Preoperative Optimisation in Enhanced Recovery after Surgery (ERAS) Programs for Total Hip and Knee Arthroplasty: A Systematic Review
- 1. St George and Sutherland Clinical School, University of New South Wales, Australia
- 2. Centre for Pain IMPACT, Neuroscience Research Australia (NeuRA), Australia
- 3. St. George and Sutherland Centre for Clinical Orthopaedic Research (SCORe), Australia
- 4. South Western Sydney Clinical School, University of New South Wales, Australia
- 5. Ingham Institute for Applied Medical Research, Australia
ABSTRACT
Background: Enhanced recovery after surgery (ERAS) programs aim to reduce peri- and post-operative complications by targeting modifiable risk factors through pre-operative and peri-operative interventions. The evidence for ERAS in reducing complications following total hip (THA) and knee arthroplasty (TKA) is mixed. This systematic review aimed to describe pre-operative optimisation protocols for THA and TKA and report their effects on post-operative morbidity and patient-reported outcome measures (PROMs).
Methods: This systematic review was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. Databases were searched for studies with pre-operative optimisation components in ERAS protocols, and data on interventions, frequency, duration, and outcomes (readmissions, complications, PROMs) were extracted. Meta-analysis was not performed due to study heterogeneity.
Results: Thirty-eight studies were included. Common interventions included patient education and physiotherapy. There are nine studies offering medical optimisation such as diabetes or weight loss management. Most studies only involved a single clinic visit and lacked clear targets. ERAS protocols led to a decrease in hospital readmissions in six studies (median -1.8%) and an increase in five (median 0.3%) compared to pre-ERAS protocols. Nine studies reported a decrease in post-operative complications (median 5.0%), while four showed an increase (median 1.9%).
Conclusion: The review found that pre-operative optimisation protocols within ERAS are poorly designed, with low-quality interventions and limited attention to intervention frequency and duration. Consequently, it remains unclear whether pre-operative optimisation affects readmissions, complications, or PROMs. Future research should focus on prospective studies addressing risk factors like obesity and diabetes to improve patient outcomes.
Trial registration: The systematic review protocol was submitted to the International Prospective Register of Systematic Reviews (CRD42021274156).
KEYWORDS
• Total Hip Arthroplasty
• Total Knee Arthroplasty
• Eras
• Pre-Operative Optimisation
• Systematic Review
CITATION
Liu V, Lin JY, Chang WJ, Naylor J, Jenkin D, et al. (2025) Preoperative Optimisation in Enhanced Recovery after Surgery (ERAS) Programs for Total Hip and Knee Arthroplasty: A Systematic Review. Ann Musc Disord 6(1): 1015.
INTRODUCTION
The prevalence of hip and knee osteoarthritis is increasing worldwide [1]. Globally, hip and knee osteoarthritis was ranked as the 11th highest contributor to global disability and 38th highest in disability-adjusted life years [2]. Osteoarthritis affects approximately 9.3% of the Australian population, causing pain and disability, restricting employment and hobbies, and reducing quality of life [3]. Increasing rates of obesity and an ageing Australian population are driving an increase in prevalence from an estimated 2.1 million in 2015 to an estimated 3.1 million (12% of the population) by 2030 [3]. Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are recommended for end-stage osteoarthritis when all appropriate conservative options, delivered for a reasonable period of time, have failed [4]. Arthroplasty is the most cost-effective and clinically effective treatment for end-stage osteoarthritis in appropriately selected individuals [5,6].
THA and TKA are major surgical procedures associated with post-operative medical and surgical complications. These include, but are not limited to, peri-prosthetic joint infection, peri-prosthetic fracture, osteolysis with implant loosening, and venous thromboembolism (VTE). These complications are associated with significant morbidity and mortality, necessitating hospital readmission, medical treatment and/or revision surgery [7-9]. There are known modifiable risk factors which increase the risk of post-operative complications, including body mass index (BMI) ≥ 30, malnutrition, poor glycaemic control, anaemia, smoking, use of opioids and vitamin D deficiency [10- 13]. In addition, poor patient-reported outcomes are also associated with modifiable physiological and psychological factors such as catastrophising, anxiety, depression, and poor self-efficacy [14,15].
In an effort to improve peri-operative outcomes and reduce morbidity, Enhanced Recovery After Surgery (ERAS), a peri-operative care pathway initially developed in the field of colorectal surgery, was adapted for patients undergoing hip and knee arthroplasty [16]. According to ERAS principles, recovery is facilitated by a multimodal approach directed towards global modulation of the surgical stress response [17]. This is achieved through pre-operative patient preparation, standardised anaesthetic regimens intraoperatively, and early mobilisation post-operatively [18]. ERAS protocols are designed and implemented by a multidisciplinary team of surgeons, anaesthetists, nursing, and allied health, and have consistently been associated with faster recovery, decreased morbidity and reduced hospital length of stay (LOS) in multiple surgical subspecialties [19]. However, evidence for the effect of ERAS implementation in orthopaedic surgery on surgical outcomes is conflicting. A recent systematic review concluded that ERAS protocols reduce the length of hospital stay after THA and THA, but have minimal to no impact on perioperative morbidity or readmission [20]. A meta-analysis concluded that ERAS reduced post-operative complications and 30-day mortality after arthroplasty, with no effect on hospital readmissions [21].
One explanation for the inconsistency in the literature regarding the benefits of ERAS protocols on morbidity and mortality may be the heterogeneity in the pre-operative management of patients, with no clear consensus on how patients should be optimised before TKA or THA. Emerging evidence supports the optimisation of diabetes control and weight loss, however how best it is achieved is very much in its infancy [22]. Only one randomised trial has shown that pre-operative weight loss via bariatric surgery resulted in fewer complications in people with obesity undergoing TKA [23]. There are no definitive trials proving diet or drug-based weight loss improves outcomes pre-arthroplasty surgery [24]. There is also no high-level evidence demonstrating the efficacy of opioid tapering prior to arthroplasty surgery in chronic opioid users [25].
In light of the current knowledge gaps, it remains unclear what constitutes effective pre-operative optimisation as part of an ERAS protocol for THA and TKA for the purposes of reducing complications and improving patient-reported recovery. This systematic review aimed to: (1) describe the pre-operative optimisation protocols for THA and TKA that are being used worldwide, including information on the type, duration, frequency and goals of interventions; and (2) report the effects of pre-operative optimisation protocols for THA and TKA on post-operative morbidity (including hospital readmission, complications and mortality) and patient reported outcomes.
