Caregiver Attitude toward COVID-19 Vaccine in an Urban Children
- 1. Carman and Ann Adams Department of Pediatrics, Central Michigan University, USA
- 2. Carman and Ann Adams Department of Pediatrics, Michigan State University School of Osteopathic Medicine, USA
- 3. Department of Sociology, Wayne State University, USA
- 4. Department of Pediatrics, Ohio State University College of Medicine, USA
Abstract
Background: Control of the coronavirus 2019 disease (COVID-19) pandemic is reliant upon vaccination of a large percentage of the global population. Low rates of vaccine acceptance hinder these efforts. In May 2021, the US Food and Drug Administration granted Emergency Use Authorization for the COVID-19 vaccine in children ≥ 12 years of age. Our study objective was to assess vaccine acceptance among caregivers of children ≤ 18 years in an urban free-standing children’s hospital and factors associated with vaccine hesitancy.
Study Design: Cross sectional Survey.
Methods: We conducted a cross-sectional survey of parents/caregivers of children <18 years of age regarding attitude towards COVID 19 vaccine. We collected: demographic information, immunization status of the child, history of COVID-19 in the family, and intention to receive the COVID-19 vaccine for parent and child. The association of demographic variables and caregiver vaccine hesitancy was examined using a multinomial logistic regression for vaccine hesitancy.
Results: We noted a high rate (74.2%) of COVID 19 vaccine hesitancy in caregivers. Although acceptance of COVID-19 vaccination for children was higher in caregivers whose child was up-to-date on routine immunizations, received seasonal influenza vaccination and those who had received COVID-19 vaccination themselves, the overall acceptance rate was still low. Caregivers who identified as African American and mothers were more likely to express vaccine hesitancy while those with children>10 years and higher education levels were more likely to express vaccine acceptance.
Conclusions: A high rate of COVID-19 vaccine hesitancy and refusal for children was noted in our urban cohort. While African American caregivers and mothers were more likely to express vaccine hesitancy, older age of children and higher parental education levels were associated with vaccine acceptance. Targeted interventions are needed to improve COVID 19 vaccine uptake rates in children particularly in the African American community
Keywords
Caregivers, COVID-19 vaccine, Hesitancy, Children
Citation
Kannikeswaran N, Leja J, Pitman-Hunt C, Sethuraman U, Merolla DM, et al. (2023) Caregiver Attitude toward COVID-19 Vaccine in an Urban Children’s Hospital. Ann Pediatr Child Health 2023; 11(3): 1310.
INTRODUCTION
While the majority of pediatric Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infections have been asymptomatic or mild, about 1 in 3 children hospitalized with Corona Virus Disease 2019 (COVID-19) require intensive care [1]. Severe manifestations of COVID-19 in children include respiratory failure, Multisystem Inflammatory Syndrome in Children (MIS-C), acute renal and multi organ failure. In May 2021, the COVID-19 vaccine was authorized for emergency use in children ≥ 12 years [2].The Centers for Disease Control and the American Academy of Pediatrics have strongly advocated for widespread vaccination in children to protect them against infection and severe illness as well as aid in promoting return to in-person school [3,4]. In addition, vaccinations in children is being recommended to protect the community by decreasing the circulation of virus to unvaccinated adults and reduce development of mutant strains [5]. However, data are sparse regarding COVID-19 vaccine acceptance for children among caregivers.
Vaccine implementation strategies are complicated by disparities in disease severity and vaccine uptake in specific patient populations. Racial and ethnic minority children have been shown to have lower rates of testing and be disproportionately impacted by COVID-19 disease with higher rates of hospitalization, severe illness and death [6,7]. Despite this, higher rates of COVID-19 vaccine hesitancy have been reported in these racial and ethnic minority communities [8- 10]. For example, the city of Detroit, Michigan has a large African American community with a high COVID-19 disease burden. However, despite this, the city has one of the lowest reported rates amongst adults for vaccination against COVID-19 [11]. This makes it critical to understand factors that impact vaccine acceptance in this population. The objective of our study was to evaluate caregiver attitudes toward COVID-19 vaccination in a tertiary care children’s hospital in Detroit and possible factors associated with vaccine hesitancy.
