Selective Patellar Resurfacing in Total Knee Arthroplasty: A 10-Year Retrospective Cohort Study of Outcomes and Risk Factors
- 1. Institute for Orthopaedics Banjica, Belgrade, Serbia
- 2. University of Belgrade, Faculty of Medicine, Belgrade, Serbia
- 3. Military Medical Academy, Belgrade, Serbia
Abstract
The necessity of patellar resurfacing in Total Knee Arthroplasty (TKA) remains controversial. This study compared outcomes between resurfaced and non resurfaced patients to identify subgroups that benefit most from the procedure. A retrospective analysis of 625 patients undergoing PCL-sacrificing TKA (2012-2023) was conducted. Patients were categorized into non-resurfaced (n=469, 75%) and resurfaced (n=156, 25%) cohorts. Resurfacing was selectively performed for patients with rheumatoid arthritis (RA), severe patellofemoral degeneration, obesity, or prior patellar fractures. Outcomes included functional scores (KSS, WOMAC), pain (VAS), and patient satisfaction (measured via a scores (VAS, WOMAC) or patient satisfaction levels between the two groups. standardized survey).The resurfaced group was significantly older and had higher rates of secondary osteoarthritis, RA, osteoporosis, and prior contralateral knee surgery. Postoperatively, the resurfaced group demonstrated a significant reduction in crepitation. However, there were no significant differences in pain Conclusion: Patellar resurfacing in TKA improves patellofemoral mechanics in high-risk subgroups (those with RA, secondary OA, osteoporosis, or prior surgery). While it did not confer superior pain relief or satisfaction compared to non-resurfacing, selective resurfacing based on these specific risk factors is supported to optimize biomechanical outcomes. A tailored approach, guided by patient-specific factors and intraoperative findings, is recommended.
Keywords
• Total knee arthroplasty
• Patella replacement
• Resurfacing
Citation
Gluš?evi? B, Aleksi? B, Milosavljevi? D, Manojlovi? N, Gluš?evi? M, et al. (2025) Selective Patellar Resurfacing in Total Knee Arthroplasty: A 10-Year Retrospective Cohort Study of Outcomes and Risk Factors. Ann Musc Disord 6(1): 1016.
ABBREVIATIONS
FKSS: Functional Knee Society Score; KSS: Knee Society Score; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; VAS: Visual Analog Scale (Pain: 0–10); Preop: Preoperative;| Postop: Postoperative; Sig.*: Independent Samples T-test (between-group differences); Sig.# : ANOVA (within-group changes over time).
INTRODUCTION
Total knee arthroplasty is a highly successful procedure with growing adoption, yet some controversies persist—including the question of patellar replacement [1,2]. While patellar resurfacing has received less dedicated research attention than TKA as a whole, it plays a critical role in improving functionality and quality of life in specific patient populations [3,4]. The decision of whether to perform patellar resurfacing during Total Knee Arthroplasty (TKA) remains a subject of debate among orthopedic surgeons [5,6]. While some advocate for routine resurfacing to reduce postoperative anterior knee pain and improve functional outcomes [7,8], others prefer selective or non-resurfacing approaches, citing potential complications such as patellar fractures, implant loosening, or overstuffing of the patellofemoral joint [9,10]. However, existing studies lack consensus on which patient subgroups (e.g., Rheumatoid Arthritis [RA], osteoporosis, or severe patellofemoral damage) benefit most from resurfacing, highlighting the need for evidence tailored to individualized decision-making [10,11]. To address this gap, this study aimed to identify specific patient subgroups that derive the greatest benefit from patellar resurfacing by comparing demographic, clinical, and surgical outcomes between resurfaced and non resurfaced cohorts in a large, single-center population. We hypothesized that patients with specific risk factors— including rheumatoid arthritis, secondary osteoarthritis, osteoporosis, or a history of prior contralateral knee surgery—would demonstrate superior patellofemoral mechanics and functional outcomes following patellar resurfacing compared to those without resurfacing. To test this hypothesis, we compared the clinical and demographic characteristics of patients who underwent patellar resurfacing during TKA with those who did not over a 10-year period. By analyzing these variables, this study seeks to provide actionable insights for surgical planning and refine evidence-based indications for this procedure [8,12].