METHODS
This systematic review was prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Guidelines [26,27]. The PRISMA checklist is provided in Supplementary Table S1. The systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021274156) and uploaded to medRxiv September 2021(doi: https://doi.org/10.1101/2021.09.27.2126418
9).
Eligibility Criteria
Types of Participants: Studies including adults aged 18 or older receiving primary elective THA or TKA surgeries were included. The surgeries could be either unilateral or bilateral and no restriction was placed on sex or race. Studies including participants receiving partial arthroplasties (i.e., uni-compartmental or hemi- arthroplasties) or arthroplasties indicated for fracture, were not included.
Types of Intervention: Eligible studies investigated pre-operative optimisation protocols administered prior to participants receiving a primary elective THA or TKA, with/without a comparative group that received a standard care protocol. No restriction was placed on the duration of pre-operative optimisation protocol. Only studies that had a comparative group were used for aim 2 of this review. To provide a comprehensive review on pre- operative optimisation, all studies investigating ERAS with a pre-operative component were included in the review.
Type of Outcome Measures: The primary outcomes
of this review for assessing aim 2 were: 1) hospital readmissions within 90 days; and 2) any complication including surgical site or other infection, cardiovascular event, VTE, or death. The secondary outcomes included length of hospital stay, and patient-reported pain and function outcomes. Studies were only included if investigating post-operative outcomes. No restriction was placed on when the outcomes were measured in the studies.
Types of Studies: For Aim 1, we included randomised controlled trials (RCTs), non-randomised clinical trials, prospective observational studies, and retrospective studies. For Aim 2, only RCTs or non-randomised clinical trials were to be included in meta-analyses if one was possible. Systematic or literature reviews, case reports or series, or conference abstracts were excluded.
Search Strategy
To identify eligible, published studies, we searched the following electronic databases:
- MEDLINE
- EMBASE
- Cumulative Index to Nursing and Allied Health Literature (CINAHL)
- Cochrane Central Register of Controlled Trials (CENTRAL)
Search strategies were established using medical subject headings (MeSH) and related text words and tailored to each database. A combination of different keywords for THA, TKA and pre-operative optimisation protocols were used to identify relevant studies. The full search terms and search strategy are included in Supplementary Table S2. No restriction was placed on the publication period, but only studies in the English language were included. We searched the reference lists of eligible studies and relevant reviews to include any missed but relevant published studies. Citation searching for forward citation of recent studies and citation alerts (i.e., Google Scholar) on included studies were also be used to identify new studies as they appeared during the review progress. The search strategy was run in October 2021 and again in March 2023, several weeks prior to manuscript drafting, to retrieve and include any relevant studies.
Study Selection
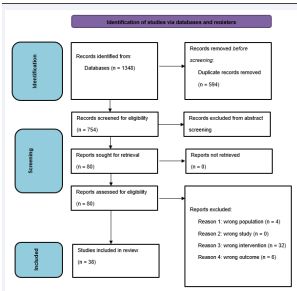
EndNote X9 software (Clarivate Analytics) was used to store, organise, and manage all search results and to remove duplicate records. Two reviewers independently evaluated the title and abstract of all studies identified through the search against the eligibility criteria. The full text of the selected studies was then retrieved. For studies retrieved from trial registrations, the full text was defined as all associated files and information. For any studies with uncertainty about the eligibility, the full text was obtained for further information. Any disagreement over study eligibility was resolved by consensus, and an additional reviewer was consulted if required. The Preferred Reporting Items for Systematic Review and Meta-Analysis Flow Chart with reasons for exclusion is presented in Figure 1.
Figure 1 PRISMA flow diagram outlining the systematic review process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses Reason 1: Is the population adults aged > 18 and received selective THA or TKA (either primary or revision; unilateral or bilateral)? Excluded if: partial or hemireplacement or due to acute fracture Reason 2: Was the study a RCT, non-RCT, prospective observational study or retrospective study? Excluded if: systematic or literature reviews, case reports or series or conference abstracts Reason 3: Did the study investigate an ERAS program prior to participants receiving THA/TKA (with or without a comparative group)? Excluded if: ERAS program commenced after THA/TKA. Reason 4: Is the study primary outcome: hospital readmission within 90 days or complications after THA/TKA? Excluded if: primary outcome is not readmission/complications after THA/TKA
Data Extraction
A customized data extraction spreadsheet was developed and piloted on two studies relevant to this review before it was used to extract data from all the included studies. Two reviewers independently performed data extraction from the final list of selected studies.
Any disagreements in the extracted data were resolved through discussion with a third reviewer. We extracted the following information from the included studies:
- Study characteristics: the first author, year of
publication, study design, country, and study setting.
- Participants: age, sex, type of surgery (i.e., THA or TKA, unilateral or bilateral, left or right), duration of knee/hip osteoarthritis, co-morbidities, use of opioids, and the number of participants allocated in each intervention group.
- Interventions: details of the pre-operative optimisation protocol (i.e., type, duration, number of interventions, frequency, intervention providers, goals of intervention), details of pre-, peri- or post- operative care protocols as a part of a continuum optimisation program if available.
- Outcome measures: the type of measure used to assess primary and secondary outcomes, at any peri- or post-operative timepoints.
- Results: data on the primary and secondary outcomes measured at any timepoints.
- If data were missing, authors of the studies were emailed a maximum of three times, after which the data was considered irretrievable.Study Quality and Risk of Bias
Study Quality and Risk of Bias
Study quality and risk of bias was assessed by two independent reviewers using the Cochrane Risk of Bias version 1 (RoB 1) tool for RCTs [28], and the Cochrane Risk of Bias in Non-Randomised Studies - of Interventions (ROBINS-I) tool for non-randomised studies [29]. Disagreement between reviewers was resolved through discussion and a third reviewer was consulted if consensus was not achieved. The risk of bias was evaluated on the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias. The ROBINS-I tool was used to assess the risk of bias for studies that have not used randomisation for intervention allocations (i.e., cross-sectional or cohort study designs). The ROBINS-I tool covers seven domains: confounding and participants’ selection (pre-intervention), intervention classification (during intervention), and deviations, missing data, measurements and selection of reported results (post-intervention) [29]. Both RoB 1 and ROBINS-I used signalling questions to guide judgments for each domain and an overall risk of bias assessment.