METHODS
We administered a cross sectional survey (supplement 1) to a convenience sample of caregivers of children ≤18 years of age who presented to the Emergency Department or the radiology suite at an inner city, children’s hospital between April 1st 2021 to May 30, 2021. Caregivers were provided a study information sheet including the right to refuse or withdraw participation prior to survey adminsitration. The following data were collected: demographic information, immunization status of the child, history of COVID-19 in the family, and intention to receive the COVID-19 vaccine for parent and child. Reasons for no/ unsure answers were solicited via multiple choice selections and free text. Caregivers had the option of selecting more than one response as reasons for their hesitancy for COVID-19 vaccine. We defined vaccine hesitancy as responses marked “no” and/or “unsure”.
Descriptive statistics were used to describe the study cohort. We examined the association of child immunization status, influenza vaccine status and caregiver COVID-19 vaccine status with vaccine hesitancy using three cross-tabulations and a chi-square test. The association of demographic variables and caregiver vaccine hesitancy was examined using a multinomial logistic regression for vaccine hesitancy. The significance level was set to an alpha 0.05, and 95% confidence intervals are provided for all relevant point estimates. The study was approved as an expedited review by our Institutional Review Board (#2020-1614).
RESULTS
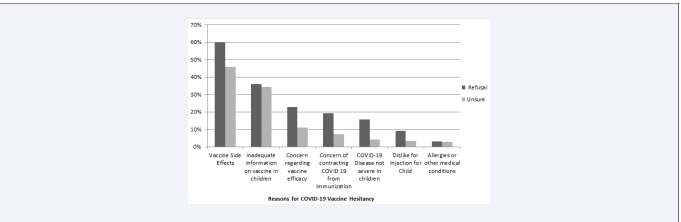
A total of 565 caregivers were approached for the study, 66 (11.7%) of whom refused participation. Among the 499 surveys distributed, 26 (5.2%) were incomplete and hence were excluded, leaving 473 surveys eligible for analysis. Study cohort demographics are shown in Table 1. Slightly over one -half of the caregivers (264; 55.8%) identified themselves as African American and had less than a college degree (275; 58.1%). Nearly two-thirds of the respondents (311; 65.8%) had experienced COVID-19 illness in their family. We found a high rate of COVID-19 vaccine refusal (n= 167; 35.3%,) and hesitancy (unsure; n= 184; 38.9%) in our study cohort. Reasons for vaccine hesitancy are shown in Figure 1. The top three reasons for vaccine hesitancy included, a) concerns regarding side effects (52.4%), b) inadequate data on children (35%), and c) concerns regarding vaccine efficacy (16.5%).
Figure 1: Reasons for COVID-19 Vaccine Hesitancy for Children amongst Caregivers.