METHODS
This retrospective study analyzed data from 625 patients who underwent posterior cruciate ligament (PCL)-sacrificing Total Knee Arthroplasty (TKA) between 2012 and 2023 at the Department of General Orthopedics 3, Orthopedic Institute Hospital “Banjica,” with a follow up period of 10 years [13-15]. The patients were divided into two groups: 469 patients (75%) who did not undergo patellar resurfacing with a polyethylene patellar button during TKA and 156 patients (25%) who did [16,17]. The 75%/25% split reflected patient-specific factors, including the presence of Rheumatoid Arthritis (RA), severe patellofemoral degeneration, obesity, or prior patellar fractures, as detailed below. Clinical and demographic variables were collected for each patient, including gender, age, cause of osteoarthritis (primary or secondary) [18,19], and previous surgeries on the contralateral knee or other joints [20]. All implants were cemented, and patellar components (when used) were dome-shaped. Functional outcomes were assessed using the Kujala Score, Functional Knee Society Score (FKSS), Knee Society Score (KSS), and WOMAC, while pain was measured via Visual Analog Scale (VAS).The study assessed these variables using chi-square tests for categorical data and t-tests for continuous data, with statistical significance set at p < 0.05 [21,22]. Patients were also evaluated for comorbidities such as hypertension (HTA) [23], diabetes mellitus (DM) [24], rheumatoid arthritis (RA) [25,26], and osteoporosis [27], among others, to identify any potential association between these conditions and the likelihood of undergoing patellar resurfacing.In our practice, the decision to perform patellar resurfacing was influenced by specific clinical criteria. For patients with rheumatoid arthritis (RA), patellar resurfacing was routinely performed due to the potential impact of residual cartilage on the synovium, which could contribute to chronic synovitis and pannus formation [28-30]. In patients with degenerative joint disease, patellar resurfacing was indicated in cases of significant patellofemoral arthritis, characterized by complete cartilage loss, eburnated bone, and severe anterior knee pain [31-33]. Additionally, patellar resurfacing was performed in obese patients [34,35] and those with a history of patellar fractures [36,37]. These criteria guided our surgical approach and were consistently applied throughout the study period [38].A complete statistical analysis was performed using the IBM SPSS software, version 26.0. The Kolmogorov Smirnov test was used to assess the normality of the distribution for numerical data. Numerical data are presented as mean values with standard deviation. The significance of differences in continuous variables was tested using parametric tests: The Independent Samples t-test and Paired Samples t-test for comparisons between two groups, and ANOVA for comparisons involving three or more measurements, with Bonferroni correction and Tukey’s HSD post-hoc test applied as needed. Categorical data are presented as absolute and relative frequencies, and the significance of differences between subgroups was assessed using the Chi-square test. This analysis ensured rigorous statistical evaluation of the data, accounting for both continuous and categorical variables while maintaining appropriate corrections for multiple comparisons.
RESULTS
Patient Demographics: Of the total 625 patients, 469 (75%) did not undergo patellar replacement surgery, and 156 (25%) did. The gender distribution was slightly skewed, with 96 (20.5%) men and 373 (79.5%) women in the non-replacement group, and 26 (16.7%) men and 130 (83.3%) women in the replacement group. Gender did not show a statistically significant difference (p = 0.357). The mean age of patients who did not undergo patellar replacement was 66.30 ± 7.33 years, while the mean age for those who underwent the procedure was 67.89 ± 9.84 years (p = 0.033). Cause of Osteoarthritis: A significant difference was observed between the groups in terms of the cause of osteoarthritis. Of the patients who did not undergo patellar replacement, 91.7% had primary OA, and 8.3% had secondary OA. In contrast, 75% of those who underwent patellar replacement had primary OA, while 25% had secondary OA (p < 0.001). This suggests that secondary OA is a more common cause for undergoing patellar replacement surgery.Second Knee Surgery: A higher percentage of patients who underwent patellar replacement had previously undergone surgery on the contralateral knee. Specifically, 32.1% of patients who had patellar replacement had surgery on the second knee, compared to 22.2% of patients who did not undergo patellar replacement (p = 0.018). This finding indicates a higher likelihood of bilateral knee involvement in patients requiring patellar replacement. Comorbidities: Among the most common comorbidities, hypertension (HTA) was observed in 55.4% of patients who did not undergo patellar replacement compared to 44.9% in the replacement group (p = 0.028). Additionally, rheumatoid arthritis (RA) was significantly more prevalent in the group undergoing patellar replacement (14.1%) compared to the non-replacement group (5.1%) (p < 0.001). The presence of osteoporosis was also more common in the replacement group (6.4% vs. 1.7%, p = 0.006). Clinical Outcomes: When analyzing pain levels before and after surgery using the Visual Analog Scale (VAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), no significant differences were observed between the two groups (Table 1).