Data Synthesis
A narrative summary was conducted to provide an overview of pre-operative optimisation protocols for THA and TKA respectively. The details of pre-operative optimisation protocols from all selected studies were summarised in Table 1. The risk factors targeted by pre- operative optimisation protocols and the corresponding intervention provided were listed. For aim 2, we planned a meta-analysis, however it was not feasible given the high heterogeneity and high risk of bias of included studies. Thus, a narrative approach was used to summarise the results from non-RCTs and retrospective studies based on study quality and type of surgery (THA/TKA). Study findings including data reduction, display and comparison, conclusion andthe classification ofevidence from individual studies were then summarised in tabular form [30,31]. From each study, the extracted data on post-operative morbidity (including hospital readmission, complications and mortality) and PROMs were descriptively analysed and summarised in charts.
RESULTS
The search strategy generated a total of 754 unique articles, of which 80 full-text articles were assessed for eligibility. Following full text screening, 38 studies were eligible for analysis.
Study Characteristics
Ten studies were prospective cohort studies [32-85], Seventeen were retrospective studies [34-90], seven studies utilised the before and after design [38-81], and there were four case control studies [33-91]. No RCTs were included in the review. Twenty studies investigated patients undergoing THA and TKA, ten studies investigated TKA only and four studies THA only. Unilateral and bilateral TKA, unilateral and bilateral THA, bilateral TKA and bilateral THA were each investigated by one study. In all studies, there was a pre-operative, intra-operative and post-operative component to the ERAS protocol. Two studies investigated pre-operative optimisation as a stand-alone intervention in reducing readmissions or complications, with standardised intra-operative and post- operative protocols between groups [32,33]. All remaining studies had different peri-operative and post-operative protocols between groups and the effect size of the ERAS intervention was attributed to the implementation of all three components.
Type of Interventions
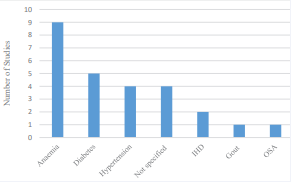
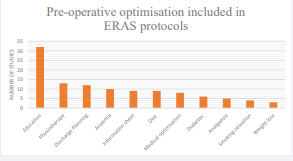
Thirty-two studies incorporated patient education and thirteen studies included physiotherapy as part of their pre-operative optimisation (Figure 2). In fourteen studies this was the only form of optimisation offered to patients. Nine studies offered medical optimisation before surgery, with five specifically focusing on diabetes (Figure 3). Three studies included weight loss for obesity management, but none specified the type of weight loss intervention offered. The details of pre-operative optimisation offered are summarised in Table 1.
Figure 2 Type of pre-operative optimisation utilised in ERAS protocols.
Figure 3 Type of medical optimisation offered to patients.
Table 1: Characteristics of pre-operative optimisation protocols from included studies.
|
Study Author |
Year |
Study Design |
Summary of pre-operative optimisation |
|
Ascione et al[51] |
2020 |
Prospective cohort |
Preoperative education and physiotherapy |
|
Auyong et al[37] |
2015 |
Retrospective cohort |
Preoperative education and discharge planning |
|
Azam et al[42] |
2021 |
Prospective cohort |
Preoperative education, physiotherapy, diabetes optimisation (HbA1c < 6.5%), hypertension and anaemia optimisation, dietary supplementation and smoking cessation advice |
|
Blum et al[46] |
2019 |
Retrospective cohort |
Preoperative education |
|
Christellis et al[38] |
2015 |
Before-and-after intervention |
Preoperative education, physiotherapy and dietician counselling |
|
de Carvalho et al[49] |
2021 |
Prospective cohort |
Preoperative education, physiotherapy and discharge planning |
|
Frassantio et al[75] |
2020 |
Prospective cohort |
Preoperative education and physiotherapy |
|
Garriga et al[76] |
2019 |
Retrospective cohort |
Medical assessment of haemoglobin levels and comorbidities including cardiovascular/respiratory disease |
|
Garriga et al[77] |
2019 |
Before and after intervention |
Preoperative education, physiotherapy and discharge planning |
|
Glassou et al[78] |
2014 |
Retrospective cohort |
Preoperative education |
|
Gleicher et al[79] |
2021 |
Before-and-after intervention |
Preoperative education and discharge planning |
|
Gwynne-Jones et al[43] |
2017 |
Before-and-after intervention |
Weekly preoperative education and physiotherapy |
|
Hansen et al[32] |
2012 |
Prospective cohort |
Identification and optimisation of risk factors: malnutrition, obesity, general health (hypertension, diabetes, infection), physiotherapy, cessation of smoking and alcohol consumption. |
|
Husted et al[80] |
2006 |
Prospective cohort |
Preoperative education and discharge planning |
|
Jiang et al[47] |
2019 |
Prospective cohort |
Preoperative physiotherapy |
|
Kelmer et al[33] |
2021 |
Case control |
Preoperative education, physiotherapy and discharge planning |
|
Maempel et al[81] |
2015 |
Before-and-after intervention |
Preoperative education and physiotherapy |
|
Maempel et al[52] |
2016 |
Retrospective cohort |
Preoperative education and physiotherapy |
|
Malviya et al[48] |
2011 |
Retrospective cohort |
Preoperative education |
|
Otte et al[82] |
2011 |
Case control |
Preoperative education |
|
Pamilo et al[44] |
2018 |
Before-and-after intervention |
Preoperative education and discharge planning |
|
Pamilo et al[45] |
2018 |
Before-and-after intervention |
Preoperative education and discharge planning |
|
Petersen et al[83] |
2020 |
Prospective cohort |
Preoperative education |
|
Picart et al[39] |
2021 |
Case-control |
Preoperative education and iron deficiency anaemia treated |
|
Plenge et al[84] |
