Holohemispheric Hemorrhage in Dural Border Cell Layer Disclosed After Evacuation of Infantile Acute Subdural Hematoma
- 1. Department of Neurosurgery, Bethlehem Garden Hospital 3-14-72 Umesono, Japan
- 2. Department of Neurosurgery, Tokyo Metropolitan Tama Medical Center 2-8-29 Musashidai, Japan
Abstract
Background: Acute subdural hematoma in an infant without external signs of head trauma is sometimes thought to be symptomatic of shaken baby syndrome (SBS) in the United States or of infantile acute subdural hematoma (IASDH) due to minor head trauma in Japan.
The present case report aimed to demonstrate that holohemispheric hemorrhage in dural border cell layer (HHDBCL) can be disclosed after evacuation of IASDH.
Case description: A 12-month-old boy was noted by his mother falling backward and striking the occipital region. After crying, he developed convulsion followed by altered consciousness. He was brought to a nearby hospital where head CT revealed acute subdural hematoma on the right side associated with large sylvian fissure on the left side. The patient underwent emergency surgery. Via dural incision, xanthochromic fluid and flesh bloody fluid including several flesh clots were removed. His postoperative course was uncomplicated and revealed good recovery to the level same as the previous condition. Magnetic resonance imaging next day after operation disclosed thin, film-like, high-intensity hemorrhage surrounding the entire cerebral hemisphere (i.e holohemispheric hemorrhage), anatomically corresponding to dural border cell layer. Ophthalmological examination revealed bilateral retinal hemorrhages. His five years follow-up neurological examinations confirmed to have normal developmental milestones.
Discussion & Conclusion: Pathoetiology causing IASDH may be secondary spread of the hemorrhage from DBCL into the subdural compartment. HHDBCL is considered to be unique neuroimaging features that may indicate primary pathoetiology causing IASDH.
IASDH can occur after a short fall, if the dural border cell layer is disrupted in an infant with cranio-cerebral disproportion, including benign enlargement of subarachnoid space and or large sylvian fissure. Neuroimaging findings showing HHDBCL may be useful to make differential diagnosis between IASDH and SBS
KEYWORDS
- Infantile acute subdural hematoma; Short fall; Holohemispheric hemorrhage; Dural border cell layer; Shaken baby syndrome; Benign enlargement of subarachnoid space; Large sylvian fissure
CITATION
Aoki N (2025) Holohemispheric Hemorrhage in Dural Border Cell Layer Disclosed After Evacuation of Infantile Acute Subdural Hematoma. Ann Forensic Res Anal 10(1): 1062.
INTRODUCTION
An acute subdural hematoma (ASDH) accompanied by retinal hemorrhage (RH) is often diagnosed without question worldwide as shaken baby syndrome (SBS) or abusive head trauma (AHT) [1].However, this tendency is based exclusively on the assumption that a short fall is unable to cause ASDH. An American neurosurgeon had insisted previously that SBS be diagnosed automatically on the assumption that a subdural hematoma (SDH) accompanied by a RH invariably indicated SBS [2]. Since then, this automatic diagnosis has gained traction in the English-speaking world, where the presence of a subdural fluid collection on computed tomography (CT) or magnetic resonance imaging (MRI) leads straightway to the diagnosis of SBS or AHD unless pathological findings indicate differently.
On the other hand, because infantile ASDH (IASDH) cases have been reported to date mostly in Japan [3-8], and rarely occur outside the home, the accidents resulting in the trauma are seldom witnessed by a third party [9]. The present case report demonstrates that IASDH can occur if the dural border cell layer (DBCL) is disrupted in an infant with cranio-cerebral disproportion (CCD), including benign enlargement of subarachnoid space (BESS) and large sylvian fissure LSF).
CASE PRESENTATION
This 12-month-old boy without significant medical history was noted by his mother falling backward and striking the occipital region against a floor at home living room. After crying, he developed generalized tonic convulsion followed by altered consciousness.
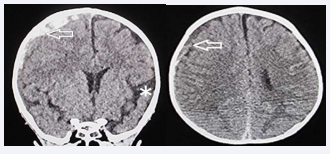
The patient was brought to a nearby hospital where signs of altered consciousness status was confirmed, prompting to undergo head CT (Figure 1).
Figure 1: Computed tomography on arrival. Left (Coronal View), Right (Axial View). Acute subdural hematoma with mixed density on the right side (arrows).
