The Impact of Covid-19 on Health Care Organization
- 1. Ministry of Health, Muscat, Oman
CITATION
Al Zadjali N (2023) The Impact of Covid-19 on Health Care Organization. Ann Public Health Res 10(2): 1125.
ABOUT NATIONAL HEALTHCARE UK
The Health and Social Care Act 2012 implemented the most central and divisive structural changes to the NHS since the service’s inception in 1948. The 2012 Act enacted significant health care changes stated in the July 2010 White Paper Equity and excellence: Liberating the National Health Service (NHS). This document outlined the 2010 Government’s goals for decentralizing NHS governance, including physicians in health care commissioning and increasing patient choice [1].
Numerous provisions of the 2012 Act took effect on 1 April 2013. When:
- NHS England and Clinical Commissioning Groups (CCGs) were given legislative responsibility for health service commissioning.
- Local governments took on additional public health obligations.
- Community health watchdog organizations were formed.
- The Strategic Health Authority and Primary Care Trust have been formally decommissioned [2].
Measuring the Production and Productivity of Health Care Services
For the Covid-19 response, the NHS in the U.K. will spend an additional £50bn over the next five years, a massive rise in health spending. However, because there is no market pricing with which to deflate expenditure, it has always been challenging to assess the output of the public sector, including health care, volumetrically. For a long time, everyone assumed that the value of outcomes equalled the value of inputs, resulting in zero productivity increase [3]. For this reason, even when statistical offices around the world used the same approach, cross- country comparisons have always been difficult. Even when focusing solely on health care, the NHS in the United Kingdom and for- profit hospitals in the United States provide stark contrasts. The Office of National Statistics has also varied its methodological methods over the last few decades, going farther than most others in adopting direct production measures for use in the national accounts and establishing quality-adjusted output for the individual assessment of public sector productivity. There are further challenges when comparing outcomes to results, such as how hospital or G.P. treatments affect health outcomes and public health and environmental issues. We begin with outputs, but the final section will return to products essential for increasing the overall economy’s productivity [4]. Health care practices throughout the epidemic have been altered [5].
PERFORMANCE AND FUNDING
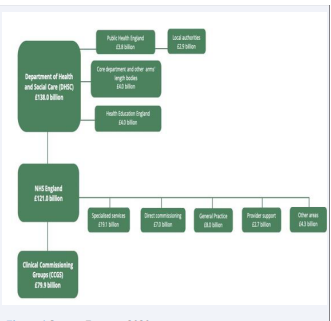
The Department of Health and Social Care allocates funds from its overall budget to support health care (DHSC). The DHSC budget in England for 2019/20 was $138 billion. NHS England has received the vast majority of this funding. In addition, DHSC funds independent organizations such as the Care Quality Commission, NHS Improvement, and the National Institute for Health and Care Excellence (NICHE), distributing the remaining funds (NICE). Ministers have ordered that NHS England’s funds be used to fulfil its obligations to the health and social care system (DHSC) [6]. NHS England monies are allocated by Clinical Commissioning Groups (CCGs) and local governments. Spending on health care services accounts for most CCG funds (£79.9 billion in 2019/20) [7]. Direct national commissioning (£41.1 billion in 2019/2020) includes specialist services (£19.1 billion), primary care (£8.8 billion), and maintenance, military, and offender services ($7.0 billion)-more than half of NHS England’s remaining resources (Figure 1).
Figure 1: Source: Expatica 2020.
For the benefit of Public Health England, NHS England distributes a significant portion of its budget to programs and services that are centrally controlled. NHS funding sources in England are depicted in the diagram below [8].