2020 |
Prospective cohort |
Preoperative education, assessed in optimisation clinic, pre-op analgaesia rationalised, treatment of anaemia |
|
Qiu et al[36] |
2016 |
Retrospective cohort |
Preoperative education, medical optimisation (diabetes, hypertension, sleep apnoea, gout) in primary care and specialist setting, lifestyle modification (smoking, obesity) |
|
Ripolloes-Melchor et al[85] |
2020 |
Prospective cohort |
Preoperative education, smoking and alcohol cessation 4 weeks before surgery, anaemia treated |
|
Savaridas et al[86] |
2013 |
Retrospective cohort |
Preoperative education |
|
Stambough et al[87] |
2015 |
Retrospective cohort |
Preoperative education and analgaesia optimisation |
|
Starks et al[40] |
2014 |
Retrospective cohort |
Preoperative education, discharge planning, and pre-existing medical conditions optimised (anaemia, hypertension, ischaemic heart disease) |
|
Stowers et al[88] |
2016 |
Retrospective cohort |
Weekly education classes |
|
Van Horne et al[34] |
2019 |
Retrospective cohort |
Preoperative education, physiotherapy, medical optimisation of modifiable risk factors, weight loss and analgaesia optimisation |
|
Van Horne et al[35] |
2020 |
Retrospective cohort |
Preoperative education, physiotherapy, medical optimisation of modifiable risk factors, weight loss and analgaesia optimisation |
|
Vendittoli et al[89] |
2019 |
Retrospective cohort |
Preoperative education, physiotherapy, optimisation of anaemia, diabetes and other medical comorbidities |
|
Wilches et al[50] |
2017 |
Retrospective cohort |
Preoperative education, physiotherapy and treatment of anaemia |
|
Winther et al[90] |
2015 |
Retrospective cohort |
Preoperative education and physiotherapy |
|
Yanik et al[41] |
2018 |
Retrospective cohort |
Preoperative education |
|
Zhang et al[91] |
2018 |
Case control |
Preoperative education, physiotherapy, diet supplementation and analgaesia optimisation |
Duration of Intervention
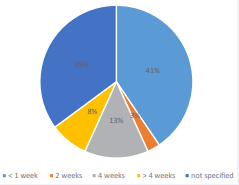
In twenty-one studies the duration of optimisation was assumed to be one day [33-90]. This consisted of a single preoperative clinic visit which incorporated education, physiotherapy or discharge planning without further optimisation before surgery (Figure 4). Four studies optimised patients for 4 weeks [32- 85], and two studies optimised patients for approximately 2 months [34, 35]. In one study surgery was delayed if necessary, allowing for sufficient duration for medical comorbidities to be managed [36]. In ten studies, the duration of optimisation was not stated.
Figure 4 Duration of pre-operative optimisation
Goals of Optimisation
In the five studies incorporating diabetes management,only one study set a target HbA1c for optimisation. None of the three studies utilising weight loss as an optimisation set a target weight or weight loss percentage. Two of the nine studies that included anaemia optimisation set a target haemoglobin. No studies followed up patients after the implementation of an intervention. In other words, the specific effect of the intervention on the organ or target of interest (e.g. effect of dietary intervention of weight) was not evaluated in any study.
Clinical Efficacy of Pre-Operative Optimisation Protocols on Post-Surgical Outcomes
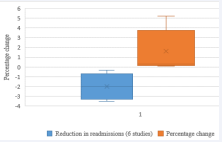
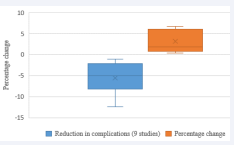
Primary Outcomes: The effects of pre-operative optimisation protocols alone on hospital readmissions and complications (both medical and surgical) following THA and TKA were unclear as most studies included differing pre-, peri-, and post-operative ERAS interventions, and did not investigate the stand-alone effect of pre-operative optimisation. The implementation of ERAS protocols showed a decrease in hospital readmissions within 90 days in six studies (median -1.8%, interquartile range (IQR) -2.3%) [33-41], and an increase in five studies (median 0.3%, IQR 3.6%) [36-45], compared to pre-ERAS protocols (Figure 5). For post-operative complications, nine studies [32-48], showed a decrease in incidence upon implementation of ERAS (median -5.0%, IQR -5.1%), with four studies [36-49], recording an increase (median 1.9%, IQR -5.3%) (Figure 6).
Figure 5 Box and whisker plot demonstrating change in readmission rate after implementation of ERAS. Separated into studies showing increase/decrease in readmissions.
Figure 6 Box and whisker plot demonstrating change in complication rate after implementation of ERAS. Separated into studies showing increase/ decrease in complications.
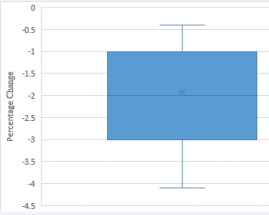
Secondary Outcomes: No study investigated the isolated impact of pre-operative optimisation (controlling the intra-operative and post-operative variables) on the length of stay or patient-reported outcomes. Therefore, the effects on in secondary outcomes were attributed to the implementation of ERAS as a whole, with no indication of the weighting of the pre-operative component to these differences. The implementation of ERAS resulted in a reduction in length of stay in 23 studies (median -2 days, IQR 2) (Figure 7), with one study reporting an increased length of stay (3.3 days) [50]. Patient-reported outcome measures were improved in seven studies [37-52]. Objectively measured physical function was improved after ERAS implementation in three studies [37-42]. No studies reported a deterioration in PROMs following implementation of ERAS.
Figure 7 Box and whisker plot demonstrating change in length of stay after ERAS implementation.
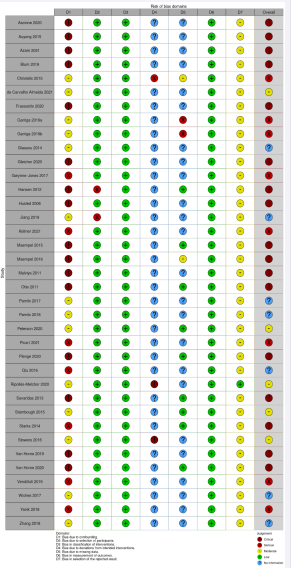
Risk of Bias
All studies included in the systematic review were observational studies, and a moderate to critical risk of bias was present in all studies (Figure 8). A moderate to critical degree of bias due to confounding affected all studies. There was low risk of selection and measurement bias, and an unclear risk of attrition bias.
