Application of the Fracture Risk in Orthopedic Emergency
- 1. Department of Orthopedics Emergency, Zhengzhou Central Hospital affiliated to Zhengzhou University, China
Abstract
Background: Orthopedic emergency for limb fractures is common. X-rays, CT scans, and MRI are helpful in diagnosing emergency fractures. However, these tests have their limitations. We hope to find some tools that can help us improve the detection rate of fractures.
Methods: We randomly assigned four orthopedic surgeons from the emergency department to two groups, the observation group used The Fracture Risk to detect fractures in patients, while the control group relied on The Fracture Risk, clinical experience, asking for medical history, and conducting detailed physical examinations to detect fractures in patients. We performed using SPSS Statistics version 25.0 on both the general information of the included patients and the accuracy of fracture detection using respective methods.
Results: The study included emergency orthopedic patients who were treated between March 1, 2023, and May 31, 2023. The accuracy rate was 77.27% in the observation group and 91.18% in the control group. However, there was no statistically significant difference in the accuracy rates for the four sites with higher fracture rates between the two groups.
Conclusions: The Fracture Risk can serve as a supplementary tool for orthopedic emergency physicians. A more accurate detection of fractures requires a combination of clinical experience, asking for medical history, and a thorough physical examination.
Keywords
• Application;
• Fracture Risk
• Detection
• Fractures Orthopedic
• Emergency
Citation
Li Y, Song J, Yao Z, Tang M (2025) Application of the Fracture Risk in Orthopedic Emergency. Ann Orthop Rheumatol 11(1): 1103.
INTRODUCTION
Orthopedic emergency is an important department in the emergency department of the hospital [1]. Our hospital is a tertiary hospital, and approximately fifty patients are treated in the orthopedic emergency department every day, including open skin injuries and closed injuries to limbs and the spine. For skin injuries, wound cleaning and suturing are performed. However, for limb injuries, we need to assess whether there is a fracture. Currently, the determination of fractures in patients mainly relies on clinical experience and detailed physical examination. Some patients may not exhibit typical fracture characteristics such as deformity, abnormal movement, which may result in misdiagnosis of fractures. Detailed physical examinations can cause severe pain for the patients, bringing them certain discomfort. Currently, the orthopedic emergency department of our hospital mainly relies on X-ray and CT examinations to detect fractures.
However, some trauma patients who receive pre-hospital emergency care lack access to X-ray equipment, and some special patients cannot undergo radiographic examinations, such as pregnant women [2], making it difficult to determine whether there is a fracture. Some literature reports have mentioned the application of emergency ultrasound in fractures, the integration with other imaging methods should always be considered in doubtful cases or for surgical planning [3]. The FRISK (Fracture Risk) – A New Tool to Indicate the Probability of Fractures”, two objective and one subjective factor that can be used to detect fractures in the ED: the anatomic region of injury, the age of the patient, and the response to functional questions, their goal of this study was to determine simple factors that could detect fractures in patients without the need for specialized personnel, transferring physician knowledge to an algorithm-based computer program can help optimize the emergency department workflow [4].
Hypothesis that this tool can also improve the accuracy of fracture detection for professional orthopedic doctors and provide assistance to emergency orthopedic physicians, we have decided to use this new tool in clinical practice.
