Pediatric Onychomycosis: 10-Year Evaluation in a Tertiary Hospital in Brazil
- 1. Department of Pediatrics - division of Pediatric Dermatology, Federal University of Paraná, Brazil
- 2. Graduate program in Child and Adolescent Health, Federal University of Paraná, Brazil
Abstract
Introduction: Onychomycosis is a rare nail fungal infection in children and few authors have evaluated the topic in Brazil. This study aimed to evaluate the clinical characteristics and pathogens of onychomycosis in the pediatric population in a tertiary hospital in Brazil.
Methods: Retrospective and analytical study with review of medical records from a tertiary hospital in southern Brazil, evaluating patients up to 18 years of age and suspected diagnosis of onychomycosis. Data were tabulated and analyzed using JMP 10 software.
Results: Evaluated 77 medical records of patients with suspected onychomycosis, in 47 (61%) the infection was confirmed, 26 by histopathology by nail clipping and 21 by positive culture by nail scraping, the latter comprising the final sample. Thirteen cases (61.9%) were male and the median age was 11.3 years. The most frequent pathogen was Trichophyton rubrum (33.3%). Eight patients (66.7%) were treated with topical antifungal agents only, and all were cured, with a median time of 12 months.
Discussion: Although infrequent in the pediatric age group, an increase in the overall prevalence of onychomycosis is observed in this population. Trichophyton rubrum was the main pathogen, but there is a lacking of studies and divergent results regarding the main agent responsible for onychomycosis in the Brazilian population. Topical treatment was the most used, an important particularity of pediatric patients. Systemic antifungals have a higher risk of adverse events and require adjusted doses for children and adolescents. Topical treatment may be a good alternative in this population that has thinner and faster growing nails, showing greater response to treatment than adults.
Conclusion: Onychomycosis is an important differential diagnosis in nail dystrophies. Trichophyton rubrum was the main pathogen causing the disease. Topical antifungal treatment was the most used, a particularity of pediatric patients, and may present a better response compared to adults.
Keywords
Child, Onychomycosis, Prevalence, Pediatric dermatology, Dermatomycosis
CITATION
Cerqueira TB, Morgan MAP, Carvalho B, Fatturi AL, de Carvalho VO, et al. (2023) Pediatric Onychomycosis: 10-Year Evaluation in a Tertiary Hospital in Brazil. Ann Pediatr Child Health 2023; 11(4): 1314.
INTRODUCTION
Superficial cutaneous fungal infections are the fourth most common health problem worldwide, and encompass skin, hair and nails [1]. Onychomycosis is the fungal infection of the nail plate responsible for 15% of nails dystrophies in children [2,3]. They are less frequent in the pediatric age group when compared to adults, for reasons such as faster nail growth, minimal trauma, less surface area for invasion by the fungi, and lower prevalence of concomitant Tinea pedis [4,5].
The disease presents with a variety of nail changes, such as discoloration or yellowing, subungual hyperkeratosis, onycholysis, cracks and destruction of the nail plate. It is acquired by direct contact of the nail with the fungus or by dissemination of fungal infection from the affected skin, such as Tinea pedis [3-5]. Diagnostic confirmation by culture is important, and the most frequent agents are dermatophytes (Trichophyton rubrum, Trichophyton mentagrophytes), followed by yeasts (Candida spp) and non-dermatophytes (Fusarium oxysporum and Aspergillus fumigatus) [6,7]. The location on the nail plate and the invasion pattern of the fungi determine the clinical subtypes of onychomycosis [4,6].
Epidemiologic evaluations on the prevalence of fungi in a geographic region are important for treatment and implementation of preventive measures. An increase in the occurrence of onychomycosis in the pediatric age group in recent years is described and few authors have evaluated the topic in Brazil [8]. Worldwide the prevalence of onychomycosis in children on a population basis can reach 3.37% to 0.53% respectively and in dermatological and pediatric centers, but still with few pediatric studies in Latin America [6,9]. This study aimed to evaluate the clinical characteristics and pathogens of onychomycosis in the pediatric age group in a university hospital in Brazil.
MATERIALS AND METHODS
Retrospective and analytical study. A review of medical records of patients who consulted at a Pediatric Dermatology outpatient clinic of a University Hospital, located in the southern region of Brazil, was carried out. Patients up to 18 years of age, seen from January 2012 to November 2022, with suspected diagnosis of onychomycosis were included.