DISCUSSION
This systematic review found that pre-operative optimisation protocols before THA and TKA focused heavily on patient education and physiotherapy, with a minority of studies optimising medical comorbidities and obesity. The duration of optimisation is likely to be inadequate in most studies for improvement of physiological processes or reversal of pathophysiology, and typically no follow-up has been undertaken to ensure patients are adequately optimised prior to surgery. There is conflicting evidence whether ERAS reduces complications or readmissions (Figure 5,6), however it appears that the length of hospital stay is reduced, and PROMs are improved. However, the evidence for the efficacy of pre-operative optimisation cannot be determined as very few studies investigated pre- operative optimisation alone in reducing complications or readmissions.The application of ERAS protocols to the peri-operative practice of multiple surgical sub-specialties has produced significant clinical and economic benefits. It was initially implemented in the field of colorectal surgery and there is a large body of evidence which demonstrates significant reductions in morbidity, faster recovery, and reduced hospital length of stay [53-55]. A significant amount of research has confirmed the efficacy of intra-operative components of ERAS. Standardised intra-operative anaesthetic protocols utilise neuraxial and regional anaesthesia, goal-directed fluid therapy, multimodal analgesia and prevention of post-operative nausea and
vomiting [56], and these intra-operative practices are associated with a lower incidence of post-operative pulmonary complications, acute kidney injury and opioid analgesia requirements [17-59]. Furthermore, surgical practices including the use of tranexamic acid to reduce blood loss, abolition of tourniquet use and surgical drains and early indwelling catheter removal are all evidence- based recommendations with robust evidence to support their use or not [60].
In comparison, the current pre-operative interventions for THA and TKA do not have the evidence to support their routine inclusion in ERAS protocols. Our review has shown that 23 of the 38 studies (60.5%) only offered patient education and/or physiotherapy with no other interventions. Although patient education is a low-cost intervention and unlikely to cause harm, two Cochrane reviews found little evidence that education influences pain, recovery, or reduce length of hospital stay and post- operative morbidity [61,62]. Pre-operative physiotherapy, in isolation, also does not confer any clinically important benefits and does not shorten length of hospital stay [63]. Therefore three-fifths of all current pre-operative protocols utilise ineffective strategies to optimise patients’ outcomes following THA and TKA.
The length of pre-operative optimisation was found to be grossly inadequate in most studies. Sixty three percent of the protocols interrogated had allocated one day (a single pre-admission clinic appointment) as the duration of the pre-operative optimisation. This is especially concerning in medical optimisation as the topic was scarcely addressed in the included studies. Medical optimisation is a key aspect of the ERAS protocol, aim to address numerous conditions that may influence surgical outcomes. By optimising these conditions prior to surgery, ERAS protocols aim to reduce complications such as infections, delayed wound healing, and prolonged hospital stays, ultimately improving overall recovery [64].
Despite the established benefits of preoperative medical optimisation, its application in practice appears to be limited. Among the studies that did offer some form of medical optimisation the duration varied significantly for patients- ranging from 2 weeks to over 1 month. Only one study which offered medical optimisation of chronic conditions specified a variable duration of optimisation to ensure sufficient time for patients’ conditions to be assessed and treated. This highlights a gap in the literature, as many studies did not detail the timing or adequacy of the preoperative optimisation period. No studies allocated follow-up to assess the efficacy of the interventions on the specific chronic condition, and no studies indicated that surgery was postponed if patients were not adequately optimised before surgery. The lack of consistency in the application and duration of medical optimisation in these studies points to a significant area for improvement within ERAS programs, where a more standardised approach to the management of comorbidities could help improve patient outcomes and safety.
Diabetes and obesity are two chronic medical conditions that have strong associations with post- operative complications including surgical site infection, periprosthetic joint infection, VTE and myocardial infarction [65-70]. It is postulated that hyperglycaemia adversely affects wound healing by delaying the synthesis of collagen and suppresses the immune response to infection by impairing phagocytosis [71,72], and obesity may influence the risk of a complication via a number of pathways including the influence of visceral fat on dysmetabolism and chronic inflammation [73]. These conditions are rarely diagnosed in isolation, and are strongly associated with other co-morbidities that may independently increase risk of complications such as coronary artery disease, hyperlipidaemia, hypertension, and sleep apnoea [74].
Our review has demonstrated that neither the length of optimisation nor the efficacy of interventions was sufficient to address these multifaceted issues. The three studies incorporating weight loss did not specify a modality or target weight, and only one study specified the duration of the weight loss program (4 weeks). Only one of the five studies optimising diabetes set a target HbA1c (6.5%), and similarly no duration was specified. Only one study referred patients to a specialist physician for management of diabetes. Obesity and diabetes are complex medical issues which have afflicted patients for many years prior to their arthroplasty surgery, and it is essential that these conditions are addressed by a multidisciplinary team of physicians, dieticians and allied health professionals [74]. Goals should be established, and sufficient time must be allocated prior to their surgery for interventions to be implemented for patients to have these conditions adequately optimised. The Australian Diabetes Society has set a target HbA1c of 8.0% for patients undergoing surgery and recommends postponing surgery if elevated. The Royal Australian College of General Practitioners has recommended a minimum weight loss target of 5–7.5% of body weight for patients with osteoarthritis [4]. There is no clear consensus on the duration of optimisation, however patients who are on the public hospital waiting list for THA (median 179 days) and TKA (median 308 days) [75], have a flexible time interval of several months which can be exploited to optimise patient comorbidities
in a multidisciplinary setting. Patients undertaking arthroplasty in a private hospital setting have a much smaller window for optimisation due to a significantly shorter waiting period (usually less than a month), and therefore the potential for optimisation of risk factors is considerably reduced.
The strength of this review is comprehensive analysis of all currently available pre-operative ERAS protocols. This is the first review presenting a thorough analysis of pre-operative optimisation components offered in all ERSA protocols. Other strengths of this review include the a priori protocol which was pre-registered and the strict adherence to the PRISMA guidelines for performing and reporting the review. The main weakness of this review is the moderate to high risk of bias in most included studies, which were observational and retrospective in nature. Further, intra-operative and post-operative components were not standardised between groups. The intervention being assessed in most studies was ERAS as a whole (encompassing pre-, peri-, and post-operative protocols), with only two studies evaluating the impact of pre-operative interventions on patient complications and readmissions. Meta-analysis of complications and readmissions was unable to be performed on the differences between ERAS and pre-ERAS groups given the degree of confounding in the results. Although a meta-analysis was not performed, it was clear that there was little evidence to inform the efficacy of pre-operative optimisation prior to THA or TKA. The effects of the pre-operative interventions studies (focusing heavily on education and physiotherapy) did not significantly change complication or readmission rates. Future studies investigating the utility of pre- operative optimisation must address the risk factors associated with post-operative adverse events, including diabetes, obesity and opioid use, with specified duration and targets for optimisation. Intra-operative and post- operative treatments between intervention groups must be standardised to reduce risk of bias.