Large sylvian fissure on the left side (asterisk), contralateral to the subdural hematoma
Based on the CT findings showing ASDH on the right side associated with LSF on the left side, the neurosurgen decided to undergo emergency surgery.
Under general anesthesia, dural incision after burr- hole craniotomy encountered gushed xanthochromic fluid followed by flesh bloody fluid including several clots. Subdural irrigation with saline solution was not encountered by ongoing bleeding. After insertion of subdural drainage catheter, uneventful wound closure was achieved.
His postoperative course was uncomplicated and revealed good recovery to the level same as the previous condition.
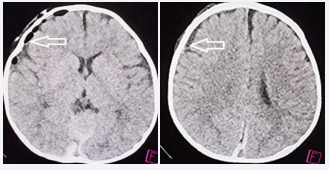
Post-operative CT showed decreased volume of acute subdural hematoma without brain swelling (Figure 2).
Figure 2: Computed tomography Post-op on the day.
Left & Right (Axial View): Decreased volume of acute subdural hematoma on the right side. (arrows)
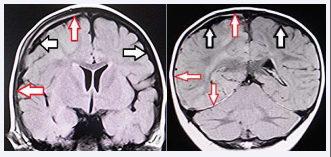
Magnetic resonance imaging (MRI) next day after operation disclosed thin, film-like, high-intensity hemorrhage surrounding the entire cerebral hemisphere (i.e holohemispheric hemorrhage), anatomically corresponding to dural border cell layer (Figure 3).
Figure 3 Magnetic resonance imaging (fluid-attenuated inversion recovery, axial view) next day after operation.
Left & Right: Coronal View Thin, film-like, high-intensity hemorrhage surrounding the entire cerebral hemisphere (i.e holohemispheric hemorrhage), anatomically corresponding to dural border cell layer on the right side. (red arrows) Large subarachnoid space indicating benign enlargement of subarachnoid space. (black arrows).
No primary cerebral parenchymal abnormality is observed.
No primary cerebral parenchymal abnormality was observed. On the day after surgery, ophthalmological examination revealed bilateral retinal hemorrhage more on the right side.
His five years follow-up neurological examinations confirmed to have normal developmental milestones.
DISCUSSION
As noted earlier, the immaturity of the cerebrospinal fluid (CSF) dynamics induce age-regulated accumulation of CSF in the subarachnoid space (SAS) [10,11]. This phenomenon is commonly observed in infants between the ages of 6 and 10 months and also occurs in some patients with BESS [10]. In this age population, development of IASDH is most often [3,6], and is considered to be secondary to CCD including BESS and LSF [6,7]. As the pathoetiology, infants with CCD may be complicated by fluid collection including hemorrhage from venous plexus in DBCL [10,11].
Based on the biophysiological characteristics of infants, IASDH was originally defined in 1984 as an acute, infantile subdural hematoma apparently caused by minor head trauma without loss of consciousness and not associated with a primary brain injury [3]. Most cases of IASDH are also associated with RH [3,4,6]. IASDH is clinically graded as mild (grade I), intermediate (grade II) or fulminant (grade III) in accordance with the findings of a previous study (Table 1) [3].
Table 1 Clinical grade on arrival in patients with infantile acute subdural hematoma, proposed in1984 (Ref.3)
|
Disease |
Type |
Clinical features |
|
grade |
||
|
I |
Mild |
Conscious, no motor disturbance but with vomiting &/or irritability |
|
II |
Intermediate |
Drowsy, minimal or mild hemiparesis |
|
III |
Fulminant |
Stuporous to comatose, moderate to severe hemiparesis, with signs of cerebral herniation |
The present case is invaluable because it demonstrates that intermediate type-IASDH can gain excellent outcome via emergency surgery because of absence of primary cerebral parenchymal injury [12,13].
A subdural collection may be described succinctly as an accumulation of fluid or blood within the dural border cell layer, which are very susceptible to disruption [10]. The MRI findings in the present case of a thin, film-like, high- intensity hemorrhage surrounding the entire cerebral hemisphere (i.e., the holohemisphere) presumably corresponded to the hemorrhage in the DBCL [12-15].
