Can bedside knee joint washout help treat septic arthritis?
- 1. Department of Internal Medicine, University of Michigan Health System Michigan
Abstract
Drainage of joint purulence is a critical component in the management of septic arthritis. Methods from arthrocentesis to open arthrotomy and arthroscopy are mainstays, with different efficacies and morbidities. Percutaneous tube instillation techniques have been employed since World War I. Methods to effect joint distension and irrigation to mimic what is accomplished at arthroscopy employed over the past
50 years have been honed to a simple bedside technique since the 80s and applied successfully in management of septic arthritis. Wider employment of this technique has the potential to improve efficacy of septic arthritis treatment, particularly when access to O.R. based procedures is limited.
Citation
Ike RW (2021) Can bedside knee joint washout help treat septic arthritis? Ann Orthop Rheumatol 8(1): 1097.
INTRODUCTION
The time-honored principles in acute septic arthritis management involve the prompt and most thorough drainage of joint purulence possible [1,2]. The benefits of the washout have been displayed in the lab from reports of a lapine model of septic arthritis which displayed reduced cartilage loss among animals whose infected knees were washed out [3]. In the development stages of surgical arthroscopy, it became evident that the procedure would attain similar goals as the more invasive open arthrotomy [4]. Additionally, the more benign outcome achieved through arthroscopy was bolstered by a review of NHS data [5].
In recent times, using quick arthroscopic washout in the case of a septic knee is viewed and adopted as standard care [5]. How often the intervention is adopted [6,7] and if it happens at all [8,9] remains an issue of discussion. The barriers to arthroscopy have increasingly been reduced through the minimal use of anesthesia and increased performance of arthroscopy in an office or procedure room compared to when it was strictly in an operating room procedure.
METHODS
Search of the literature using Web of Science, Scopus, and PubMed using terms “septic arthritis” OR “infectious arthritis” AND “lavage” OR “irrigation” OR “drainage” OR ”washout” OR “arthroscopy” generated references not already in the author’s library.
DISCUSSION
Application of arthroscopy to the septic knee is not always possible. In the U.K., during the COVID pandemic, the British Orthopedic Association (BOAST) issued guidelines that medical treatment composed of closed-needle aspiration and antibiotic therapy needed to be given to patients as first-line management. The operative treatment that involved arthroscopic joint washout +/- synovectomy was reserved for patients with sepsis signs, thus effectively reducing the exposure of infected patients to the O.R. environment [10]. Countries and communities with limited resources do not have the privileges of taking quick trips
to O.R. from arthroscopic washout, as they lack multiple facets of orthopedic service, including arthroscopic expertise [11].
Before the widespread use of arthroscopy, different techniques to wash out the septic joint had been addressed. During the First World War, carbolic acid, magnesium sulfate solution or boric acid was reported to be effective even before the discovery of antibiotics, let alone arthroscopy [12]. The intraarticular tube installation was developed to deliver antibiotics and detergents and was not consistently effective [13]. In this
regard, Bob Jackson recognized the inherent limitations to the technique; thus, he incorporated slow distension of the joint regulated by the patient together with cycled evacuation to suction that continued for 8 to 10 days [14]. In this case, the results were highly effective compared to those treated with “drip drain”; thus, Jackson described it as a highly effective strategy for synovial purulence removal. There has been a description of other methods to enhance drainage of the infected joints without the need to use conventional surgical methods. The described methods include the placement of a continuous irrigation tube
in a septic knee employing reduced arthroscopic guidance [15] and the use of an irrigating catheter (into septic hips) under radiographic guidance and general anesthesia [16]. Additionally, there is the fluoroscopic guidance of a pigtail catheter method that is attached to enhance the low-suction reservoir [17]. The different strategies have not attained widespread acceptance as adjunctive measures to improve the effective management of septic arthritis.
Bob Jackson published the first description of arthroscopy to manage and treat septic knees. The publication covered no longer pursued practices such as prolonged post-op suction drainage and detergent [18]. A recent analysis of management of the septic knee does not mention adjunctive interventions but describes the arthroscopy and washout [4].
The interventions to drain joints among children and medically unstable patients are characterized by puncture of the joints and flow-through of irrigant as in the case of joint washout [19]. A report in the 90s presented the adoption of bedside washout among patients managed with the older model of repeated closed aspirations; patients who got to the point of referral for surgical drainage due to incomplete evacuation of the joints, impossibility of resolving synovial leukocytosis, extending of local infections or in cases where sepsis was done bedside washout and 4/11 avoided cases of surgical therapy [20]. Griffet
et al. described the placement of pleurocath or cystocath in the case of children with septic arthritis to enable the entry of saline for washout, drainage or gravity drainage. The washout apparatus were removed after an average of 5-9 days after it was evident that clinical improvement was attained [21]. Yassa et al. presented a strategy of washing out a child’s septic shoulder using two large-bore cannulae placed anteriorly to enable saline inflow and exit to suction. In this case, he did not mention the fluid volume in the shoulder, but mentioned the manipulation of the shoulder, and cannulae are not left in place [22]. Johnson et al. described the “no hands” approach adopted during arthroscopy but did not utilize an arthroscope. In this case, an inflow cannula and an arthroscope are put in the joint, but the sterile glove’s
finger covers the arthroscope to enhance inflow and egress [23]. Ateschrang et al. created a system and tested it using a cadaver, but it has not been documented if it was used medically. The
saline was infused and removed using a separate cannullae while an electronic pump was used to regulate the flow rate, dwell time and intra-articular pressure [24]. In the case of Khoo, he used a two canunula system placed at the bedside the same way as the French technique [25] and kept it in place for four days [26]. Bunting and Kuper experienced a successful washout of a septic shoulder in an emergency room after it was declared that the patient condition was beyond an operative intervention. In this case, 16 gauge angiocaths were inserted with ultrasound guidance, thus allowing ingress and saline exit that delivered a clear effluent of 3 liters [27]. Yasheng et al. informed amelioration of osteomyelitis after a washout with ozonated water [28]. The medullary bone was washed out contrary to the joint, and this approach demonstrated the potential of augmenting impacts of washout through the liquid used. Additionally, the approach hinted at a new intervention for osteoarthritis, where efficacy was reported while adopting intra-articular injection of ozone [29].