WHAT A NATIONAL HEALTHCARE MANAGED DEMAND/NEED DURING PANDEMIC
The COVID-19 epidemic has severely disrupted global supply lines. To monitor and limit the spread of the Pandemic, each country needed medical supplies. When we talk about “medical goods,” we’re not talking about drugs; instead, we’re talking about things related to health care. From the most basic (such as personal protective equipment or PPE-like) to the most high-tech (such as ventilators and MRI machines), these products cover a broad spectrum of needs [9]. Personal Protective Equipment (PPE) and medical devices are two different business areas within the “medical goods” industry because of product line- specific technical and technological distinctions. Facemasks (medical masks and N95-type respirators) and gloves will focus on this study’s first category of Personal Protective Equipment (PPE). Increased demand for both product lines has resulted in severe shortages across the healthcare sector since the Pandemic began [10]. There is a complicated supply chain including multiple manufacturers, distributors, and other intermediaries for these product lines, exposed to several offshore waves in recent decades. Most Personal Protective Equipment (PPE) was made in China before the COVID-19 Pandemic, with the United States being the leading importer of products such as face masks, eye protection, and medical gloves. Health care systems have prioritized cost optimization and inventory reduction for an extended length of time, which is why PPE-related sector offshoring was driven mainly by economic concerns [11]. The distinction between measuring production and productivity and health and economic well- being must also be made. The health outcomes have been better than if the NHS had not substantially changed its operations during the Pandemic. Effects will integrate a more complex collection of factors, including life years lost due to treatment delays or cancellations and Covid-19 lives saved [12].
CHANGES IN HOSPITAL’S TYPICAL WAYS OF OPERATION
There is a global epidemic of COVID19. COVID19 therapy and reduced non-COVID treatment considerably affect the number and case mix of patients treated in high-income nations. There was an increase in COVID patients in all countries but a reduction in patients with other conditions. These developments affect health care providers’ financial well-being, although the impact has varied depending on how health care systems are typically structured and funded and the extent to which government rules protect providers [13]. By comparing the financial consequences of the COVID19 Pandemic in the United States to those in three other healthcare systems (England, Germany, and Israel), we can analyze the political and policy components that contributed to the intensity and distribution of COVID19’s repercussions on U.S. providers [14]. To combat a pandemic, the NHS is leading the way. Even though hospitals are typically under-capitalized, demand for Covid-19 treatment regularly rises because of the quick spread of the disease and the severity of its symptoms. Medical and non-medical executives must make clinical operations and resource allocation choices daily as a result of this [15].
Facilitators of Rapid Organizational Transformation and their Future Ramifications
According to our interviews, hospitals were able to rapidly adapt to the Pandemic due to (1) widespread support from both NHS staff and external stakeholders, (2) increased funding, (3) streamlined governance processes and governance structures,
- the establishment of rapid surge capacity, and (5) improved communication and technology infrastructure [16]. There was no doubt about it: Despite the destruction, many people interviewed said the Pandemic’s dynamics helped remove unnecessary red tape, which might lead to reconsidering service delivery and future development in NHS facilities.
- The capacity to recruit, retain, and adjust employees. Because of the desire of the NHS workers to work together to combat the virus, hospitals were able to achieve quick advances. On the other hand, current dynamics have raised stress, fatigue, aversion to future change, and the urge to deliver more services [17].
- State assistance. The elimination of funding constraints enabled hospitals to start large procurement programs for consumables swiftly (e.g., personal protective equipment), testing capacity and equipment (e.g., ventilators), as well as to launch previously underfunded continuous improvement projects [18].
- Infrastructure is needed for the technology to work. Like many other businesses, hospitals have spent much money to make it easier for people to work from home. Videoconferencing made it easier for people to communicate and work together inside and outside hospitals [19].
HEALTH CARE AS SOCIAL INFRASTRUCTURE: CAPACITY, DEMAND PEAKS, AND HOW IT HELPS PEOPLE LIVE THEIR LIVES
Hospitals, by definition, try to figure out how many Covid-19 patients they will have in the future. In 2020, they could figure out how many Covid-19 patients they would have. Capacity needs can be thought of in terms of how much space is needed and how much space is not used, like empty beds. More advanced models also include queuing. However, the NHS has mostly stayed away from these methods. Instead, it has used “demand control” (NHS England, 2016; i.e., limiting demand) in conjunction with a “just- in-time” approach to bed, staffing, and supply management [20]. Thus, NHS England has always had higher occupancy rates and fewer beds per 1000 people than other industrialized countries. Due to the NHS’s emphasis on “lean manufacturing” could not meet peak demand and had to stop non-Covid-19 activities. In addition, the quasi-fixed-proportions nature of the production function makes surge capacity even less likely [21].