Table 1: Differences in pain intensity and satisfaction with surgery.
|
Parameter |
No Patellar Resurfacing |
Patellar Resurfacing |
p-value* |
|
Preoperative VAS pain |
10.00 ± 0.00 |
10.00 ± 0.00 |
/ |
|
Postoperative VAS pain |
1.60 ± 0.61 |
1.66 ± 0.62 |
0.313 |
|
p-value # |
<0.001 |
<0.001 |
|
|
Satisfaction score |
9.67 ± 0.47 |
9.66 ± 0.50 |
0.798 |
Independent Samples Test; #Paired Samples Test
|
|
Without Patellar Replacement |
With Patellar Replacement |
Sig. (p-value) |
|
Number of patients |
469 (75.0%) |
156 (25.0%) |
|
|
Gender: Male / Female |
96 (20.5%) / 373 (79.5%) |
26 (16.7%) / 130 (83.3%) |
0.357* |
|
Age (years) |
66.30 ± 7.33 |
67.89 ± 9.84 |
0.033# |
|
Cause: Primary / Secondary Osteoarthritis |
430 (91.7%) / 39 (8.3%) |
117 (75.0%) / 39 (25.0%) |
<0.001* |
|
Surgery on other knee: No / Yes |
365 (77.8%) / 104 (22.2%) |
106 (67.9%) / 50 (32.1%) |
0.018* |
|
Surgery on other joint: No / Yes |
425 (90.6%) / 44 (9.4%) |
142 (91.0%) / 14 (9.0%) |
1.000* |
*- Chi-square test; #- Independent Samples Test
Comorbidities
|
|
Without Patellar Replacement |
With Patellar Replacement |
Sig. (p-value) |
|
No comorbidities |
67 (14.3%) |
9 (5.8%) |
0.007 |
|
Hypertension |
260 (55.4%) |
70 (44.9%) |
0.028 |
|
Diabetes Mellitus |
72 (15.4%) |
23 (14.7%) |
0.956 |
|
Cerebrovascular Disease |
14 (3.0%) |
2 (1.3%) |
0.382 |
|
Chronic Obstructive Pulmonary Disease |
22 (4.7%) |
12 (7.7%) |
0.219 |
|
Anemia |
9 (1.9%) |
3 (1.9%) |
1.000 |
|
Angina Pectoris |
5 (1.1%) |
1 (0.6%) |
1.000 |
|
Arrhythmias |
38 (8.1%) |
7 (4.5%) |
0.182 |
|
Asthma |
11 (2.3%) |
8 (5.1%) |
0.138 |
|
Rheumatoid Arthritis |
24 (5.1%) |
22 (14.1%) |
<0.001 |
|
Breast Cancer |
35 (7.5%) |
26 (16.7%) |
0.001 |
|
Hypothyroidism |
36 (7.7%) |
12 (7.7%) |
1.000 |
|
Gastritis |
10 (2.1%) |
4 (2.6%) |
0.997 |
|
Myocardial Infarction |
11 (2.3%) |
2 (1.3%) |
0.630 |
|
Benign Prostatic Hyperplasia |
3 (0.6%) |
1 (0.6%) |
1.000 |
|
Nodular Goiter |
/ |
2 (1.3%) |
0.101 |
|
Osteoporosis |
8 (1.7%) |
10 (6.4%) |
0.006 |
|
Lupus |
1 (0.2%) |
/ |
1.000 |
|
Thrombosis |
2 (0.4%) |
/ |
1.000 |
|
Thrombocytopenia |
1 (0.2%) |
/ |
1.000 |
|
Sjögren's Syndrome |
1 (0.2%) |
/ |
1.000 |
|
Non-Hodgkin's Lymphoma |
1 (0.2%) |
/ |
1.000 |
|
Heart Defects |
5 (1.1%) |
2 (1.3%) |
1.000 |
|
Arthralgia |
22 (4.7%) |
8 (5.1%) |
0.996 |
|
Back Pain |
15 (3.2%) |
3 (1.9%) |
0.583 |
|
Kidney Cancer |
1 (0.2%) |
/ |
1.000 |
|
Cerebrovascular disease |
5 (1.1%) |
3 (1.9%) |
0.679 |
|
Depression |
8 (1.7%) |
1 (0.6%) |
0.563 |
|
Bronchitis |
2 (0.4%) |
/ |
1.000 |
|
Epilepsy |
2 (0.4%) |
1 (0.6%) |
1.000 |
|
Hyperthyroidism |
1 (0.2%) |
1 (0.6%) |
0.999 |
|
Tuberculosis |
/ |
1 (0.6%) |
0.563 |
|
Parkinson's Disease |
1 (0.2%) |
1 (0.6%) |
0.999 |
|
Glaucoma |
1 (0.2%) |
2 (1.3%) |
0.315 |
|
Hashimoto's Thyroiditis |
1 (0.2%) |
/ |
1.000 |
|
Dementia |
1 (0.2%) |
/ |
1.000 |
|
Lung Cancer |
1 (0.2%) |
/ |
1.000 |
|
Colon Cancer |
1 (0.2%) |
/ |
1.000 |
|
Hiatal Hernia |
1 (0.2%) |
/ |
1.000 |
|
Gout |
2 (0.4%) |
/ |
1.000 |
|
Leukopenia |
1 (0.2%) |
/ |
1.000 |
*- Chi-square test; Cumulative percentages
Notes:
• Sig. = Significance (p-value)
• # = Independent Samples Test (likely t-test for age comparison)
/ = No cases reported
crepitation compared to the non-resurfaced group (p < 0.05), suggesting improved patellofemoral joint mechanics. Regarding satisfaction levels, no significant differences were found between the two surgical approaches.
DISCUSSION
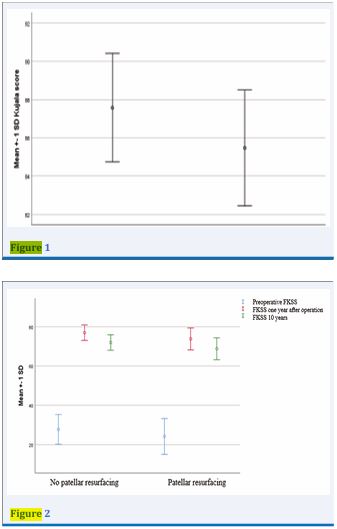
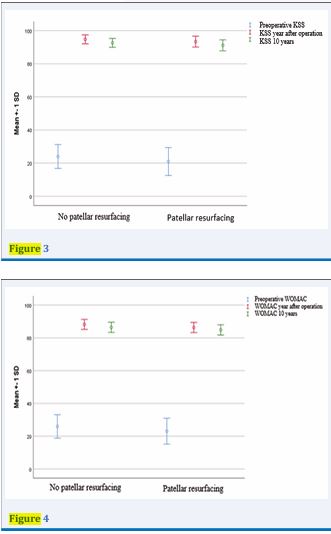
Clinical Outcomes Comparison: Without Patellar Replacement vs. With Patellar Replacement