The following parameters were determined for analysis: age and sex of patients, area of residence (rural or urban), age of onset of symptoms, age at diagnosis, presence of associated diseases, family history of onychomycosis, presence of concomitant Tinea pedis, clinical type of onychomycosis, site of involvement, agent identified in the culture, histopathological findings of the nail plate and type of treatment. For evaluation of the direct mycological examination, the technique used routinely in the laboratory is clarification by KOH 20%, and for cultures, Sabouraud dextrose agar with and without cycloheximide is used. The species of positive cultures are identified by micromorphological and macromorphological evaluation. The collected nail fragments were stored in formaldehyde, embedded in paraffin block, and the slides obtained were stained in PAS-cd (with digestion). Microscopic analysis was performed for hyphae detection.
Data were analyzed using JMP 10 software. Measures of central tendency and dispersion are expressed as means and standard deviation (mean + SD) for continuous variables with symmetrical distribution and as medians, minimum and maximum values (minimum- maximum) for those with asymmetrical distribution. The Mann-Whitney and Kruskal-Wallis ANOVA tests were used to estimate the difference between variables with asymmetric distribution. For all tests, a minimum significance level of 5% was considered and the sample studied confers a minimum test power of 90%.
RESULTS
We found 77 medical records of patients with suspected diagnosis of onychomycosis, in 47 (61%) the fungal infection was confirmed, being in 26 patients through histopathological evaluation with the collection of nail clipping demonstrating the presence of fungi and 21 by positive culture for fungi through nail scraping, and the latter composed the final sample. Thirteen cases (61.9%) were male and 8 female (38%). The median age of the patients was 11.3 years, ranging from 1 year and 3 months to 16 years and 2 months.
Of the patients analyzed, 19 (90.4%) lived in urban areas, 12 (57.1%) were diagnosed with concomitant Tinea pedis and 9 (42.8%) had a family history of onychomycosis. None of the children and adolescents evaluated had immunosuppression or other comorbidities.
Pododactyl nails were affected in 20 cases (95.2%), with concomitant involvement of chirodactyl nails in 1 patient (4.7%). The distal subungual clinical form occurred in 20 patients (95.2%).
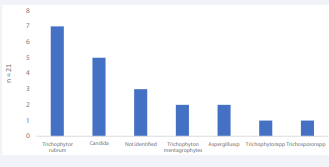
The most frequent pathogen was Trichophyton rubrum, present in 7 cases (33.3%), followed by Candida with 5 cases (23.8%). In 3 (14.2%) cultures there was the growth of Dermatophyte but it was not possible to determine its genus. There were 2 cases of Trichophyton mentagrophytes (9.5%), 2 of Aspergillus sp (9.5%) (Graph 1).
Graph 1: Frequency of pathogens in pediatric onychomycosis
Topical treatment was prescribed for 18 patients (85.7%). Cyclopiroxolamine enamel was used in 14 patients (66.6%), followed by amorolfine enamel, used alone in 1 patient (4.7%). And 3 (14.2%) initially used cyclopiroxolamine and later amorolfine in their treatments.
Nine patients (42.8%) received systemic treatment, and among these 6 (28.4%) were treated concomitantly with topical antifungals. Terbinafine was the most commonly used systemic antifungal in 6 patients (28.6%), followed by fluconazole in 3 patients (14.3%). Only 1 patient (4.7%) required the use of two systemic antifungals, terbinafine and later fluconazole.
At follow-up, 6 (28.5%) patients were lost to follow-up during treatment. In the evaluation of the 15 patients (71.5%) who completed treatment, the median treatment time was 12 months (5-18 months) for complete improvement. When evaluating the 12 patients (57.2%) who underwent only topical treatment, 4 patients (33.3%) were lost to follow-up and of the 8 (66.7%) who completed treatment all healed, with a median time of 12 months (6-20 months).
There was no difference regarding patient age at diagnosis and the use of topical or systemic treatment, and between patient age at symptom onset and the type of pathogen causing onychomycosis (p>0.05) (Table 1).
Table 1: Distribution of patients by age according to treatment used and pathogen.
|
Treatment |
n |
Age at diagnosis* (mean ± deviation) |
p |
|
Fluconazole |
3 |
12,5±2,7 |
|
|
Terbinafine |
6 |
11,0±1,7 |
0,84 |
|
Topical antifungal (enamel) |
12 |
9,3±5,0 |
|
|
Pathogen |
n |
Age at onset of symptoms* (median/range) |
p |
|
Aspergillus |
2 |
8,7 (2-15,5) |
|
|
Candida |
5 |
7,0 (0-11) |
|
|
Dermatophyte |
3 |
12 (3 -14,1) |
0,67 |
|
Trichophyton mentagrophytes |
2 |
7,2 (7-7,4) |
|
|
Trichophyton rubrum |
7 |
11,0 (1-12) |
|
|
Trichophyton sp |
1 |
1,5 |
|
|
Trichosporon |
1 |
10 |
|
* age in years
DISCUSSION
Cutaneous fungal infections are less frequent in children when compared to adults, but predominate in the group of infectious dermatoses in the pediatric population. Although onychomycosis is not a frequent disease in the paediatric age group, with an estimated prevalence of 0.35-5.5%, an increase in the overall prevalence has been observed in this population possibly due to increased urbanization, increased frequency of early use of closed shoes, increased prevalence of obesity, and an increase in the knowledge of physicians making the diagnosis [3,4].