METHODS
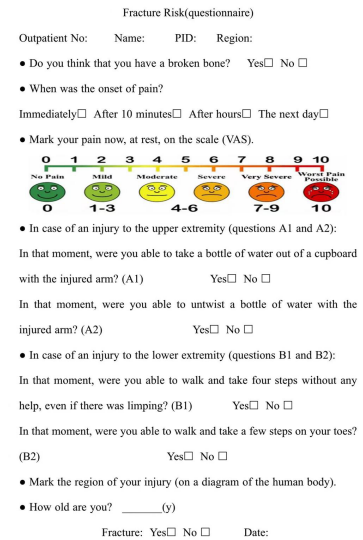
Four of our orthopedic emergency doctors have decided to start using The Fracture Risk in the orthopedic emergency department. First, we reviewed relevant literature on questionnaire design [5,6], and created a questionnaire based on The Fracture Risk (Figure 1). We randomly assigned four orthopedic surgeons from the emergency department to two groups, with two doctors in the observation group, and two doctors in the control group. The observation group used The Fracture Risk to detect fractures in patients, if the patients agree to participate in the study, we will register the patients on the questionnaire, while the control group relies on The Fracture Risk, clinical experience, detailed patient history taking (age, time of pain, high-energy or low-energy injury, etc.), and physical examination of patients (swelling extent, pain level, degree of deformity, range of motion, bone fricative) to detect the patient’s fracture. X-ray or CT scan was performed immediately in both groups of patients with suspected fractures, and the accuracy was determined based on the results of the radiological examinations.
Figure 1 Fracture Risk (questionnaire).
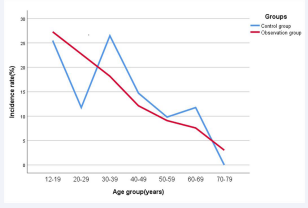
The study included patients who visited the orthopedic emergency department between March 1, 2023, and May 31, 2023. The inclusion criteria were patients over the age of 12 who could accurately describe the course of their illness (Figure 2), pregnant women, cognitive impairment, and patients with spinal injuries were excluded. Statistical analysis was conducted to compare the general information of the two groups of included patients and the accuracy of fracture detection. The IBM SPSS Statistics version 25.0 software package was used for statistical analysis of the data collected through the above-described procedures,quantitative data should be analyzed using t-test, while qualitative data should be analyzed using chi-square test. In all analyses, P < 0.05 with 95% confidence intervals was considered statistically significant. Since this study is a preliminary assessment of patients, the final diagnosis is based on X-rays and CT scans. The study was conducted in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. It was reviewed and approved by the Hospital Ethics Committee. Informed consent was obtained from all individual participants included in the study.
Figure 2 The graph shows the incidence rate of per age group in groups with increasing age (10-year increments).
RESULTS
A total of 168 patients presented to the orthopedic emergency department during the study period. Among them, there were 66 patients in the observation group and 102 patients in the control group. In the observation group, there were 34 males (51.52%), and 32 females (48.48%), with a mean age of 33.14 ± 2.14 (range, 12 to 72) years. The Fracture Risk test was used to detect fractures, with 51 cases correctly diagnosed, and 15 cases incorrectly diagnosed, resulting in an accuracy rate of 77.27%. In the control group, there were 50 males (49.02%) and 52 females (50.98%), with a mean age of 34.86 ± 1.67 (range, 12 to 68) years (Table 1).
Table 1: Information sheet for enrolled patients.
|
|
Observation group(n=66) |
Control group(n=102) |
|
Sex |
||
|
Male |
34 (51.52%) |
50 (49.02%) |
|
Female |
32 (48.48%) |
52 (50.98%) |
|
Age(min-max) (mean)years |
12-72(33.14) |
12-68(34.86) |
|
Region |
||
|
Hand |
8 (12.12%) |
21 (20.59%) |
|
Wrist |
6 (9.09%) |
10 (9.80%) |
|
Forearm shaft |
1 (1.52%) |
2 (1.96%) |
|
Elbow |
8 (12.12%) |
6 (5.88%) |
|
Humeral shaf |
1 (1.52%) |
1 (0.98%) |
|
Shoulder |
1 (1.52%) |
7 (6.86%) |
|
Hip |
2 (3.03%) |
2 (1.96%) |
|
Femur shaft |
1 (1.52%) |
3 (2.94%) |
|
Knee |
6 (9.09%) |
16 (15.69%) |
|
Tibia shaft |
3 (4.54%) |
7 (6.86%) |
|
Ankle |
19 (28.79%) |
14 (13.73%) |
|
Foot |
10 (15.15%) |
13 (12.75%) |
Fractures were detected based on experience and physical examination, with 93 cases correctly diagnosed, and 9 cases incorrectly diagnosed, resulting in an accuracy rate of 91.18%. There were no statistically significant differences in gender (p=0.752). There were no statistically significant differences in age (p=0.524), there was a statistically significant difference in the accuracy of fracture detection between the two patient groups (p=0.012), when analyzing the four high-incidence sites of fracture (hand, wrist, ankle, foot), there were no statistically significant differences in accuracy (Table 2).