CONCLUSION
Within the ERAS paradigm, current pre-operative optimisationprotocolsforTHAandTKAarepoorlydesigned, providing limited insight into the duration, frequency and number of interventions offered, with a heavy focus on low-quality interventions and little attention towards the duration, frequency and number of interventions offered. There is a paucity of evidence to guide the pre-operative management of chronic conditions known to be associated with post-operative morbidity and mortality. Given these limitations, it is unclear whether pre-operative optimisation affects readmission rates, complications or PROMs. Future work should be prospective and controlled, addressing risk factors associated with post-operative morbidity, particularly obesity and diabetes, in order to optimise patient outcomes.
DECLARATIONS
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors..
Authors’ contributions
VL and JL drafted the manuscript. WJC, JN and SA conceptualised the study and developed the methodology of the review. All the authors reviewed and approved the final version of the manuscript.
REFERENCES
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. E Clin Med. 2020; 29: 100587.
- Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014; 73: 1323.
- Osteoarthritis. In. Canberra. Australian Institute of Health Welfare. 2020.
- Guideline for the management of knee and hip osteoarthritisHigashi H, Barendregt JJ. Cost-effectiveness of total hip and knee replacements for the Australian population with osteoarthritis: discrete-event simulation model. PLoS One. 2011; 6: e25403.
- Ruiz D Jr, Koenig L, Dall TM, Gallo P, Narzikul A, Parvizi J, et al. The direct and indirect costs to society of treatment for end-stage knee osteoarthritis. J Bone Joint Surg Am. 2013; 95: 1473-1480.
- Saleh KJ, Kassim R, Yoon P, Vorlicky LN. Complications of total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2002; 31: 485-488.
- Della Rocca GJ, Leung KS, Pape HC. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011; 2: S66-S70.
- Wall C, de Steiger R. Pre operative optimisation for hip and knee arthroplasty. Aust J Gen Pract. 2020; 49: 710-714.
- Kee JR, Mears SC, Edwards PK, Barnes CL. Modifiable Risk Factors Are Common in Early Revision Hip and Knee Arthroplasty. J Arthroplasty. 2017; 32: 3689-3692.
- Alamanda VK, Springer BD. The prevention of infection: 12 modifiablerisk factors. Bone Joint J. 2019; 101: 3-9.
- Schroer WC, Diesfeld PJ, LeMarr AR, Morton DJ, Reedy ME. Modifiable Risk Factors in Primary Joint Arthroplasty Increase 90-Day Cost of Care. J Arthroplasty. 2018; 33: 2740-2744.
- Bonasia DE, Palazzolo A, Cottino U, Saccia F, Mazzola C, Rosso F, et al. Modifiable and Nonmodifiable Predictive Factors Associated with the Outcomes of Total Knee Arthroplasty. Joints. 2019; 7: 13-18.
- Bletterman AN, de Geest-Vrolijk ME, Vriezekolk JE, Nijhuis-van der Sanden MW, van Meeteren NL, Hoogeboom TJ. Preoperative psychosocial factors predicting patient’s functional recovery after total knee or total hip arthroplasty: a systematic review. Clin Rehabil. 2018; 32: 512-525.
- Larsen DB, Laursen M, Edwards RR, Simonsen O, Arendt-Nielsen L, Petersen KK. The Combination of Preoperative Pain, Conditioned Pain Modulation, and Pain Catastrophizing Predicts Postoperative Pain 12 Months After Total Knee Arthroplasty. Pain Med. 2021; 22: 1583-1590.
- Ljungqvist O, Young-Fadok T, Demartines N. The History of Enhanced Recovery After Surgery and the ERAS Society. J Laparoendosc Adv Surg Tech A. 2017; 27: 860-862.
- Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. BJA: Br J Anaesth. 2016; 117: iii62-iii72.
- Ljungqvist O, Hubner M. Enhanced recovery after surgery-ERAS- principles, practice and feasibility in the elderly. Aging Clin Exp Res. 2018; 30: 249-252.
- Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016; 117: iii62-iii72.
- Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK. Enhanced Recovery After Primary Total Hip and Knee Arthroplasty: A Systematic Review. J Bone Joint Surg Am. 2021; 103: 1938-1947.
- Hu ZC, He LJ, Chen D, Li XB, Feng ZH, Fu CW, et al. An enhanced recovery after surgery program in orthopedic surgery: a systematic review and meta-analysis. Orthop Surg Res. 2019; 14: 77.
- Adie S, Harris I, Chuan A, Lewis P, Naylor JM. Selecting and optimising patients for total knee arthroplasty. Med J Aust. 2019; 210: 135-141.
- Dowsey MM, Brown WA, Cochrane A, Burton PR, Liew D, Choong PF. Effect of Bariatric Surgery on Risk of Complications After Total Knee Arthroplasty: A Randomized Clinical Trial. JAMA Netw open. 2022; 5: e226722.
- Pavlovic N, Boland RA, Brady B, Genel F, Harris IA, Flood VM, et al. Effect of weight-loss diets prior to elective surgery on postoperative outcomes in obesity: A systematic review and meta-analysis. Clin Obesz. 2021; 11: e12485.
- Liu S, Blake E, Naylor JM, Adie S, Patanwala AE, Stevens J, et al. Letter to the Editor for the Article Titled “Opioid Tapering/Detoxification Protocols, A Compendium: Narrative Review”. Pain med. 2021; 22: 3102-3103.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Rev. 2015; 4: 1.
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015; 349: 7647.
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343: d5928.
- Sterne JA, Hernán MA, Reeves BC, Savovi? J, Berkman ND, ViswanathanM, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355: i4919.
- Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. Jo Develop Effect. 2012; 4: 409-429.
- Whittemore R, Knafl K. The integrative review: updated methodology.J Adv Nurs. 2005; 52: 546-553.
- Hansen TB, Bredtoft HK, Larsen K. Preoperative physical optimization in fast-track hip and knee arthroplasty. Dan Med J. 2012; 59: A4381.
- Kelmer GC, Turcotte JJ, Dolle SS, Angeles JD, MacDonald JH, King PJ. Preoperative Education for Total Joint Arthroplasty: Does Reimbursement Reduction Threaten Improved Outcomes? J Arthroplasty. 2021; 36: 2651-2657.
