Bronchiolitis Obliterans in an Infant with Multi Drug Resistant Pulmonary Tuberculosis - Do Not Forget Respiratory Syncytial Virus Co-Infection
- 1. Department of Pediatric Infectious Diseases, Bai Jerbai Wadia Hospital for Children, India
- 2. Grant Government Medical College, India
Abstract
A 14-month-old boy with multi-drug resistant (MDR) pulmonary tuberculosis (PTB) on moxifloxacin, paraaminosalicylate (PAS), clofazimine, linezolid and cycloserine since 5 months of age had fever and cough for 3 days, increased respiratory activity for 2 days and generalized erythematous rash over body for a day. CT chest showed areas of air trapping in bilateral upper and lower lobe lung parenchyma suggestive of bronchiolitis obliterans. Nasopharyngeal aspirate multiplex PCR for respiratory panel was positive for respiratory syncytial virus (RSV). He was treated with oral ribavirin, steroids and high flow nasal cannula (HFNC). This case highlights the rarity of such co-infections and highlights that not all worsening of PTB is treatment failure and one should always keep in mind co-infections with other respiratory pathogens.
Keywords
• Respiratory syncytial virus (RSV)
• Pediatric Tuberculosis
• Steroids
CITATION
Joshi M, Jain S, Shah I (2023) Bronchiolitis Obliterans in an Infant with Multi Drug Resistant Pulmonary Tuberculosis - Do Not Forget Re spiratory Syncytial Virus Co-Infection. Ann Pediatr Child Health 2023; 11(5): 1321.
INTRODUCTION
Multi-drug resistant (MDR) pulmonary tuberculosis (PTB) continues to pose a global health challenge, especially among vulnerable populations like children [1]. Respiratory syncytial virus (RSV) is a common cause of pneumonia in infants and young children [2]. It is worth noting that children under 5 years old bear the highest burden not only of tuberculosis (TB) but also of other acute non-TB respiratory tract infections. However, there is limited information available on the prevalence of respiratory virus co-infections in children suspected of having PTB [3]. To the best of our knowledge, we present the first reported case of a child with MDR PTB concurrently infected with RSV. This case highlights the rarity of such co-infections and underscores the need for heightened awareness and vigilance in managing such a scenario.
CASE SUMMARY
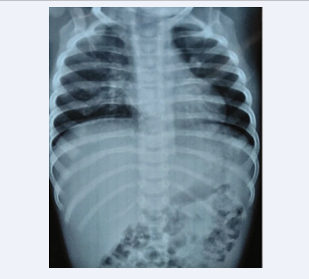
A 14-month-old boy with MDR-PTB on moxifloxacin, paraaminosalicylate (PAS), clofazimine, linezolid and cycloserine since 5 months of age had fever and cough for 3 days, increased respiratory activity for 2 days and generalized erythematous rash over body for a day. On admission, child was pale, weight was 6.8 kg (<-3SD as per World Health Organization (WHO) growth charts), length was 43.5 cm (< 3SD as per WHO growth charts), respiratory rate was 56/min and oxygen saturation was 91% on oxygen by prongs at 4L/min. There was decreased air entry on right side of chest with bilateral wheeze and hepatosplenomegaly. He was put on high flow nasal cannula (HFNC). Investigations showed hemoglobin 11.5 g%, white cell count 28350/mm3 (60% polymorphs, 32.8% lymphocytes), platelets 345,000 cells/cumm and ESR of 54 mm at end of 1 hour. C reactive protein (CRP) was 119 mg/L. HIV ELISA was negative. X-ray chest had bilateral infiltrates. (Fig 1)
Figure 1: X-ray chest showing bilateral infiltrates.
CT chest showed areas of of air trapping in bilateral upper and lower lobe lung parenchyma suggestive bronchiolitis obliterans. Nasopharyngeal aspirate multiplex PCR for respiratory panel was positive for respiratory syncytial virus (RSV). He was investigated for other immunodeficiencies - Nitroblue tetrazolium test (NBT) 95% burst cells (normal: 95-100%), and dihydrorhodamine test(DHR)- 95% (Normal range: 95-100 %) test were normal. Lymphocyte subset analysis (LSSA) showed Cd3-/Cd19+ of 635 (7%) cells/cumm (Normal range 390-1400 cells/cumm), Cd3+/ Cd19- cells of 8074 (89%) cells/cumm (Normal range 1400-3700 cells/cumm) and CD16/56 of 272 cells/cumm (Normal range 130-720 cells/cumm). Patient was treated with budesonide and salbutamol nebulization and oral ribavirin at 15 mg/kg/day for 10 days. Intravenous Methylprednisolone was given at 2 mg/kg/ day for 5 days followed by prednisolone at 1 mg/kg/day for 4 days and subsequent tapering over 3 months. Meanwhile, ATT was continued. Gradually, the child was switched to nasal CPAP, tapered to oxygen by prongs and lastly on room air in 5 days. On follow up, he maintains an oxygen saturation of 95-98% on room air, his ATT has been stopped after 18 months of therapy and he is on budesonide metered dose inhaler. He is currently 2 ½ years old and weighs 9 kg.
DISCUSSION
The treatment of MDR-PTB in children requires an individualized and comprehensive approach, considering factors such as the child’s age, drug susceptibility, and potential drug interactions [4]. In our case, the 14-month-old patient had been receiving a tailored combination of Moxifloxacin, PAS, Clofazimine, Linezolid, and Cycloserine since the age of 5 months.
Patients with PTB may develop ancillary lung infections [3]. These infections are mostly bacterial, and less frequently fungal [3]. For recently discovered PTB, Klebsiella pneumoniae is found to be the most prevalent secondary bacterial infection [3]. In addition, viruses may also contribute to the development, manifestation, and progression of PTB in children by interfering with the host’s immune system [3,5]. Our patient presented with RSV coinfection.
Young children face a significant threat of illness and death due to severe RSV disease. The risk of severe RSV disease is higher in children with certain underlying conditions like premature birth (with or without bronchopulmonary dysplasia), congenital heart disease, immunosuppression, or respiratory conditions such as cystic fibrosis [6]. Factors such as overcrowding, childcare center attendance, and exposure to second-hand smoke can also increase the likelihood of developing a severe RSV infection [6]. Our patient had MDR-PTB.
At present, there are no definitive curative treatments for severe RSV disease, and the available options mainly revolve around providing supportive care [7].This includes providing adequate hydration, supplemental oxygen, airway suctioning, and mechanical ventilation if necessary. Ribavirin, an antiviral drug, is the only licensed therapy for RSV, but its use is limited to severe cases in immunocompromised patients due to concerns about toxicity, safety, and the inconvenience of administration via aerosol route [8]. Our patient was already on linezolid and there were concerns of using oral ribavirin in our patient due to risk of anemia. However, due to non-availability of inhaled ribavirin, he was given oral ribavirin with monitoring of his hemoglobin. Also due to bronchiolitis obliterans, he needed steroids to control his hypoxia which was also used with caution to a minimum dose possible to prevent worsening of his MDR PTB. Inspite of that, he needed systemic steroids for 3 months to maintain his oxygen saturation with switch to inhaled steroids after that. He completed 18 months of ATT and did not have worsening of PTB inspite of steroids highlighting the fact that steroids have to be used very judiciously in patients with PTB and bronchiolitis obliterans.
REFERENCES
5. Anila Jose, Vedavathi R, Preethi R Gandhi, Tharuni Latha.A, Hilas, Vijaykumar SS. Study of Secondary Lung Infections in Newly Diagnosed Pulmonary Tuberculosis. J Med Sci Clin Res. 2019; 7: 482 487.