In the present study, the median age of the patients was 11.3 years, a result similar to that pointed out by Solís-Arias in his literature review carried out in 2017, which pointed out that it is a more prevalent disease in adolescents, despite a smaller number of published epidemiological studies of onychomycosis in the pediatric age group when compared to adults [5].
The nails of the pododactyls were affected in 20 cases (95.2%), as already described in a review by Leung et al, stating that the pododactyls are affected 7 to 10 times more often than the chirodactyls, and the involvement of the first pododactyl is even more frequent [2].
Of the patients analyzed, 19 (90.4%) lived in urban areas, 12 (57.1%) had concomitant Tinea pedis and 9 (42.8%) had a family history of onychomycosis. These findings reinforce the predisposing factors for onychomycosis such as the use of occlusive and tight shoes, fungal infection in other parts of the body, hyperhidrosis, practicing sports activities, nail trauma, community toilets, and family members with fungal infection [2,5].
Untreated or inadequately treated Tinea pedis is a predisposing factor for the development of onychomycosis, and the presence of both dermatoses in the same patient is frequent. Tinea pedis can serve as a reservoir for the dermatophyte that subsequently infects the nail causing onychomycosis. In a systematic review by Gawdzik et al. of 2,382 children with onychomycosis, 527 (22%) children had concomitant Tinea pedis [10]. In our study, an even higher value was found, more than half of the cases had concomitant Tinea pedis, demonstrating the importance of complete dermatologic examination for early detection and treatment of Tinea pedis in order to avoid contamination of the nail.
It is known that individuals with fungal infections easily infect other family members, as occurred in the present study in which 42.8% of the sample had a family history of onychomycosis. Jazdarehee et al., in a review of 90 articles, demonstrated that in 44 to 47% of households with infection of an initial member there was dissemination of onychomycosis, in addition to identifying the same strains of dermatophytes in affected members in the family, suggesting that shared equipment and surfaces in the same house can be a cause of reinfection and dissemination of onychomycosis among family members [11].
In the present analysis Trichophyton rubrum was the main pathogen causing the disease. There is a lack of studies regarding the epidemiological characteristics of the main pathogens causing specific onychomycosis in the Brazilian pediatric population, with divergent results regarding the main agent responsible for onychomycosis in the Brazilian population. Similar to the present study, Wille et al performed in São Paulo/Brazil (BR) an evaluation of the epidemiology of dermatomycosis in a city in the interior of the state, and in a sample with 20 positive cultures for onychomycosis, without specifying age, Trichophyton rubrum was the most prevalent pathogen [12].
Other studies have shown a higher prevalence of Candida pathogens in the Brazilian population with onychomycosis. Correia et al performed an epidemiological evaluation of superficial mycoses in children from Mato Grosso/BR and obtained a sample of 49 patients with onychomycosis, and the most common pathogen found was Candida albicans [13]. Maranhão et al., also found Candida albicans as the most frequent species in a retrospective study covering the three main tertiary centers in Alagoas/BR, between 2009 and 2016, with a sample of 3316 patients composed of children, adults and the elderly [14]. In addition, a study carried out in São Paulo/Brazil (BR) by Martin et al, with nail fragments from 184 patients, over 19 years old with suspected onychomycosis, Candida parapsilosis was the most frequent agent [15].
Topical antifungal treatment was the most commonly used in the present study, an important particularity of pediatric patients. Systemic antifungal treatments are generally more effective for the treatment of onychomycosis, but they have a higher risk of adverse events and require dose adjustments for children and adolescents, with different therapeutic implications. In this context, topical treatment may be a good alternative in this population that has thinner and faster growing nails, and thus may show a greater response to this type of treatment than adults [8,16,17].
CONCLUSION
A limitation of this study is the low number of positive cultures. The explanation could be due to the sample collected in an erroneous way, since there is greater difficulty in collecting in the pediatric age group, with insufficient material for analysis. Despite this, the importance of this study is to provide an overview of the epidemiology of onychomycosis in the pediatric age group in southern Brazil over a 10-year period.
Although infrequent in children and adolescents, onychomycosis is an important differential diagnosis in ungueal dystrophies, the main causative agent was Trichophyton rubrum and topical treatment was effective.
Studies such as this are fundamental for the knowledge of the epidemiology and etiology of onychomycosis cases, with consequent contribution to better control of infection, optimization of treatment and reduction of recurrences.