GREEN PRACTICES IN HEALTH CARE
As a health care provider, you have two significant challenges: improving the population’s health and reducing your environmental imprint. In health care, executives have a unique opportunity to directly address the industry’s ecological footprint while simultaneously ensuring that the neighbourhoods and people they serve are healthy and safe in the face of possible climate change risks [22]. Many health professionals and organizations are interested in green health care, which incorporates environmentally friendly practices into healthcare delivery. As environmental protection becomes more critical, it can make a positive impact. Health care institutions are shown to be good citizens in the community due to this initiative. Children and the general public can benefit from its use. Money can be saved by doing this. Green health care was discussed at length at the Roundtable on Environmental Health Sciences, Research, and Medicine’s (Roundtable) meeting on January 10-11, 2006, for numerous reasons. As a healthcare worker, green health care is the most appealing option. This is because it can protect and enhance one’s health [23,24].
Green construction can be described in a variety of ways. According to the Federal Environmental Executive’s Office, “green or sustainable construction is designing and constructing structures in such a way that natural resources are conserved and pollution is minimized” (OFEE, 2003). This phrase is used throughout the process of designing, constructing, and operating a healthcare institution. According to the Green Guide for Healthcare, several strategies enhance a healthcare facility’s environmental performance (2006). These include site selection, energy efficiency, the use of recycled and renewable materials, low-emission materials, alternative modes of transportation, daylighting (the use of natural light in a space to reduce reliance on electric lighting and energy costs), waste reduction, local and organic food consumption, and green cleaning materials [25]. Certain decisions, such as where to build, are decided during the design and construction phases; others, such as where to obtain food and clean, are determined after the structure is complete. Commitments to energy conservation, renewable resource use, and other principles must be established and maintained throughout the life of a facility, from construction through shutdown and replacement [26].
NEED FOR GREEN PRACTICES IN HEALTHCARE
There are also moral reasons to look for green health care. Autonomy, beneficence, non-harm, and justice are the four main principles of biomedical ethics (Beauchamp, 2001; Engelhardt, 1995). Green health care is an excellent example of both beneficence and nonmaleficence. It benefits patients and staff, as well as nearby and distant communities, as well as future generations. It also avoids the harm that may come from certain conventional practices. Public health ethics has been linked to three philosophical traditions: utilitarianism, liberalism, and communitarianism (Roberts and Reich, 2002). All three have solid arguments for green health care. Utilitarians would say that greening healthcare facilities improve the total well-being of people, including patients, staff, visitors, and people in the community [27]. Liberal thinkers, following Kant, would say that policies and practices that allow people to be exposed to dangerous things violate their right to a healthy environment. Moreover, communitarians would say that green health care helps make a “good society” possible. The Principles of Ethical Public Health Practice say that public health should focus on the leading causes of illness and the health needs to prevent health problems. This seems like green health care. (2002-2004) (Thomas, et al.). Thus, green health care aligns with biological and public health ethics [28].
HOW IS GREEN HEALTH CARE IMPLEMENTED?
As with any complex system, healthcare institutions are not conducive to rapid transformation. Numerous elements influence change, including the emergence of new external demands, the surfacing of new data, the reframing of concerns about healthcare organization administration, the effect of visionary leadership, and the reconciliation of opposing internal interests [29]. Each of these characteristics may contribute to the sustainability of health care; indeed, each may be critical. Green health care supporters must understand institutional dynamics, including institutional strengths and weaknesses, and opportunities and risks at the institutional and more significant operational levels. Success stories in green healthcare may be educational in displaying what works and what might go wrong [30].
ROLE OF PROCUREMENT MANAGER
Procurement of resources and items for use and resale demands care, so the procurement manager plays a vital role in a business. The procurement manager’s primary function is to coordinate and communicate with buyers and purchasing departments in various companies. The procurement manager must guarantee that his organization obtains items and services of the highest quality-the following highlights the procurement manager’s responsibilities in a healthcare organization [31].
