TUR syndrome [22]. Nonetheless, PKRP still presents risks of bleeding and prolonged catheterization, particularly in cases involving significantly enlarged prostates [23,24]. Among the newer modalities, DiLEP has gained attention as a promising endoscopic technique due to its precise tissue cutting, effective hemostasis, and favorable safety profile [25]. DiLEP encompasses various diode laser systems categorized by their emission wavelengths, such as 980 nm, 1318 nm, and 1470 nm [26]. It is well recognized that the 1470 nm diode laser stands out because it has the highest absorption in water, which allows it to efficiently vaporize tissue and provide superior coagulation [14]. Due to these physical properties, 1470 nm DiLEP is expected to offer clinical advantages including reduced intraoperative blood loss, shorter catheterization time, and decreased hospitalization duration. Our meta analysis comprehensively evaluated both the efficacy and safety of 1470 nm DiLEP. In terms of perioperative efficacy, 1470 nm DiLEP was associated with significantly shorter operative time, reduced hemoglobin loss, shorter bladder irrigation time, and reduced catheterization duration. These findings suggest that DiLEP may provide a less invasive and faster recovery surgical option without compromising clinical effectiveness. With regard to postoperative functional outcomes, no significant differences were observed between 1470 nm DiLEP and PKRP in most symptom and voiding parameters during follow-up. However, 1470 nm DiLEP showed superior improvement in QoL at 6 months and significantly greater reduction in PVR at both 6 and 12 months. These findings indicate that although the two techniques provide broadly comparable long-term outcomes, 1470 nm DiLEP may offer modest advantages in mid-to-long term symptom relief and voiding efficiency. From a safety perspective, our analysis found no statistically significant differences between the two techniques in perioperative complications including TUR syndrome, bladder injury, capsule perforation, secondary bleeding, re catheterization, transient incontinence, urethral stricture, or irritative symptoms. This highlights the favorable safety profile of 1470 nm DiLEP, comparable to that of PKRP. The potential advantages of DiLEP may be attributed to the specific properties of the 1470 nm wavelength, which has high absorption in both water and hemoglobin, leading to precise ablation and effective hemostasis with minimal collateral damage [27, 28]. In addition to its clinical benefits, 1470 nm DiLEP may also offer economic advantages by reducing operative time, minimizing the need for blood transfusion, shortening catheterization and hospitalization durations, and potentially lowering the overall healthcare burden associated with postoperative complications and recovery time [29]. However, it is important to acknowledge certain limitations. First, all included randomized controlled trials were conducted in Asia, which may limit the generalizability of the results. Second, the follow-up durations varied among studies and did not exceed one year, restricting our ability to evaluate long-term outcomes. Third, there is a lack of direct comparisons regarding the learning curves and cost-effectiveness between 1470 nm DiLEP and PKRP. Fourth, heterogeneity may exist due to variations in laser types, energy settings, surgeon experience, and outcome assessment methods across studies. Although we applied a random-effects model to account for this variability, it may still affect the stability of the results. Additionally, the small number of included studies (only four) limited our ability to conduct sensitivity analyses or subgroup analyses to assess potential biases.
Figure 5 Forest plots showing the pooled results of IPSS and Qmax between 1470 nm DiLEP and PKRP group. (A) IPSS; (B) Qmax; IPSS, International Prostate Symptom Score; Qmax, maximum urinary flow rate
CONCLUSION
In conclusion, 1470 nm DiLEP demonstrates comparable safety and at least equivalent, if not superior, efficacy to PKRP in the treatment of BPH. It offers specific advantages in perioperative parameters and mid-term functional outcomes, suggesting it may be a valuable surgical option for appropriately selected patients. Future large-scale, high-quality randomized trials with long-term follow-up are warranted to confirm these findings and optimize patient selection.
DATA AVAILABILITY STATEMENT
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
AUTHOR CONTRIBUTIONS
Jitao Wu and Xiaohong Ma designed the research, edited and revised the paper. Yicheng Guo, Fengze Sun and Lin Wang performed the data extraction. Chu Liu, Yanwei Zhang and Yicheng Guo carried out the meta-analysis. Yicheng Guo and Bin Wang drafted the paper. All of the authors approved the submitted and final versions.
FUNDING
This work was supported by the National Natural Science Foundation of China (Nos. 82370690, 82303813) and Natural Science Foundation of Shandong Province (Nos. ZR2023MH241, ZR2023QH271, ZR2021MH185).
REFERENCES
- Bosch RJ. Pathogenesis of benign prostatic hyperplasia. Eur Urol. 1991; 1: 27-30.
- Chughtai B, Forde JC, Thomas DD, Laor L, Hossack T, Woo HH, et al. Benign prostatic hyperplasia. Nat Rev Dis Primers. 2016; 2: 16031.
- Jønler M, Riehmann M, Bruskewitz RC. Benign prostatic hyperplasia. Current pharmacological treatment. Drugs. 1994; 47: 66-81.