Table 2: Statistical analysis table of variables for two groups.
|
|
Observation group |
Control group |
p-Value |
|
Sex |
|||
|
Male |
34/66(51.52%) |
50/102(49.02%) |
0.752 |
|
Female |
32/66(48.48%) |
52/102(50.98%) |
|
|
Age (mean±SD) years |
33.14 ± 2.14 |
34.86 ± 1.67 |
0.524 |
|
Accuracy rate(all %) |
77.27 |
91.18 |
0.012 |
|
Accuracy rate(ankle %) |
68.42 |
92.86 |
0.090 |
|
Accuracy rate(hand %) |
87.50 |
80.95 |
0.677 |
|
Accuracy rate(wrist %) |
66.67 |
90 |
0.247 |
|
Accuracy rate(foot %) |
80 |
76.92 |
0.859 |
DISCUSSION
Currently, X-rays, CT scans, MRI, and color Doppler ultrasound are helpful in diagnosing emergency fractures. However, these tests have their limitations. They can only be conducted in a hospital setting and require specialized technicians and equipment. Additionally, there are costs associated with these examinations. “The FRISK (Fracture Risk) – A New Tool to Indicate the Probability of Fractures”, they found three factors seem to be able to predict fracture risk: the injured region, the patient’s age, and a functional question. In this study, the prediction accuracy of The Fracture Risk for all fractures was 77.27%, fractures were detected based on experience and physical examination, resulting in an accuracy rate of 91.18%, among which the prediction accuracy of hand, wrist, ankle and foot were 87.5%, 66.67%, 68.42% and 80%. It is not possible to say whether the factor “age” or “region” is more important, in the observation group, the incidence decreased gradually with the increase of age, and the incidence of middle-aged and young patients was higher than that of elderly patients.
The energy received at the time of limb injury is a basis for us to judge fracture, and higher energy is more likely to cause fracture than lower energy injury, especially in middle-aged and young patients. Some elderly patients or fatigue fractures can be caused by low energy injuries. The characteristics of osteoporotic bone fractures, associated with minimal or moderate trauma, were evident in the population of females aged 65+ and to a lesser extent in males aged 65+. The fractures prevalent in the population aged 17- 64, both male and female, were high-energy fractures [7]. Features that distinguish a low-trauma from a high-trauma fracture event are inherently arbitrary, often described as a fracture that occurs spontaneously or with minimal force, the US National Osteoporosis Foundation (NOF) guidelines have noted that most fractures in older adults are due at least in part to low bone mass, even when they result from considerable trauma [8].
Pain is the main factor for patients to visit the hospital, and the degree of pain when the patient is injured is also a basis for judging whether the fracture occurs. The doctor should ask the time of pain after the injury. The fracture is generally accompanied by severe pain in the injured part, especially when the pain is aggravated when the affected limb is moved, accompanied by local obvious tenderness. Physicians should be aware that tenderness in the anatomical snuff box (ASB), tenderness over the scaphoid tubercle and pain on longitudinal compression of the thumb have limited added value in a diagnostic process for a scaphoid fracture [9]. History taking and physical examination are important tools in a diagnostic process of diagnosing patients with wrist pain. The degree of swelling can also be used as a reference for judging fracture. Limb injury may be accompanied by local soft tissue injury, resulting in local swelling. Fracture may lead to severe swelling of the affected limb, and even tension blisters and subcutaneous ecchymosis. Local swelling and pain may limit the movement of the affected limb, and in the case of a complete fracture, it can result in the complete loss of functional activity in the injured limb. Displacement of the broken end of the fracture may result in a change in the shape of the affected limb, which may be manifested as shortening, angulation, or rotational deformity. Bone chafing sensation is produced when the broken ends of both sides of the fracture rub against each other, and is the exclusive sign of the fracture. However, some fractures, such as avulsion fractures and incomplete fracture, do not have typical fracture-specific signs.