Although acceptance of COVID-19 vaccination for children was higher in caregivers whose child was up-to-date on routine childhood immunizations, received seasonal influenza vaccination and those who had received COVID-19 vaccination themselves (Table 2);
Table 1: Demographics and characteristics of study participants (n=473)
| n (%) | |
| Characteristics | |
| Child Gender* | |
| Female | 240 (50.7) |
| Race* | |
| White | 161 (34) |
| Black | 264 (55.8) |
| Asian/Pacific Islander | 9 (1.9) |
| Other | 21 (4.2) |
| Child Age* | |
| Less than 6 months | 35 (7.4) |
| 6-23 Months | 59 (12.5) |
| 2-5 Years | 99 (20.9) |
| 6-10 Years | 111 (23.5) |
| >10 Years | 139 (29.4) |
| Caregiver Type | |
| Mother | 372 (78.6) |
| Caregiver Education* | |
| Less than 8th Grade | 49 (10.4) |
| High School Graduate | 170 (35.9) |
| Trade/Technical School | 56 (11.8) |
| Associates Degree | 73 (15.4) |
| Bachelor’s Degree | 44 (9.3) |
| Post-Graduate Degree | 42 (8.9) |
| Child Comorbidity* | |
| Yes | 169 (35.7) |
| No | 302 (63.8) |
| Family Experience with COVID19 | |
| Yes | 311 (65.8) |
| No | 162 (34.2) |
* Child gender not recorded in 1 survey
* Race not recorded in 5 surveys and 15 caregivers preferred not to answer
* Age group not recorded in 30 surveys
* Caregiver education not recorded in 42 surveys
* Child Comorbidity not recorded in 2 surveys
the overall acceptance rate was still low. Notably, only 29.9% of caregivers favoring routine childhood vaccinations and 47.6% of caregivers who favored seasonal influenza vaccines were accepting of the COVID19 vaccine for their children. Among caregivers who accepted COVID-19 vaccine for themselves, only 58.6% accepted the vaccine for their child (Table 2).
Table 2: Caregiver attitudes regarding COVID-19 vaccination for children by child and caregiver immunization status (N=473)
Notes: Results from three separate cross tabulations; ***p<.001.
Multinomial logistic regression analysis of factors associated with COVID-19 vaccine hesitancy and refusal showed that African American caregivers and mothers were more likely to express COVID-19 vaccine hesitancy and refusal, while caregivers with children age >10 years and those with an associate’s degree or higher were less likely to express hesitancy and refusal (Table 3).
Table 3: Multinomial logistic regression of factors associated with child COVID-19 vaccine hesitancy in caregivers (n=401)a
| No vs. Yes | Unsure vs. Yes | |||||
| OR | CI | p | OR | CI | p | |
| Child Gender | ||||||
| Female Child (REF) | ||||||
| Male Child | 1.359 | .786-2.351 | 0.273 | 1.153 | .682-.1.948 | 0.595 |
| Race | ||||||
| Not Black (REF) | ||||||
| Black | 2.319 | 1.323-4.063 | 0.003 | 2.013 | 1.178-3.438 | 0.01 |
| Child Age | ||||||
| Under 6 Years (REF) | ||||||
| 6 Years and Older | 0.368 | .205-.661 | <.001 | 0.402 | .228-.709 | 0.002 |
| Caregiver Education | ||||||
| Less than Associate degree (REF) | ||||||
| Associates or Higher | 0.481 | .273-.848 | 0.011 | 0.641 | .376-1.092 | 0.102 |
| Caregiver Relationship to Child | ||||||
| Not Mother (REF) | ||||||
| Mother | 2.253 | 1.180-4.299 | 0.014 | 1.993 | 1.092-3.637 | 0.025 |
| Child Comorbidity b | ||||||
| No/Did not Answer (REF) | ||||||
| Yes | 0.724 | .411-1.277 | 0.265 | 0.837 | .489-1.432 | 0.515 |
| Family COVID Experience c | ||||||
| No (REF) | ||||||
| Yes | 0.839 | .475-1.482 | 0.546 | 0.927 | .541-1.589 | 0.783 |
DISCUSSION
We noted a high rate of COVID-19 vaccine hesitancy and refusal for children in our urban cohort. Contrastingly, previous studies have reported a higher parental intent (65%-80%) for COVID-19 vaccination [12,13]. However, these studies were conducted early in the pandemic when significant uncertainty existed about the disease, severity and outcomes. Additionally, the majority of caregivers in our study identified as African American and had less than an associate degree; both being previously associated with lower vaccine acceptance rates [8,14,15]. Similar to previous studies [12,14], the main reasons for vaccine refusal and hesitancy were insufficient data and concerns regarding the vaccine’s safety and efficacy. A small minority of caregivers were also concerned about their child contracting COVID-19 disease from vaccination. In light of these findings, it is critical to strengthen public trust by bolstering positive perceptions about vaccine safety and efficacy noting that the serious side effects are rare and that the benefits of vaccination outweigh the risks.