- Van Horne A, Van Horne J. Patient-optimizing enhanced recovery pathways for total knee and hip arthroplasty in Medicare patients: implication for transition to ambulatory surgery centers. Arthroplast Today. 2019. 5: 497-502.
- Van Horne A, Van Horne J. Presurgical optimization and opioid- minimizing enhanced recovery pathway for ambulatory knee and hip arthroplasty: postsurgical opioid use and clinical outcomes. Arthroplast Today. 2020; 6: 71-76.
- Qiu C, Cannesson M, Morkos A, Nguyen VT, LaPlace D, Trivedi NS, et al. Practice and Outcomes of the Perioperative Surgical Home in a California Integrated Delivery System. Anesth Analg. 2016; 123:59606.
- Auyong DB, Allen CJ, Pahang JA, Clabeaux JJ, MacDonald KM, Hanson NA. Reduced Length of Hospitalization in Primary Total Knee Arthroplasty Patients Using an Updated Enhanced Recovery After Orthopedic Surgery (ERAS) Pathway. J Arthroplast. 2015; 30: 1705-1709.
- Christelis N, Wallace S, Sage CE, Babitu U, Liew S, Dugal J, et al. An enhanced recovery after surgery program for hip and knee arthroplasty. Med J Aust. 2015; 202: 363-368.
- Picart B, Lecoeur B, Rochcongar G, Dunet J, Pegoix M, Hulet C. Implementation and results of an enhanced recovery (fast-track) program in total knee replacement patients at a French university hospital. Orthop Traumatol Surg Res. 2021; 107: 102851.
- Starks I, Wainwright TW, Lewis J, Lloyd J, Middleton RG. Older patients have the most to gain from orthopaedic enhanced recovery programmes. Age Ageing. 2014; 43: 642-648.
- Yanik JM, Bedard NA, Hanley JM, Otero JE, Callaghan JJ, Marsh JL. Rapid Recovery Total Joint Arthroplasty is Safe, Efficient, and Cost- Effective in the Veterans Administration Setting. J Arthroplast. 2018; 33: 3138-3142.
- Azam MQ, Goyal T, Paul S, Yadav AK, Govil N. Enhanced recovery protocol after single-stage bilateral primary total knee arthroplasty decreases duration of hospital stay without increasing complication rates. Eur J Orthop Surg Traumatol. 2021; 32: 711-717.
- Gwynne-Jones DP, Martin G, Crane C. Enhanced Recovery After Surgery for Hip and Knee Replacements. Orthop Nurs. 2017; 36: 203- 210.
- Pamilo KJ, Torkki P, Peltola M, Pesola M, Remes V, Paloneva J. Fast- tracking for total knee replacement reduces use of institutional care without compromising quality. Acta Orthop. 2018; 89: 184-189.
- Pamilo KJ, Torkki P, Peltola M, Pesola M, Remes V, Paloneva J. Reduced length of uninterrupted institutional stay after implementing a fast- track protocol for primary total hip replacement: Register-based analysis of 4 hospitals and 3,193 replacements. Acta Orthop. 2018; 89: 10-16.
- Blum CL, Akerman M, Callari M, Jordan E, Capozzi JD. Association of nausea and length of stay with carbohydrate loading prior to total joint arthroplasty. J Clin Out Manag. 2019; 26: 175-179.
- Jiang HH, Jian XF, Shangguan YF, Qing J, Chen LB. Effects of Enhanced Recovery After Surgery in Total Knee Arthroplasty for Patients Older Than 65 Years. Orthop Surg. 2019; 11: 229-235.
- Malviya A, Martin K, Harper I, Muller SD, Emmerson KP, Partington PF, et al. Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop. 2011; 82: 577-581.
- de Carvalho Almeida RF, Serra HO, de Oliveira LP. Fast-track versus conventional surgery in relation to time of hospital discharge following total hip arthroplasty: a single-center prospective study. J Orthop Surg Res. 2021; 16: 488.
- Wilches C, Sulbaran JD, Fernandez JE, Gisbert JM, Bausili JM, Pelfort X. Fast-track recovery technique applied to primary total hip and knee replacement surgery. Analysis of costs and complications. Rev Esp Cir Ortop Traumatol. 2017; 61: 111-116.
- Ascione F, Braile A, Romano AM, di Giunta A, Masciangelo M, Senorsky EH, et al. Experience-optimised fast rack improves outcomes and decreases complications in total knee arthroplasty. Knee. 2020; 27: 500-508.
- Maempel JF, Clement ND, Ballantyne JA, Dunstan E: Enhanced recovery programmes after total hip arthroplasty can result in reduced length of hospital stay without compromising functional outcome. Bone Joint J. 2016; 98: 475-482.
- Bagnall NM, Malietzis G, Kennedy RH, Athanasiou T, Faiz O, Darzi A. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal dis. 2014; 16: 947-956.
- Geltzeiler CB, Rotramel A, Wilson C, Deng L, Whiteford MH, Frankhouse J. Prospective study of colorectal enhanced recovery after surgery in a community hospital. JAMA Surg. 2014; 149: 955- 961.
- Rawlinson A, Kang P, Evans J, Khanna A. A systematic review of enhanced recovery protocols in colorectal surgery. Ann R Coll Surg Engl. 2011. 93: 583-588.
- Feldheiser A, Aziz O, Baldini G, Cox BPBW, Fearon KCH, Feldman LS, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016; 60: 289-334.
- Talboys R, Mak M, Modi N, Fanous N, Cutts S. Enhanced recovery programme reduces opiate consumption in hip hemiarthroplasty. Eur J Orthop Sur Traumatol. 2016. 26: 177-181.
- Hu S, Zhang ZY, Hua YQ, Li J, Cai ZD. A comparison of regional and general anaesthesia for total replacement of the hip or knee: a meta- analysis. The J Bone Joint Surg Br. 2009; 91: 935-942.
- Stundner O, Chiu YL, Sun X, Mazumdar M, Fleischut P, Poultsides L, et al. Comparative perioperative outcomes associated with neuraxial versus general anesthesia for simultaneous bilateral total knee arthroplasty. Reg Anesth Pain Med. 2012; 37: 638-644.
- Wainwright TW, Gill M, McDonald DA, Middleton RG, Reed M, Sahota O, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020; 91: 3-19.
- McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev. 2004; 1: Cd003526.
- McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A. Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 2014. 2014; 5: Cd003526.