|
Parameter |
Without Patellar Replacement |
With Patellar Replacement |
Sig. (p-value) |
|
Kujala Score |
87.57 ± 2.84 |
85.47 ± 3.03 |
<0.001* |
|
FKSS (Preop) |
27.74 ± 7.58 |
24.17 ± 9.14 |
<0.001* |
|
FKSS (1 Year Postop) |
76.98 ± 3.96 |
73.81 ± 5.57 |
<0.001* |
|
FKSS (10 Years Postop) |
71.98 ± 3.96 |
68.81 ± 5.57 |
<0.001* |
|
Sig.# (Time Effect) |
<0.001 |
<0.001 |
|
|
KSS (Preop) |
23.99 ± 7.21 |
20.98 ± 8.44 |
<0.001* |
|
KSS (1 Year Postop) |
94.73 ± 2.67 |
93.31 ± 3.29 |
<0.001* |
|
KSS (10 Years Postop) |
92.60 ± 2.69 |
91.12 ± 3.31 |
<0.001* |
|
Sig.# (Time Effect) |
<0.001 |
<0.001 |
|
|
WOMAC (Preop) |
25.96 ± 7.17 |
23.08 ± 7.91 |
<0.001* |
|
WOMAC (1 Year Postop) |
88.22 ± 3.04 |
86.32 ± 3.10 |
<0.001* |
|
WOMAC (10 Years Postop) |
86.42 ± 3.09 |
84.86 ± 3.16 |
<0.001* |
|
Sig.# (Time Effect) |
<0.001 |
<0.001 |
|
|
VAS Pain (Preop) |
10.00 ± 0.00 |
10.00 ± 0.00 |
1.000 |
|
VAS Pain (Postop) |
1.60 ± 0.61 |
1.66 ± 0.62 |
0.313 |
|
Satisfaction Score |
9.67 ± 0.47 |
9.66 ± 0.50 |
0.798 |
Patellar resurfacing during Total Knee Arthroplasty (TKA) remains one of the most debated topics in orthopedic surgery [3-39]. The decision to resurface or not to resurface the patella is influenced by a variety of factors, including patient demographics, underlying pathology, surgeon preference, and the potential for postoperative complications [6-41]. This discussion will explore the general principles of patellar resurfacing in TKA, followed by an analysis of the results presented in this study, which compare outcomes between patients who underwent TKA with and without patellar resurfacing. The findings will be contextualized within the broader literature to provide a comprehensive understanding of the implications of patellar resurfacing [42]. The patellofemoral joint is a critical component of knee biomechanics, contributing to knee extension, stability, and overall function [3-43]. During TKA, the management of the patella - whether to resurface it or leave it unsurfaced - has significant implications for postoperative outcomes, including anterior knee pain, patellar tracking, and the need for revision surgery [44,45]. The indication for patellar resurfacing is typically considered in patients with significant patellofemoral arthritis, patellar maltracking, or those with a history of anterior knee pain [46]. Resurfacing involves removing the articular cartilage of the patella and replacing it with a prosthetic component, which aims to improve patellar tracking and reduce pain [46,47]. However, the procedure is not without risks, including patellar fracture, implant loosening, and increased surgical complexity [48]. The controversy surrounding patellar resurfacing in TKA stems from conflicting evidence regarding its benefits and risks [49], with some studies demonstrating reduced anterior knee pain and revision rates when resurfacing is performed, while others suggest the potential complications may outweigh these advantages, particularly in cases with minimal patellofemoral involvement [50]. This divergence in outcomes has led to persistent debate within the orthopedic community, further complicated by the influence of patient-specific factors such as age, activity level, and comorbidities on surgical decision-making [17]. The results of this study provide valuable insights into the characteristics and outcomes of patients who underwent TKA with and without patellar resurfacing. The analysis of 469 patients without patellar resurfacing (75.0%) and 156 patients with patellar resurfacing (25.0%) reveals several