As procurement managers, the things we need to consider while making orders are stated below:
- Price: As a procurement managers, we need to consider the price factor before ordering. We have to order according to our Hospital’s needs and keep our budget in mind. We have to spend budgeting equally on every product.
- Volume: if we order too much of a product, that’s also a problem. So before ordering manager has to see how much of an amount is needed to be ordered/purchased so that we can type correctly. If we collect too much on a single product, it will only affect our budget and consume space in our storage room for a long time.
- Quality: Quality should be the prime criterion to select a product. As healthcare organization managers, we cannot compromise on the quality we provide to our customers. The customer put their 100% trust in healthcare organizations, so we are responsible for giving them the best we can. So, the manager has to evaluate every product before making a final decision.
- Demand: The manager has to see the direction of each product before ordering them. Managers must order items that are used excessively in huge quantities and things not usually used in low amounts.
- Internal Capabilities: A company’s in-house staff can complete any task or operation. Assessing your internal capacities can help you identify your strengths and deficiencies. The manager has to look into these as well.
- Vendors: The manager also must look into the vendor’s background before making multiple purchases. And if the products are excellent and practical, the manager can make a long-term contract with them.
- Storages: it is also an essential part of the purchasing decision. The manager has to purchase according to its ability to keep it for some time. If healthcare has small space, then order in small amounts, and if the unit has enough space, we can purchase every month.
- Lead Time: The manager also has to keep in mind the receiving time after making an order. We have to make order keeping this time in mind.
- Return and Refund Policy: the manager has to make an order by keeping Refund and return policies. If the product does not fall under the acceptance criteria manager will be required to refund or replace them.
- Stock Safety: the manager has to train their team to handle every product carefully
- .Lean implementation begins with identifying and removing waste to provide more value to customers or patients. There are several examples of poor healthcare in the literature. The healthcare system’s ultimate purpose is to treat or relieve patient misery. The ultimate goal of all healthcare procedures is to accomplish this. Drugs, medicines and medical equipment were employed to achieve this final objective. As a result of lean adoption in the healthcare system, patient satisfaction and service delivery time are critical performance metrics. Healthcare facilities require multi-skilled personnel to manage various healthcare activities, including some in which patients are actively involved. Front-line healthcare workers need to be retrained to enhance patient care. And the requirement to provide fast feedback on the quality of one’s job. Reducing the number of stages in the process, reducing the number of steps that employees have to walk, and decreasing the time it takes to fix errors are all part of the lean implementation.
OPERATIONAL RISK
NHS trusts operate in an adversarial environment. Claims for clinical negligence and employee harm might cost hundreds of thousands or even millions of pounds, with potentially dire financial consequences for the trust issue. Since 1 April 1995, trusts have been allowed to join the Clinical Negligence Scheme for Trusts (CNST), which pools donations to fund high-cost claims. After exhausting all other avenues, insurance should be a last resort for risk transfer. Such risks should still be handled as part of a comprehensive strategy for managing trust risk. The consequences of the NHS and Community Care Act 1990 require trusts to adapt to the requirements of a new healthcare system. To be successful, beliefs must make optimal use of their limited resources. Unmanaged risk consumes funds not budgeted for. Eliminating or lowering exposure to unknown/unwanted/ unacceptable risks and providing adequate protection for remaining risks will guarantee that the economic effect of purchaser choices can be borne. Risk management strategies are critical for dealing with financial hazards that occur infrequently but have a significant impact.
A strategy for operational risk management is primarily concerned with operational hazards and the policies and procedures necessary to control risk and meet year-to-year service objectives. This is not to be confused with the risk assessment required by the Capital Investment Manual. As a result, it is unnecessary to outline the risks connected with potential acquisitions and dispositions, estate development control plans, estate rationalization plans, and estate investment programs, among other things. However, capital investment projects must consider operational risk. Similarly, the risk strategy does not need to include extensive rules and procedures for each component, as they will be dynamic and subject to change frequently.
