Laparoscopic Reduction of a Left Paraduodenal Hernia Associated with Kidney Atrophy in a Pediatric Patient
- 1. Department of General Surgery, Carle Foundation Hospital, USA
- 2. Department of Pediatric Surgery, Carle Foundation Hospital, USA
Abstract
Bowel obstruction is a common cause of surgical admission and operation. Uncommonly, this can be caused by a congenital defect in the fusion of the peritoneum and mesocolon called a paraduodenal hernia. These internal hernias range in presentation from asymptomatic incarceration to complete bowel obstruction. Most patients present at middle age and require surgery even if they are asymptomatic at the time. Laparoscopy is a relatively new modality for intervention, but is feasible. In this case, a 15-year-old patient presented with subacute bowel obstruction due to a left-sided paraduodenal hernia associated with an atrophic left kidney.
Keywords
Bowel obstruction, Internal hernia, Laparoscopy, Paraduodenal hernia
Citation
Rawson N, Dominguez K (2020) Laparoscopic Reduction of a Left Paraduodenal Hernia Associated with Kidney Atrophy in a Pediatric Patient. Ann Emerg Surg 5(1): 1033.
INTRODUCTION
The most common form of congenital internal hernia is a leftsided paraduodenal hernia through the fossa of Landzert. This causes a spectrum of symptoms ranging from asymptomatic to high grade bowel obstruction. Derangement of the intraabdominal structures does not appear to be common, but seems possible. Surgery is typically mandated and can be completed laparoscopically or through an open technique.
CASE PRESENTATION
A 15-year-old male arrived with complaints of 1-week of intermittent left lower quadrant abdominal pain, nausea, and non-bilious vomiting. He described a history of constipation that he usually managed with over the counter laxatives and fiber. Computed tomography (CT) was completed and demonstrated a majority of his small bowel was contained inside of a spherical structure in his left upper quadrant suspected to be an internal hernia, as well as an atrophic left kidney (Figure 1).

Figure 1: Axial view CT scan demonstrating the intestinal vasculature entering into a left sided paraduodenal hernia (A) and a coronal view of a well-defined bowel containing sac (B).
There was a clear caliber change as dilated bowel entered the hernia and decompressed bowel exited it. He was subsequently taken to the operating room for laparoscopic reduction.
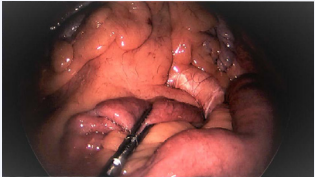
The procedure was initiated with open placement of an infraumbilical 10 mm port and survey of the abdomen. The hernia sac was immediately visible without clear entry or exit of bowel. Two 5 mm ports were then placed in the right lower quadrant as working ports. An unsuccessful attempt was made to enter the hernia sac bluntly over the duodenum. Instead, the defect was identified (Figure 2) by running the distal bowl from the cecum proximally. A third right lower quadrant port was required for retraction and better triangulation of the tissue of interest. Nearly two-thirds of the small bowel was reduced from the hernia sac.
Figure 2: Intraoperative images of the distal bowel protruding from the fossa of Landzert (arrow).
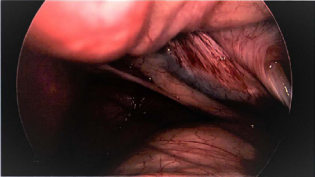
Once resistance was met, the hernia sac was visualized with the camera to ensure no further contents required evacuation (Figure 3).
Figure 3: The empty hernia sac after all contents had been removed.
The defect was then closed primarily.
Post-operatively, the patient remained nil per os until postoperative day 1. He had minimal pain and his diet was able to be rapidly advanced. He had return of bowel function and was discharged on post-operative day 2.
DISCUSSION
Paraduodenal hernia is the most common type of congenital internal hernia, but accounts for just under 0.5% of all intestinal obstructions [1]. Two forms exist based on laterality. The left paraduodenal hernia accounts for the majority of cases and is thought to occur due to abnormal rotation of the midgut causing failure of the descending mesocolon to fuse with the peritoneum [2]. This failure of fusion creates the fossa of Landzert which is bounded posteriorly by the retroperitoneum, medially by the duodenum, laterally by the mesocolon, and anteriorly by the inferior mesenteric vein. On the right, a similar problem occurs, but instead herniation occurs into the fossa of Kolb.
Symptoms can range from asymptomatic to complete obstruction. If symptoms develop, they typically present in the 4th and 5th decade of life [3]. It is not usually associated with renal atrophy as in this case, but the hernia has been reported to displace intra-abdominal organs making a mechanical etiology the most likely mechanism of this patient’s left atrophic kidney. Diagnosis is usually made on CT scan by identifying the cluster of small bowel in the left or right upper quadrant.
Regardless of the symptoms, surgery is typically recommended as there is a reported 50% risk of lifetime complications [4]. Laparoscopic cases have been reported, but if bowel compromise is suspected most authors recommend an open approach. The general surgical principles are to reduce the hernia from the fossa of Landzert or Kolb and then close the defect. Some authors suggest sac removal, but this remains controversial due to potential colonic vascular injury. The recurrence after surgery has not been well documented with one review finding only 1 out of 31 patients to have had recurrent hernia and obstruction [5].