important findings. The study population was predominantly female, with women comprising 79.5% of the non-resurfaced group and 83.3% of the resurfaced group. This is consistent with the general trend in TKA populations. The mean age of patients in the resurfaced group was slightly higher (67.89 ± 9.84 years) compared to the non-resurfaced group (66.30 ± 7.33 years), with a statistically significant difference (p = 0.033). This suggests that older patients may be more likely to receive patellar resurfacing, possibly due to concerns about patellar wear or instability in older individuals with longer-standing arthritis.The primary indication for surgery in both groups was osteoarthritis, with 91.7% of the non-resurfaced group and 75.0% of the resurfaced group undergoing TKA for primary osteoarthritis. However, the resurfaced group had a significantly higher proportion of patients with secondary osteoarthritis (25.0% vs. 8.3%, p < 0.001). This finding may indicate that surgeons are more likely to resurface the patella in cases of secondary osteoarthritis, where the patellofemoral joint may be more severely affected. Additionally, the resurfaced group had a higher rate of prior surgery on the contralateral knee (32.1% vs. 22.2%, p = 0.018), suggesting that patients with a history of knee surgery may be more likely to undergo patellar resurfacing, possibly due to prior complications or persistent symptoms related to the patellofemoral joint. The comorbidity profiles of the two groups revealed several significant differences. Patients in the resurfaced group had a lower prevalence of hypertension (HTA) (44.9% vs. 55.4%, p = 0.028) and a higher prevalence of rheumatoid arthritis (RA) (14.1% vs. 5.1%, p < 0.001). The higher prevalence of RA in the resurfaced group is particularly noteworthy, as rheumatoid arthritis is known to affect the patellofemoral joint more severely than osteoarthritis. This may explain why surgeons are more likely to resurface the patella in these patients, as the inflammatory nature of RA can lead to greater cartilage degradation and patellar instability. A higher prevalence of osteoporosis was also observed in the resurfaced group (6.4% vs. 1.7%, p = 0.006). Osteoporosis can affect the integrity of the patellar bone, making it more susceptible to fractures or complications if left unresurfaced. This may explain why surgeons are more likely to resurface the patella in patients with osteoporosis, as resurfacing may provide additional stability and reduce the risk of patellar fractures. The decision to resurface the patella during TKA remains a topic of debate in the orthopedic community [17]. Proponents of patellar resurfacing argue that it reduces the risk of anterior knee pain, improves patellar tracking, and decreases the need for revision surgery [3]. Opponents, however, point to the potential complications associated with resurfacing, such as patellar fractures, implant loosening, and increased surgical time [3-45]. The results of this study suggest that the outcomes of TKA with and without patellar resurfacing are similar in many respects. For example, there were no significant differences between the two groups in terms of other comorbidities such as diabetes mellitus (DM) or chronic obstructive pulmonary disease (COPD). This indicates that the presence of these comorbidities does not appear to influence the decision to resurface the patella, nor do they significantly affect the outcomes of TKA in either group. However, the higher prevalence of RA and osteoporosis in the resurfaced group suggests that these conditions may play a role in the decision-making process [6-18]. Patients with RA or osteoporosis may benefit more from patellar resurfacing due to the increased risk of patellofemoral complications in these populations [17,18]. Additionally, the higher rate of prior contralateral knee surgery in the resurfaced group may indicate that these patients have a higher likelihood of experiencing patellofemoral issues, prompting surgeons to resurface the patella to prevent recurrent problems.