FINANCIAL RISK
Financial hazards encompass any dangers that might jeopardize trust turnover and viability. This category is expanded, and the risks may be quantified by comparing each component to the financial risk profile for trusts in England and Wales. Other transitory elements, such as the future influence of government action on issues such as trust mergers, should also be considered. Finance is the trust’s immediate high-impact/low-frequency risk. As a result, a massive endeavour should be launched to address this threat. A tailored public relations effort should increase the trust’s reputation and prestige in the local and nearby areas. High-level meetings should be convened to lobby regional offices and important decision-makers at the health authority.
Contingency plans for all activities should be developed to reduce the consequences of any significant change in patient volume, profile, or financing.
There are four types of Operational Risk Faced by the National Health Care UK:
-
- Inadequacies in human capital and human resources management can lead to financial losses and a harmful social impact. Human mistakes, fraud, or other unethical activities are often the consequence of a lack of capacity to attract, manage, motivate, develop, and retain competent internal and external organizations.
- In every part of the firm, failures in internal business processes pose the potential of financial loss and a harmful social impact. Internal project failures and errors in product design are examples of this.
- Failures inside an organization’s internal systems pose a significant threat to financial and reputational well-being. Connectivity between branches, management information and core banking systems, information technology, and power backups are all included in this category.
- A financial loss or a decrease in social performance due to external circumstances out of an MFI’s control is “external events risk.” Natural calamities like storms and flooding and artificial events like war, robbery, arson, road blockades, and terrorist strikes fall under this umbrella.
RISK MATRIX
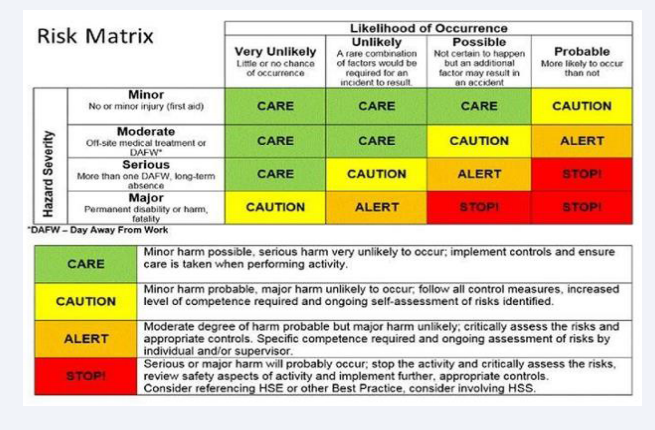
As part of assessing and rating the degree of risk, a Decision Matrix Risk Assessment (DMRA) technique, or risk matrix approach, is used to examine various risks and determine which threats should be addressed first to minimize the possibility of future problems. A person’s risk level is determined by the severity of the injury and the likelihood that it will occur. Even with little data and without specialized experience, it is straightforward to implement and visually appealing, and it is a speedy method for graphically assessing risks, the severity of hazards, and the frequency/probability of challenges. A popular decision-support tool in both the public and private sectors, the risk matrix is commonly employed in healthcare organizations because it standardizes risk grading. Stakeholders can see how these two factors contribute to total risk, which helps them to better understand and communicate about the hazards that have been discovered. As a result, a risk matrix helps determine the number of corrective actions/controls required in each department, unit, or facility, based on the score. To sum it up, using a risk matrix can be useful for evaluating and documenting changes in risk prior to and following the implementation of control measures (Figure 2).
Figure 2
CONCLUSION
Like every other sector, Covid-19 has also affected all the Healthcare industries. Covid-19 has changed the regular pattern and structure of all the health care units. Now more than usual, funds go to the health care sector by every government. NHS has also changed its strategy. NHS is trying new methods to manage its operations. This year has been challenging for the health care sector. NHS has managed their funds, and now they have created a separate unit for Covid Patients.
REFERENCES
- Gah MW. It-Enabled Healthcare Delivery: The U.K. National Health Service. 2013.
