Role of Conservative Management in Hemophagocytic Lymphohistiocytosis in a child with Pulmonary Tuberculosis
- 1. Department of Pediatric Infectious Diseases, Bai Jerbai Wadia Hospital for Children, India
- 2. Grant Government Medical College, India
Abstract
A 7-year-old girl presented with a month-long history of fever, cough, and fatigue and hepatosplenomegaly with low erythrocyte sedimentation rate and transaminitis. She was diagnosed to have drug sensitive Mycobacterium tuberculosis (M.Tb) on sputum Xpert MTB/Rif assay. She was also detected to have hemophagocytic lymphohistiocytosis (HLH) with high ferritin and hemophagocytes on bone marrow aspiration. She was managed conservatively with anti tuberculous therapy (ATT) to which she responded.
Keywords
• Pediatric Tuberculosis
• Hemophagocytic lymphohistiocytosis
• Low dose steroids
CITATION
Joshi M, Jain S, Shah I (2023) Role of Conservative Management in Hemophagocytic Lymphohistiocytosis in a child with Pulmonary Tuber culosis. Ann Pediatr Child Health 2023; 11(5): 1320.
INTRODUCTION
Tuberculosis (TB), caused by Mycobacterium tuberculosis (M.Tb), is a widespread infectious disease that primarily affects the respiratory system but can involve various organs [1]. Hemophagocytic lymphohistiocytosis (HLH) is a rare and life threatening disorder characterized by dysregulated activation and proliferation of macrophages and T lymphocytes, leading to severe inflammation and tissue damage [2]. While the association between HLH and TB has been extensively studied in adults, limited data are available regarding this association in pediatric patients [1]. A 7-year-old girl with MTB had HLH and was successfully managed by conservative approach rather than intensive treatment.
CASE REPORT
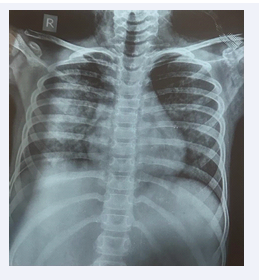
A 7-year-old girl presented with a persistent fever lasting for a month, accompanied by cough and fatigue. Her medical history revealed no contact with tuberculosis (TB) patients, recurrent infections, or previous hospital admissions. She weighed 21 kgs and height was 117 cms [both between 25th and 50th percentile as per Indian Academy of Pediatrics (IAP) growth chart]. On general examination, she had a heart rate of 126/min, respiratory rate of 36/min, blood pressure of 100/60 mm of Hg (between 50th and 75th percentile). On systemic examination, there were fine crepitations present on right inframammary area, with hepatomegaly and splenomegaly. Other systems were normal. Sputum Xpert MTB/Rif assay test confirmed the presence of M.tb with rifampicin sensitivity. Chest X-ray revealed bilateral haziness (Figure 1).
Figure 1: Chest Xray showing bilateral haziness.
CT scan of the chest and abdomen revealed ground glass haziness in both lungs, splenic granulomas, and changes suggestive of pyelonephritis in both kidneys.
Laboratory tests showed persistent lymphopenia, with an unusually low erythrocyte sedimentation rate (ESR) of 2 mm/hour (Table 1). Due to elevated liver enzymes (aspartate transaminase - 165 IU/L, alanine transaminase - 84 IU/L, total bilirubin - 1.1 mg/dL; direct - 0.8 mg/dL), indicating transaminitis, she was initiated on anti-tuberculosis treatmen (ATT) consisting of ofloxacin, ethambutol, and linezolid. However, instead of improvement, her condition worsened after two days, characterised by high-grade fever, respiratory distress, and abdominal tenderness with hepatomegaly. She was suspected to have HLH and serum triglycerides (227 mg/ dL) and ferritin (573 mcg/L) were also elevated. HIV ELISA was negative. Cytomegalovirus (CMV), Ebstein Barr virus (EBV) and Parvovirus PCR were negative. Bone marrow aspiration revealed the presence of hemophagocytes. She was treated with non invasive ventilation for 48 hours and was subsequently weaned off oxygen, transitioning to room air. At this juncture, steroids or intravenous immunoglobulin were not added. Over the course of 72 hours following the initial worsening, her condition gradually improved. Her clinical condition stabilised without addition of any immunosuppressants. Her serial hemogram are depicted in Table 1. Consequently, she was switched to a first-line ATT regimen consisting of isoniazid, rifampicin, ethambutol, and pyrazinamide on normalization of liver enzymes.
DISCUSSION
TB is highly prevalent in Asia, including India, where it remains a significant public health concern. TB commonly presents with respiratory symptoms such as cough, fever, and fatigue. However, it is important to note that TB can manifest in disseminated forms, affecting multiple organs beyond the lungs [3]. Our patient had pulmonary TB. Laboratory findings supported the suspicion of hemophagocytic lymphohistiocytosis (HLH), including persistent lymphopenia, an unusually low erythrocyte sedimentation rate (ESR), and high ferritin levels. These criteria align with the diagnostic protocol for HLH, which includes the presence of specific symptoms and laboratory abnormalities [4]. Although TB infection disturbs immune homeostasis and causes secondary HLH, the pathophysiology of HLH involves excessive immune activation and cytokine storm. However, the underlying mechanism of TB-HLH is still unknown [5].
Based on the case report by Hauch et al., the management of HLH in the context of TB often involves a combination of anti-TB therapy and immunomodulatory agents such as dexamethasone, etoposide, and intravenous immunoglobulin (IVIg) [6]. However, in our patient, we successfully managed the condition with a minimal treatment approach, consisting of the standard anti-TB regimen. Non-invasive ventilation was also employed to support respiratory function. The outcome of our patient suggests that in select cases, a conservative treatment may be sufficient for managing TB-associated HLH. This approach may be preferable before considering more aggressive immunomodulatory interventions.