Limitations of the Study
While this study offers valuable insights into the characteristics and outcomes of patients undergoing total knee arthroplasty (TKA) with and without patellar resurfacing, it is important to acknowledge its limitations. Firstly, the retrospective design of the study restricts the ability to establish definitive causal relationships between patellar resurfacing and clinical outcomes. Secondly, the sample size of the resurfaced group (n = 156) is notably smaller compared to the non-resurfaced group (n = 469), potentially impacting the statistical power and generalizability of the findings. Additionally, a significant limitation of our study is that all procedures were conducted within a single hospital and a single department. This may introduce bias and limit the external validity of the results, as the outcomes may not be representative of practices or patient populations in other settings. Future multicenter studies with larger, more balanced cohorts and extended follow-up periods are needed to further validate these findings.
CONCLUSION
In summary, the prevailing evidence supports a deliberate and selective strategy for patellar resurfacing in total knee arthroplasty (TKA). Based on our clinical outcomes, we strongly advocate for resurfacing in identified high-risk patient cohorts. This includes patients with inflammatory arthropathies such as rheumatoid arthritis, those with secondary osteoarthritis, individuals diagnosed with osteoporosis, and patients with a history of prior knee surgery. In these groups, patellar resurfacing demonstrably improves patellofemoral joint kinematics and significantly reduces the incidence of postoperative complications, particularly anterior knee pain and audible crepitation.It is important to note that for the general population, reported outcomes for pain relief and overall patient satisfaction remain equivalent between resurfaced and non-resurfaced cohorts. This fundamental equivalence is why a universal policy is not justified. Instead, the intraoperative assessment is critical; resurfacing should be performed when there is visible evidence of significant patellofemoral degeneration, ranging from full-thickness cartilage wear to eburnated bone. It is important to note that for the general population, reported outcomes for pain relief and overall patient satisfaction remain equivalent between resurfaced and non-resurfaced cohorts. This fundamental equivalence is why a universal policy is not justified. Instead, the intraoperative assessment is critical; resurfacing should be performed when there is visible evidence of significant patellofemoral degeneration, ranging from full-thickness cartilage wear to eburnated bone.research with larger, prospective trials will help to further refine these indications. Until then, a selective approach, guided by patient-specific factors and surgical findings, represents the optimal standard of care for patellofemoral management in TKA.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Competing interests
The authors declare that they have no competing interests in this section.