Orthopedic emergency, as an important department of the emergency department, sees a lot of patients with limb injuries every day. As a tertiary hospital, our orthopedic emergency department treats approximately 50 patients daily. These patients are initially assigned to the orthopedic emergency department for physical examination and preliminary diagnosis, and those with suspected fractures undergo X-ray, ultrasound, or CT scans. Currently, our preliminary judgment of whether a patient has a fracture mainly relies on clinical experience and physical examinations. The Fracture Risk is not only suitable for non-professionals in predicting fractures, but it also serves as a good complement for orthopedic professionals in the detection of fractures. However, some fractures do not have typical signs, so we can only rely on the injury mechanism, degree of swelling, pain score, and range of motion of the injured limb to determine the presence of a fracture. These judgments are subjective and require orthopedic emergency clinical experience. We also consulted some literature, including literature on the evaluation of hand, wrist, elbow, shoulder, hip, knee, ankle, and foot bone fractures, hoping to find some objective tools for detecting fractures to help improve our accuracy in diagnosing fractures.
The application of X-rays for diagnosing fractures has been widely used in hospitals at all levels. Plain X-ray continues to be the first and often the only technique necessary [10], with different projections required for assessing fractures in different body regions. Pinto et al. pointed out in their study that while radiographs remain the mainstay for fracture assessment, some non-displaced and subtle fractures may be radiographically occult [11]. In the case of high clinical suspicion for fracture in one of these bones, computed tomography (CT) should be strongly considered in the presence of a normal plain radiograph [12]. Evaluation of malleolar fractures by X-ray only inevitably results in the overlooking of many pathologies, routine CT scans can help improve the accuracy of diagnosis [13]. Addala TE et al., reported that ULD-CT appears a reliable alternative for digital radiographs for detection of fractures of the extremities in the emergency room with a good sensitivity and specificity [14]. Ultrasound is commonly used in pediatric orthopedic emergency to avoid radiation exposure to children. David Troxler et al. reported that POCUS for diagnosing upper extremity fractures in children proved as sensitive as standard X-ray imaging and was significantly faster and less painful [15].
With the development of artificial intelligence, it has been applied to the diagnosis of emergency fractures. AI assistance improved the sensitivity and may even improve the specificity of fracture detection by radiologists and nonradiologists [16]. The optimized AI model improves the diagnostic efficacy in detecting extremity fractures on radiographs, and the optimized AI model is significantly better than radiologists in detecting avulsion fractures, which may be helpful in the clinical practice of orthopedic emergency [17]. Holly Gil et al., reported that implementation of an MRI scanner for dedicated emergency department use enables faster hip fracture diagnosis and surgical consultation, or definitive disposition without increasing ED throughput time [18].
CONCLUSIONS
The Fracture Risk provides a good alternative for detecting fractures, as it is easy to use and not limited to professionals. It can serve as a supplementary tool for orthopedic emergency physicians. To achieve better fracture detection, it is necessary to combine clinical experience, asking for medical history, and detailed physical examinations. The limitations of this study include being a single-center study with a relatively short duration of patient data collection (3 months). Further time and experience are needed to assess the reliability of this tool.
AUTHOR CONTRIBUTIONS
All authors contributed to the study conception and design. Data collection by Li, Song, Yao and Tang. Analysis and the first draft of the manuscript was written by Yafeng Li. All authors commented on previous versions of the manuscript, and read and approved the final manuscript.