In keeping with other studies [8,12,14], when compared with their peers, COVID-19 vaccine acceptance rate was higher among caregivers who opted for childhood and seasonal influenza vaccination. Troublingly, acceptance for COVID-19 vaccine was relatively low even among these caregivers. A high proportion of caregivers who accepted the vaccine for themselves were hesitant to accept it for their children, possibly driven by the belief that severity of COVID-19 disease in children does not warrant vaccination. Health care providers should be empowered via appropriate training and support to guide caregivers in making an informed decision using scientific evidence. It has been suggested that programs with a proven track record that have been successful with implementation of other vaccines, such as the CDC’s Assessment, Feedback, Incentives, and eXchange (AFIX) program, can be used for provider education and feedback to improve COVID-19 vaccination rates [16].
Some studies have shown that lack of trust in vaccines and healthcare systems account for the higher vaccine refusal and hesitancy noted in African Americans and lower education groups [17,18]. Further, the COVID-19 pandemic has highlighted the adverse effects of social determinants of health on not only the disease outcomes but also vaccine acceptance. A multipronged approach, including educational interventions to disperse accurate information with transparency, could prove pivotal, especially in populations with higher vaccine hesitancy. In this vein, the Centers for Disease Control has recommended a community-driven approach including identification of community partners, understanding of barriers to vaccination and implementation of plans with funding support for vaccination messaging, outreach, and administration to improve vaccination rates among racial minorities [19].
Mothers were more likely to express COVID-19 vaccine hesitancy and refusal in our study. Although this could be secondary to the fact that majority of caregivers who participated in our study were mothers, Simonson et al.[20], have previously shown that mothers were more reluctant to vaccinate their child against COVID-19 compared to fathers (27% vs.11%). Further they found that young mothers were more likely to refuse vaccination compared to their older peers. The authors suggest that young mothers are more exposed to social media and hence at higher risk of accepting misinformation regarding the vaccine. Surprisingly, the presence of medical co-morbidity was not associated with a higher vaccine acceptance. Goldman et al12 reported a lower rate of intent to vaccinate in caregivers of children with chronic illness as well. Since children with chronic illness are at higher risk for severe COVID-19 disease [21], and would benefit the most from vaccination, focused efforts should be undertaken to promote vaccination in this cohort.
This study has several limitations to consider. First, this is a single center study with a small convenience sample size. Additionally, 15.2 % of the surveys could not be used in the regression analysis due to missing response on one or more variable. However, there was no difference in the patient and caregiver demographics, caregiver relationship, education status and presence of medical co morbidity between these and the overall sample. Our results may not be generalizable to other communities with different baseline vaccine acceptance rates, racial, and educational backgrounds. Further, the timing of the study may have influenced the results. The survey was conducted post-pandemic peak, during the time when alpha strain of SARS CoV-2 was prevalent, and during the time when safety concerns was raised regarding the Johnson and Johnson vaccine but prior to the reports of pericarditis/myocarditis in young adults [22], which could have influenced the survey responses. Finally, the survey was conducted close to the time when emergency authorization for vaccine was provided for children ≥ 12 years of age which could account for the higher acceptance rates in older children.
CONCLUSIONS
A high rate of COVID-19 vaccine hesitancy and refusal for children was noted in our urban cohort. While African American caregivers and mothers were more likely to express vaccine hesitancy, older age of children and higher parental education levels were associated with vaccine acceptance. Targeted interventions aimed at promoting safety and efficacy of COVID-19 vaccine in children, particularly in the African American community, is needed to improve vaccine acceptance rates.
Ethical Approval: This study was approved by our Institutional Review Board ((#2020-1614).