Funding
Not applicable
Authors’ contributions
A.B. and G.B. wrote the main manuscript text and G.M and N. M prepared tables, M.D and M.D prepared all data base. R.M does all statics. All authors reviewed the manuscript.
Acknowledgements
Not applicable.
REFERENCES
- Petersen W, Rembitzki IV, Brüggemann GP, Ellermann A, Best R, Koppenburg AG, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop. 2014; 38: 319-328.
- Spencer SJ, Young D, Blyth MJG. Secondary resurfacing of the patella in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020; 28: 1150-1158.
- Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005; 438: 191-196.
- Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am. 2012 ; 94: 2270-2278.
- Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005; 87: 1438- 1445.
- Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006; 88: 734-739.
- Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007; 464: 65-72.
- Chen K, Li G, Fu D, et al. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop. 2013; 37: 1075-1083.
- Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, MyersL. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow- up. J Bone Joint Surg Am. 2001; 83: 1376-1381.
- He JY, Jiang LS, Dai LY. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee. 2011; 18: 137-144.
- Wood DJ, Smith AJ, Collopy D, et al. Patellar resurfacing in total knee arthroplasty: a ten-year prospective randomized controlled trial. J Bone Joint Surg Am. 2002; 84: 983-990.
- Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003; 85: 212-217.
- Smith TO, Hing CB, Davies L, Donell ST. Fixed versus mobile bearing total knee arthroplasty. Bone Joint J. 2019; 101: 133-140.
- Van Der List JP, Chawla H, Zuiderbaan HA, Pearle AD. The role of preoperative patient characteristics on outcomes of total knee arthroplasty. J Arthroplasty. 2016; 31: 2617-2627.
- Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. Three groups of dissatisfied patients exist after total knee arthroplasty: early, persistent, and late. Bone Joint J. 2018; 100- B:161-169.
- 16. Longo UG, Ciuffreda M, Mannering N, D’Andrea V, Cimmino M, Denaro V. Patellar resurfacing in total knee arthroplasty. EFORT Open Rev. 2018; 3: 217-223.
- Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J. Better outcomes with patellar resurfacing during primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021; 29: 1130-1141.
- Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee osteoarthritis: a primer. Perm J. 2017; 21: 16-183.
- Dell’Isola A, Allan R, Smith SL, Marreiros SS, Steultjens M. Identification of clinical phenotypes in knee osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord. 2016; 17: 425.
- Kim KT, Lee S, Lee JI, Kim JW. Analysis and prediction of persistentpain after total knee arthroplasty. Knee. 2016; 23: 522-528.
- 21.Sullivan GM, Feinn R. Using effect size—or why the P value is not enough. J Grad Med Educ. 2012; 4: 279-82.
- Andrade C. The P value and statistical significance. Indian J Psychol Med. 2019; 41: 210-215.
- Singh JA, Lewallen DG. Hypertension is associated with increased risk of early revision after total knee arthroplasty. J Arthroplasty. 2017; 32: 2753-2757.
- Marchant MH Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am. 2009; 91: 1621- 1629.
- Goodman SM, Springer B, Guyatt G, et al. American College of Rheumatology/American Association of Hip and Knee Surgeons guideline for the perioperative management of antirheumaticmedication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. Arthritis Rheumatol. 2017; 69: 1538-1551.
- Nikiphorou E, Norton S, Young A, et al. The association of obesity with disease activity, functional ability and quality of life in early rheumatoid arthritis. Clin Rheumatol. 2016; 35: 225-231.