- Rosen RC, Giuliano F, Carson CC. Sexual dysfunction and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH). Eur Urol. 2005; 47: 824-837.
- Kuntz RM. Current role of lasers in the treatment of benign prostatichyperplasia (BPH). Eur Urol. 2006; 49: 961-969.
- Do?owy ?, Krajewski W, Dembowski J, Zdrojowy R, Ko?odziej A. The role of lasers in modern urology. Cent European J Urol. 2015; 68: 175- 182.
- Elzayat EA, Elhilali MM. Holmium laser enucleation of the prostate (HoLEP): long-term results, reoperation rate, and possible impact of the learning curve. Eur Urol. 2007; 52: 1465-1471.
- Yin L, Teng J, Huang CJ, Zhang X, Xu D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J Endourol. 2013; 27: 604-611.
- Erol A, Cam K, Tekin A, Memik O, Coban S, Ozer Y. High power diode laser vaporization of the prostate: preliminary results for benign prostatic hyperplasia. J Urol. 2009; 182: 1078-1082.
- Xu A, Zou Y, Li B, Liu C, Zheng S, Li H, et al. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. J Endourol. 2013; 27: 1254-1260.
- Jiang D, Liao G, Ma H, Yang X, Pang J. A randomized controlled trial comparing 1470nm diode laser vs. plasmakinetic enucleation of the prostate for treating benign prostatic hyperplasia. Eur Urol. 2022; 81: S1302.
- Lin D, Luo C, Cui K, Xu H, Yuan H, Luan Y, et al. 1470 nm diode laser enucleation versus bipolar transurethral resection of the prostate for the surgical management of benign prostatic hyperplasia: a randomized comparison. Lasers Med Sci. 2025; 40: 226.
- Shao D, Zang Z, Li Z, Zhang H, Sun D, Diao T, et al. Efficacy and Safetyof 1470 nm Diode Laser Enucleation of the Prostate in Elderly BenignProstatic Hyperplasia Patients. J Endourol. 2023; 37: 700-705.
- Zhang J, Wang X, Zhang Y, Shi C, Tu M, Shi G. 1470 nm Diode Laser Enucleation vs Plasmakinetic Resection of the Prostate for Benign Prostatic Hyperplasia: A Randomized Study. J Endourol. 2019; 33: 211-217.
- Barry M, Roehrborn C. Management of benign prostatic hyperplasia. Annu Rev Med. 1997; 48: 177-189.
- Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016; 13: 108-119.
- Boyle P, McGinn R, Maisonneuve P, La Vecchia C. Epidemiology of benign prostatic hyperplasia: present knowledge and studies needed. Eur Urol. 1991; 20: 3-10.
- Parsons JK, Kashefi C. Physical activity, benign prostatic hyperplasia,and lower urinary tract symptoms. Eur Urol. 2008; 53: 1228-1235.
- Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006; 50: 969-979;
- Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS, et al. Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline. J Urol. 2018; 200: 612-619.
- Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008; 180: 246-249.
- Erturhan S, Erbagci A, Seckiner I, Yagci F, Ustun A. Plasmakinetic resection of the prostate versus standard transurethral resection of the prostate: a prospective randomized trial with 1-year follow-up. Prostate Cancer Prostatic Dis. 2007; 10: 97-100.
- Bhansali M, Patankar S, Dobhada S, Khaladkar S. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. J Endourol. 2009; 23: 141-145.
- Dincel C, Samli MM, Guler C, Demirbas M, Karalar M. Plasma kinetic vaporization of the prostate: clinical evaluation of a new technique. J Endourol. 2004; 18: 293-298.
- Seitz M, Bayer T, Ruszat R, Tilki D, Bachmann A, Gratzke C, et al. Preliminary evaluation of a novel side-fire diode laser emitting light at 940 nm, for the potential treatment of benign prostatic hyperplasia: ex-vivo and in-vivo investigations. BJU Int. 2009; 103:770-775.
- Wezel F, Wendt-Nordahl G, Huck N, Bach T, Weiss C, Michel MS, et al. New alternatives for laser vaporization of the prostate: experimental evaluation of a 980-, 1,318- and 1,470-nm diode laser device. World J Urol. 2010; 28: 181-186.
- Dincel C, Samli MM, Guler C, Demirbas M, Karalar M. Plasma kinetic vaporization of the prostate: clinical evaluation of a new technique. J Endourol. 2004; 18: 293-298.
- Seitz M, Bayer T, Ruszat R, Tilki D, Bachmann A, Gratzke C, et al. Preliminary evaluation of a novel side-fire diode laser emitting light at 940 nm, for the potential treatment of benign prostatic hyperplasia: ex-vivo and in-vivo investigations. BJU Int. 2009; 103:770-775.
- Wezel F, Wendt-Nordahl G, Huck N, Bach T, Weiss C, Michel MS, et al. New alternatives for laser vaporization of the prostate: experimental evaluation of a 980-, 1,318- and 1,470-nm diode laser device. World J Urol. 2010; 28: 181-186.