- Wang L, Lee M, Zhang Z, Moodie J, Cheng D, Martin J. Does preoperative rehabilitation for patients planning to undergo joint replacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2016; 6: e009857.
- Australian Physiotherapy Association. Five facts about enhanced recovery after joint replacement. Australian Physiotherapy Association. 2024
- Gu A, Wei C, Robinson HN, Sobrio SA, Liu J, Sculco TP, et al. Postoperative Complications and Impact of Diabetes Mellitus Severity on Revision Total Knee Arthroplasty. The J Knee Surg. 2020; 33: 228-234.
- López-de-Andrés A, Hernández-Barrera V, Martínez-Huedo MA, Villanueva-Martinez M, Jiménez-Trujillo I, Jiménez-García R. Type 2 diabetes and in-hospital complications after revision of total hip and knee arthroplasty. PLOS ONE. 2017; 12: e0183796.
- Qin W, Huang X, Yang H, Shen M. The Influence of Diabetes Mellitus on Patients Undergoing Primary Total Lower Extremity Arthroplasty: A Systematic Review and Meta-Analysis. BioMed Res Int. 2020; 2020: 6661691.
- Courtney PM, Boniello AJ, Berger RA. Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database. J Arthroplasty. 2017; 32: 1426-1430.
- Menendez ME, Memtsoudis SG, Opperer M, Boettner F, Gonzalez Della Valle A. A nationwide analysis of risk factors for in-hospital myocardial infarction after total joint arthroplasty. Int Orthop. 2015; 39: 777-786.
- Yang Z, Liu H, Xie X, Tan Z, Qin T, Kang P. The influence of diabetes mellitus on the post-operative outcome of elective primary total knee replacement: a systematic review and meta-analysis. Bone Joint J. 2014; 96: 1637-1643.
- Robertson HD, Polk HC Jr. The mechanism of infection in patients with diabetes mellitus: A review of leukocyte malfunction. Surgery. 1974; 75: 123-128.
- Goodson WH 3rd, Hung TK. Studies of wound healing in experimental diabetes mellitus. The J Surg Res. 1977; 22: 221-227.
- Doyle SL, Lysaght J, Reynolds JV. Obesity and post-operative complications in patients undergoing non-bariatric surgery. Obesity Rev. 2010; 11: 875-886.
- Obesity and total joint arthroplasty: a literature based review. The J Arthroplasty. 2013; 28: 714-721.
- Health AIo, Welfare: Annual report 2021–22. In. Canberra: AIHW. 2022.
- Frassanito L, Vergari A, Nestorini R, Cerulli G, Placella G, Pace V, et al. Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet Sur. 2020; 104: 87-92.
- Garriga C, Murphy J, Leal J, Arden NK, Price AJ, Prieto-Alhambra D, et al. Assessment on patient outcomes of primary hip replacement: an interrupted time series analysis from ‘The National Joint Registry of England and Wales’. BMJ Open. 2019; 9: e031599.
- Garriga C, Murphy J, Leal J, Price A, Prieto-Alhambra D, Carr A, et al. Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: an interrupted time series analysis from “The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man”. Osteoarthritis Cartilage. 2019; 27: 1280-1293.
- Glassou EN, Pedersen AB, Hansen TB. Risk of re-admission,
reoperation, and mortality within 90 days of total hip and knee arthroplasty in fast-track departments in Denmark from 2005 to 2011. Acta Orthop. 2014; 85: 493-500.
- Gleicher Y, Siddiqui N, Mazda Y, Matelski J, Backstein DJ, Wolfstadt JI. Reducing Acute Hospitalization Length of Stay After Total Knee Arthroplasty: A Quality Improvement Study. J Arthroplasty. 2021; 36: 837-844.
- Husted H, Holm G. Fast track in total hip and knee arthroplasty-- experiences from Hvidovre University Hospital, Denmark. Injury. 2006; 37: S31-S35.
- Maempel JF, Walmsley PJ. Enhanced recovery programmes can reduce length of stay after total knee replacement without sacrificing functional outcome at one year. Ann R Coll Surg Engl. 2015; 9: 563- 567.
- Otte KS, Husted H, Ãrsnes T, Kehlet H. Bilateral simultaneous total hip arthroplasty in a fast track setting. Hip Int. 2011; 21: 336-339.
- Petersen PB, Jørgensen CC, Kehlet H, Group LFCfF-tH Knee Replacement C. Fast-track hip and knee arthroplasty in older adults—a prospective cohort of 1,427 procedures in patients ≥ 85 years. Age Ageing. 2020; 49: 425-431.
- Plenge U, Parker R, Davids S, Davies GL, Fullerton Z, Gray L, et al. Quality of recovery after total hip and knee arthroplasty in South Africa: a national prospective observational cohort study. BMC Musculoskelet Disord. 2020; 21: 721.
- Ripolles-Melchor J, Abad-Motos A, Diez-Remesal Y, Aseguinolaza- Pagola M, Padin-Barreiro L, Sanchez-Martin R, et al. Association Between Use of Enhanced Recovery After Surgery Protocol and
-
Postoperative Complications in Total Hip and Knee Arthroplasty in the Postoperative Outcomes Within Enhanced Recovery After Surgery Protocol in Elective Total Hip and Knee Arthroplasty Study (POWER2). JAMA Surg. 2020; 155: e196024.
- Savaridas T, Serrano-Pedraza I, Khan SK, Martin K, Malviya A, Reed MR. Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. Acta Orthop. 2013; 84: 40-43.
- Stambough JB, Nunley RM, Curry MC, Steger-May K, Clohisy JC. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty. 2015; 30: 521-526.
- Stowers MD, Manuopangai L, Hill AG, Gray JR, Coleman B, Munro JT. Enhanced Recovery After Surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J Surg. 2016; 86: 475-479.
- Vendittoli PA, Pellei K, Desmeules F, Masse V, Loubert C, Lavigne M, et al. Enhanced recovery short-stay hip and knee joint replacement program improves patients outcomes while reducing hospital costs. Orthop Traumatol Surg Res. 2019; 105: 1237-1243.
- Winther SB, Foss OA, Wik TS, Davis SP, Engdal M, Jessen V, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop. 2015; 86: 78-85.
- Zhang S, Huang Q, Xie J, Xu B, Cao G, Pei F. Factors influencing postoperative length of stay in an enhanced recovery after surgery program for primary total knee arthroplasty. J Orthop Sur. 2018; 13: 29.