- Shah AS. National Healthcare Delivery Systems Influence Lung Transplant Outcomes for Cystic Fibrosis. 2008.
- Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021; 70(3): 537-543. doi: 10.1136/gutjnl-2020-322179. Epub 2020 Jul 20. PMID: 32690602.
- Faniyi AA, Lugg ST, Faustini SE, Webster C, Duffy JE, Hewison M, et al. Vitamin D status and seroconversion for COVID-19 in UK healthcare workers. Eur Respir J. 2021; 57(4): 2004234. doi: 10.1183/13993003.04234-2020. PMID: 33303541; PMCID: PMC7736751.
- Rind IA, Cannata A, McDonaugh B, Cassimon B, Bannister C, Scott PA, et al. Patients hospitalised with heart failure across different waves of the COVID-19 pandemic show consistent clinical characteristics and outcomes. Int J Cardiol. 2022; 350: 125-129. doi: 10.1016/j.ijcard.2021.12.042. Epub 2021 Dec 29. PMID: 34971665; PMCID: PMC8714242.
- Hoernke K, Djellouli N, Andrews L, Lewis-Jackson S, Manby L, Martin S, et al. Frontline healthcare workers' experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021; 11(1): e046199. doi: 10.1136/bmjopen-2020-046199. PMID: 33472794; PMCID: PMC7818840.
- England BR, Roul P, Yang Y, Kalil AC, Michaud K, Thiele GM, et al. Risk of COVID-19 in Rheumatoid Arthritis: A National Veterans Affairs Matched Cohort Study in At-Risk Individuals. Arthritis Rheumatol. 2021; 73(12): 2179-2188. doi: 10.1002/art.41800. Epub 2021 Oct 19. PMID: 33955209; PMCID: PMC8239709.
- French L, Hanna P, Huckle C. "If I die, they do not care": U.K. National Health Service staff experiences of betrayal-based moral injury during COVID-19. Psychol Trauma. 2022; 14(3): 516-521. doi: 10.1037/tra0001134. Epub 2021 Sep 13. PMID: 34516222.
- Mahendradhata Y, Andayani NLPE, Hasri ET, Arifi MD, Siahaan RGM, Solikha DA, et al. The Capacity of the Indonesian Healthcare System to Respond to COVID-19. Front Public Health. 2021; 9: 649819. doi: 10.3389/fpubh.2021.649819. PMID: 34307272; PMCID: PMC8292619.
- Fernandes G, Hassan I, Sridhar D. Building resilient health-care supply chains to manage pandemics in low- and middle-income countries. Bull World Health Organ. 2022 100(2): 174-176. doi: 10.2471/BLT.21.287177. Epub 2022 Jan 10. PMID: 35125544; PMCID: PMC8795856.
- Snowdon AW, Wright A. Supply chain capacity to respond to the COVID-19 pandemic in Ontario: Challenges faced by a health system in transition. Healthc Manage Forum. 2022; 35(2): 53-61. doi: 10.1177/08404704211057664. Epub 2022 Feb 7. PMID: 35129402; PMCID: PMC8832126.
- Joseph Finkenstadt D, Robert Handfield. Blurry vision: Supply chain visibility for personal protective equipment during COVID-19. 2021; 27(3): 100689.
- Vahidy F, Jones SL, Tano ME, Nicolas JC, Khan OA, Meeks JR, et al. Rapid Response to Drive COVID-19 Research in a Learning Health Care System: Rationale and Design of the Houston Methodist COVID-19 Surveillance and Outcomes Registry (CURATOR). JMIR Med Inform. 2021; 9(2): e26773. doi: 10.2196/26773. PMID: 33544692; PMCID: PMC7903978.
- Maness SB, Merrell L, Thompson EL, Griner SB, Kline N, Wheldon C. Social Determinants of Health and Health Disparities: COVID-19 Exposures and Mortality Among African American People in the United States. Public Health Rep. 2021; 136(1): 18-22. doi: 10.1177/0033354920969169. Epub 2020 Nov 11. PMID: 33176112; PMCID: PMC7856381.