REFERENCES
- Bond MC, Sayal A. Orthopedic Emergencies. Emerg Med Clin North Am. 2020; 38: xv-xvi.
- Happel C, Borowski M, Kamp A, Rudolf F, Wicke JH, Gröner D, et al. Pränatale Strahlenexposition aus nuklearmedizinischer Indikation [Prenatal Radiation Exposure in Nuclear Medicine]. Nuklearmedizin. 2021; 60: 233-239.
- Cocco G, Ricci V, Villani M, Delli Pizzi A, Izzi J, Mastandrea M, et al. Ultrasound imaging of bone fractures. Insights Imaging. 2022; 13: 1894.
- Wichlas F, Hahn FM, Tsitsilonis S, Lindner T, Marnitz T, Deininger C, et al. The FRISK (Fracture Risk)-A New Tool to Indicate the Probability of Fractures. Int J Environ Res Public Health. 2023; 20: 1265.
- Ferreira ÁRS. Some considerations for creating a researchquestionnaire. Rev Col Bras Cir. 2020; 47: e20202895.
- Shelley A, Horner K. Questionnaire surveys - sources of error and implications for design, reporting and appraisal. Br Dent J. 2021; 230: 251-258.
- Pavi? R, Hnatešen D, Margeti? P. Epidemiology of Adult Fractures in Eastern Croatia by Cause of Injury, Fracture Location and Type of Treatment. Acta Clin Croat. 2017; 56: 494-504.
- Leslie WD, Schousboe JT, Morin SN, Martineau P, Lix LM, Johansson H, et al. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int. 2020; 31: 1059-1067
- Krastman P, Mathijssen NM, Bierma-Zeinstra SMA, Kraan G, RunhaarJ. Diagnostic accuracy of history taking, physical examination and imaging for phalangeal, metacarpal and carpal fractures: a systematic review update. BMC Musculoskelet Disord. 2020; 21: 12.
- Blanco-Barrio A, Moreno-Pastor A, Lozano-Ros M. Fractures of the limbs: basic concepts for the emergency department. Radiologia (Engl Ed). 2023; 65: S42-S52.
- Pinto A, Berritto D, Russo A, Riccitiello F, Caruso M, Belfiore MP, et al. Traumatic fractures in adults: missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed. 2018; 89: 111-123.
- Wedmore I, Young S, Franklin J. Emergency department evaluation and management of foot and ankle pain. Emerg Med Clin North Am. 2015; 33: 363-396.
- Szyma?ski T, Zdanowicz U. Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures-How much do we miss? Foot Ankle Surg. 2022; 28: 263-268.
- Addala TE, Greffier J, Hamard A, Snene F, Bobbia X, Bastide S, et al. Early results of ultra-low-dose CT-scan for extremity traumas in emergency room. Quant Imaging Med Surg. 2022; 12: 4248-4258.
- Troxler D, Sanchez C, de Trey T, Mayr J, Walther M. Non-Inferiority of Point-of-Care Ultrasound Compared to Radiography to Diagnose Upper Extremity Fractures in Children. Children (Basel). 2022; 9: 1496.
- Guermazi A, Tannoury C, Kompel AJ, Murakami AM, Ducarouge A, Gillibert A, et al. Improving Radiographic Fracture Recognition Performance and Efficiency Using Artificial Intelligence. Radiol. 2022; 302 :627-636.
- Liu Y, Liu W, Chen H, Xie S, Wang C, Liang T, et al. Artificial intelligence versus radiologist in the accuracy of fracture detection based on computed tomography images: a multi-dimensional, multi-region analysis. Quant Imaging Med Surg. 2023; 13: 6424-6433.
- Gil H, Tuttle AA, Dean LA, Johnson DA, Portelli D, Baird J, et al. Dedicated MRI in the emergency department to expedite diagnostic management of hip fracture. Emerg Radiol. 2020; 27: 41-44.