- Zhang Q, Dong J, Zhou D. Comparison of clinical outcomes between patellar resurfacing and non-resurfacing in total knee arthroplasty. Medicine (Baltimore). 2020; 99: e19440.
- Van Der Linden-Van Der Zwaag HMJ, Bos J, Van Der Heide HJL, Nelissen RGHH. A computed tomography study of the patellofemoral joint after total knee arthroplasty without patellar resurfacing. Int Orthop. 2018; 42: 2769-2776.
- Chen K, Li G, Fu D, et al. Patellar resurfacing versus nonresurfacing in total knee arthroplasty. Medicine (Baltimore). 2015; 94: e1850.
- Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement. J Bone Joint Surg Am. 2012; 94: 2270-2278.
- Migliorini F, Eschweiler J, Niewiera M, El Mansy Y, Tingart M, Rath B. Better outcomes after patellar resurfacing during primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021; 29: 1130-1141.
- Koh IJ, Lin CC, Patel NA, et al. Patellar resurfacing did not improve outcomes in patients with patellofemoral osteoarthritis. J Bone Joint Surg Am. 2020; 102: 1321-1328.
- Longo UG, Ciuffreda M, Mannering N, D’Andrea V, Cimmino M, DenaroV. Patellar resurfacing in total knee arthroplasty. EFORT Open Rev.2018; 3: 217-223.
- Watts CD, Wagner ER, Houdek MT, Osmon DR, Hanssen AD, Lewallen DG, et al. Morbid obesity: a significant risk factor for failure of two- stage revision total knee arthroplasty for infection. J Bone Joint Surg Am. 2014; 96: e154.
- Wagner ER, Kamath AF, Fruth K, Harmsen WS, Berry DJ. Effect of body mass index on reoperation and complications after total knee arthroplasty. J Bone Joint Surg Am. 2016; 98: 2052-2060.
- Chalidis BE, Tsiridis E, Tragas AA, Stavrou Z, Giannoudis PV. Management of periprosthetic patellar fractures. Injury. 2007; 38: 458-468.
- Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am. 2002; 84: 532-540.
- Koh IJ, Lin CC, Patel NA, et al. Patellar resurfacing did not improve outcomes in patients with patellofemoral osteoarthritis. J Bone Joint Surg Am. 2020; 102: 1321-1328.
- Jones CW, Jacobs H, Shumborski S, et al. Patellar resurfacing in primary total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty. 2021; 36: 1450-1458.
- Putman S, Boureau F, Girard J, et al. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019; 105: S43-S51.
- van Jonbergen HP, Werkman DM, van Kampen A. A randomised trial of patellar resurfacing in total knee replacement: ten-year results. Bone Joint J. 2020; 102-B: 587-592.
- Li S, Chen Y, Su W, et al. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2015; 39: 847-857.
- Sherman SL, Erickson BJ, Cvetanovich GL, et al. Patellofemoral kinematics and contact patterns in total knee arthroplasty. J Bone Joint Surg Am. 2017; 99: 497-503.
- Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality- of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017; 25: 2942-2951.
- Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014; 96-100.
- Alcerro JC, Rossi MD, Lavernia CJ. Primary total knee arthroplasty: clinical outcomes with contemporary surgical techniques. J Am Acad Orthop Surg. 2019; 27: 259-271.
- Dy CJ, Franco N, Ma Y, Mazumdar M, McCarthy MM, Gonzalez Della ValleA. Complications after patello-femoral versus total knee replacementin the treatment of isolated patello-femoral osteoarthritis. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012; 20: 2174-2190.
- Meijer MF, Reininga IH, Boerboom AL, Stevens M, Bulstra SK. Poorer survival after a primary implant during revision total knee arthroplasty. Int Orthop. 2013; 37: 415-419.
- van der List JP, Chawla H, Pearle AD. Why do patellae resurface in total knee arthroplasty? A review of the literature. J Knee Surg. 2016; 29: 398-412.
- Koh IJ, Lin CC, Patel NA, et al. Patellar resurfacing did not improve outcomes in patients with patellofemoral osteoarthritis. J Bone Joint Surg Am. 2020; 102: 1321-1328.