- Turhan Z, Dilcen HY, Dolu ?. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr Psychol. 2022; 41(11): 8147-8156. doi: 10.1007/s12144-021-02105-8. Epub 2021 Jul 22. PMID: 34312580; PMCID: PMC8295547.
- Moon JR, Falick Ascher A. Post-COVID-19 Health Care System: A Call for Community-Based, Person-Centered, and Primary Care-Driven Care. Am J Public Health. 2021; 111(8): 1451-1455. doi: 10.2105/AJPH.2021.306160. PMID: 34464189; PMCID: PMC8489647.
- Wallenburg I, Helderman JK, Jeurissen P, Bal R. Unmasking a health care system: the Dutch policy response to the Covid-19 crisis. Health Econ Policy Law. 2022; 17(1): 27-36. doi: 10.1017/S1744133121000128. Epub 2021 Mar 5. PMID: 33663625; PMCID: PMC8007948.
- Anzaldua A, Halpern J. Can Clinical Empathy Survive? Distress, Burnout, and Malignant Duty in the Age of Covid-19. Hastings Cent Rep. 2021; 51(1): 22-27. doi: 10.1002/hast.1216. PMID: 33630324; PMCID: PMC8013970.
- Murata S, Rezeppa T, Thoma B, Marengo L, Krancevich K, Chiyka E, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021; 38(2): 233-246. doi: 10.1002/da.23120. Epub 2020 Dec 28. PMID: 33368805; PMCID: PMC7902409.
- Alderwick H, Dunn P, Gardner T, Mays N, Dixon J. Will a new NHS structure in England help recovery from the pandemic? BMJ. 2021; 372: n248. doi: 10.1136/bmj.n248. PMID: 33536236.
- Wise J. Covid-19: Is the UK heading towards mandatory vaccination of healthcare workers? BMJ. 2021; 373: n1056. doi: 10.1136/bmj.n1056. PMID: 33883193.
- Powell J. The rise of the green general practice. BMJ. 2021; 372: m4827. doi: 10.1136/bmj.m4827. PMID: 33531339.
- Yafi E. Impact of Green Training on Environmental Performance through Mediating Role of Competencies and Motivation. 2021; 13(10): 5624.
- Kotera Y, Rachel S, Michelle BU, Pauline G, Rebecca R. Teaching Healthcare Professional Students in Online Learning during COVID-19: Reflection of University. 2021; 3(3): 193-201.
- Reilly S, McCabe C, Marchevsky N, Green M, Davies L, Ives N, et al. Status of primary and secondary mental healthcare of people with severe mental illness: an epidemiological study from the UK PARTNERS2 programme. BJPsych Open. 2021; 7(2): e53. doi: 10.1192/bjo.2021.10. PMID: 33583478; PMCID: PMC8058911.
- Warner R, Hoinville L, Pottle E, Taylor C, Green J. Refocusing cancer multidisciplinary team meetings in the United Kingdom: comparing urology with other specialties. Ann R Coll Surg Engl. 2021; 103(1): 10-17. doi: 10.1308/rcsann.2020.0212. Epub 2020 Sep 28. PMID: 32981347; PMCID: PMC7705157.
- Chakraborty E. Developing Cleaning and Building Management Strategies for Green and Sustainable Healthcare Facilities 1st (Edn). 2021; 12.
- Benzidia S, Makaoui N, Bentahar O. The impact of big data analytics and artificial intelligence on green supply chain process integration and hospital environmental performance. 2021; 165.
- Simion VE. Green and Sustainable Public Procurement-An Instrument for Nudging Consumer Behavior. A Case Study on Romanian Green Public Agriculture across Different Sectors of Activity. 2021; 13(1): 12.
- Chiarini A, Opoku A, Vagnoni E. Public healthcare practices and criteria for a sustainable procurement: A comparative study between U.K. and Italy. Journal of Cleaner Production. 2017; 162: 391-399.
- Ahmadi A, Pishvaee MS, Torabi SA. Procurement Management in Healthcare Systems. Operations Research Applications in Health Care Management. 2017; 569-598.