Particularly relevant here is thin-film like appearance seen after evacuation of ASDH may indicate hemorrhage localized in the DBCL. Based on the serial neuroimaging analysis, pathoetiology causing IASDH may be secondary spread of the hemorrhage from the DBCL into the subdural compartment [12]. Thus, some cases with IASDH may occur secondary to hemorrhage in DBCL without primary bridging vein rupture. Because the DBCL is easily disrupted, a hemorrhage originating in the inner dural plexus may be chiefly responsible for the non-traumatic situation or mild head impact [10].
Thin-film like appearance seen after evacuation of ASDH presumably shows hemorrhage localized in DBCL. The presence of HHDBCL in IASDH may make differential diagnosis from SBS/AHT, though requiring further discussion in future. In the present case, the intermediate- type IASDH located at inner part of the holohemispheric hemorrhage may indicate the secondary spread of the hemorrhage from the DBCL into the subdural compartment.
CONCLUSION
Pathoetiology causing IASDH may be secondary spread of the hemorrhage from DBCL into the subdural compartment. Holohemispheric hemorrhage in the DBCL is considered to be unique neuroimaging features that may indicate pathoetiology causing IASDH and in addition may be useful to make differential diagnosis between IASDH and SBS/AHT.
AUTHOR CONTRIBUTION
Nobuhiko Aoki (corresponding author with no coauthors) conceived the study, conducted a search of the literature, and drafted the original manuscript. The author has reviewed the manuscript draft, revised it critically for intellectual content, and approved the final version for submission.
DECLARATIONS, ETHICS APPROVAL, AND CONSENT TO PARTICIPATE
This article was approved by the ethics committee of Bethlehem Garden Hospital and Tokyo Metropolitan Tama Medical Center. No funding was obtained for this study. The parents/legal guardians of the patient provided their consent to publish the details of this case.
CONSENT TO PUBLISH
The author consents to the publication of all identifiable details, which may include photographs, case history, and other details.
REFERENCES
- Wittschieber B, Karger D, Pfeifer H, Understanding Subdural Collections in Pediatric Abusive Head Trauma. AJNR AmJ Neuroradiol. 2019; 40: 388-395.
- Rekate HL Subdural hematomas in infants. (Letter) J Neurosurg. 1985; 61: 316-317.
- Aoki N, Masuzawa H, Infantile acute subdural hematoma. Clinical analysis of 26 cases. J Neurosurg. 1984; 61: 273-2807.
- Aoki N, Clinical and neuroimaging characteristics in mild-type infantile acute subdural hematoma. Report of four cases. Childs Nerv Syst. 2003; 40: 189-195.
- 5. Aoki N, “Infantile” acute subdural hematoma: a clinical entity different from abusive head trauma. J Pediatr Neurol Neurosci. 2020; 4: 151-153.
- Aoki N, Infantile acute subdural hematoma. Clinical and neuroimaging analysis of 15 cases focusing on intracranial structural vulnerabilities. J Sur. 2024; 9: 11104.
- Aoki N, Asymptomatic infantile acute subdural hematoma with benign enlargement of the subarachnoid space and large sylvian fissure. Mega J Case Rep. 2024; 7: 2001-2006.
- Aoki N. Infantile acute subdural hematoma: Caused by abuse or mild head trauma? Nervous System in Children. 2011; 36: 326-330.
- Aoki N, Infantile acute subdural hematoma with retinal hemorrhage caused by minor occipital impact witnessed by an ICU nurse: a case report. Pediatr Neurol Neurosci. 2020; 4: 47-50.
- Mack J, Squier W, Eastman JT, Anatomy and development of the meninges: implications for subdural collections and CSF circulation. Pediatr Radiol. 2009; 391: 200-210.
- Nabeshima S, Reese TS, Landis DM, Brightman MW, Junctions in the meninges and marginal glia. J Comp Neurol. 1975; 164: 127-169.
- Aoki N, Fulminant-type Infantile acute subdural hematoma: Pre- and Post-operative Neuroimaging Analysis. Int J Clin Case Rep Rev. 2024; 20: 01-05.
- Aoki N, Holohemispheric Hemorrhage in Infantile Acute Subdural Hematoma: Serial Neuroimaging Analysis. J Neuroscience and Neurological Surgery. 2024; 14; 01-05.
- Aoki N, Mild-type infantile acute subdural hematoma presenting with a holohemispheric subdural hematoma. Ame J Surg Clin Case Rep. 2024; 8: 1-5
- Aoki N, Holohemispheric Subdural Hematoma: Infantile Acute Subdural Hematoma Localized in the Dural Border Cell Layer. Ann Case Report. 2024; 9: 1959.