Joint washout is an important intervention for septic arthritis regardless of the technique or approach adopted. The details of the procedure performance that include volume and type of washout fluid, post-lavage and additives remain to be addressed, and their difference is dependent on the clinical scenario. Washout can be accomplished without the challenges associated with access, expertise and costs that govern O.R-based procedures. Using this procedure in countries with limited resources where the barriers are factual and high could improve the management of septic arthritis in the regions [30]. Low expectations characterize septic arthritis treatment in areas with limited resources, and amputation avoidance is considered a victory [31].
PERFORMING JOINT WASHOUT
Bedside joint washout can be accomplished by any physician proficient in arthrocentesis [32]. Washout can be performed with 2 cannulae, as in France [32], or by the single entry method – once called “tidal irrigation” - we have always employed. We believe this provides a more thorough washout as inflowed fluid cannot exit out a pressure gradient before filling the joint and the instillation causes some capsular distension. Initial steps are same as those for arthrocentesis: a comfortably supine patient, appropriate skin anesthesia (with some extra infiltrated in anticipation of a larger bore needle), joint penetration with
removal of any fluid, followed by intraarticular instillation through same needle of 10 ml bupivacaine. After this, things become more specialized. A needle of around 14 gauge (2mm) – whether a Vere’s needle, sterilized cow teat cannula, or plain 14 g needle [Figure 1]
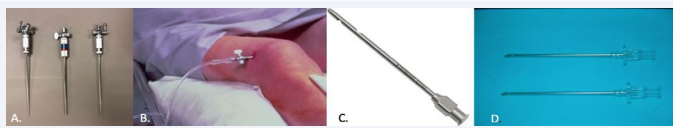
Figure 1: Technique of joint washout I. Needles. A. 14 g Verres needle, 3 different brands. B. knee being washed out through Verres needle connected to irrigation tubing. 30-60 mL aliquots of saline are instilled into joint, then removed and repeated until at least a liter passes through. C. cow teat cannula, 14 g, suitable for use as washout needle. D. 2 mm cannulae favored by French rheumatologists (courtesy of X. Ayral, Paris). Reproduced from reference 32, with permission.].
- is used to penetrate the joint. The hub of the needle is connected to the male end of the tube of the assembly that will convey washout fluid in to and out of the joint [Figure 2]
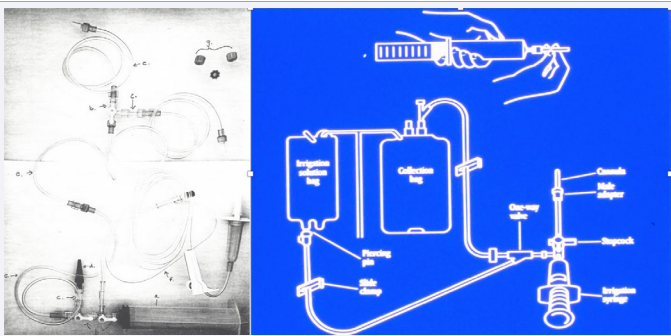
Figure 2: Technique of joint washout. Fluid connections. A. “homemade” kit, utilizing off-the-shelf items. a. 60 cc syringe, b. 3 way stopcock, c. double male luer adapter, d. “Christmas tree” adapter, e. connecting tubing, f. bag spike with macrodripper and tubing, g. screw capsB. “Tidal irrigation” kit developed and vended by Abbott Labs (Abbott Park, IL), used in trial described in ref 33, no longer sold). Reproduced from reference 32, with permission.
30 – 60 ml fluid is instilled into the joint, 3 way stopcocks then adjusted to direct effluent to a tube connected to a collection bag or suction. The process is repeated until the infusion bag is
empty, whether starting at 1 L or 3 L.[33] The entire process takes about 30 minutes. Glucocorticoid or hyaluronate can be instilled as desired. A Steri-Strip is adequate for closure and the patient is immediately ambulatory, with the usual instructions regarding post-injection activity (102). In the United States, no specific billing code exists for washout, so billing is submitted for “miscellaneous knee procedure” with documentation.[34]
CONCLUSION
The simple and safe technique of bedside knee washout can be applied as a method to drain joint purulence in septic arthritis and could supplant more extensive drainage procedures and substitute for them where for various factors they may not be available.
REFERENCES
12. Carline WA. The drainage of septic knee joints. Br Med J. 1917; 1: 294- 295.
18. Jackson RW. The septic knee--arthroscopic treatment. Arthroscopy. 1985; 1: 194-197.
25. Ayral X & Dougados M. Joint lavage. Rev Rhum Engl Ed. 1995;62: 281- 287.
32. Ike RW. How to wash out a knee. J Biomed Res Environ Sci (in press)








































































































































