CLEARVIEW: Comprehensive Law Enforcement Evaluation and Response Verification in Emergency Workplace
- 1. Department of Surgery, Georgetown University School of Medicine, USA
- 2. Georgetown University Law Center, USA
- 3. Department of Surgery, MedStar Washington Hospital Center, USA
- 4. Division of Traumatology, Surgical Critical Care and Emergency Surgery, University of Pennsylvania Perelman School of Medicine, USA
Abstract
Objectives: Unregulated policing in the Emergency Department (ED) may negatively impact patients, physicians, hospital employees, and law enforcement officers (LEO). Often it is the front line workers in the ED that are called upon to intervene in inappropriate police behavior, sometimes without proper policy guidance or education on effective intervention techniques. In order to understand current practices, tailor hospital policies and education, and track the outcomes of future interventions, an evidence-based tool is needed to rigorously observe employee and clinician intervention in inappropriate policing. Our goal was to develop this standardized tool (CLEARVIEW: Comprehensive Law Enforcement Evaluation and Response Verification in Emergency Workplace) to characterize and track current interactions between medical staff and LEO in the ED.
Methods: We used a two stage iterative process for tool development. First, trained observers recorded qualitative ED observations over a month. Second, observations were reviewed by the Georgetown Center for Innovation in Community Safety (a multidisciplinary team specializing in mitigating policing harm through bystander training) to define discrete identifiable intervention behaviors. During feasibility testing, observers were trained to identify and track these specific formalized intervention behaviors by medical staff using the newly developed CLEARVIEW tool at the Emergency Department (ED) of a high-volume academic Level 1 trauma center.
Results: A total of 1128 hours with 277 trauma patients presenting to the ED were observed. During the tool development period, 3% (12 of 398) of LEO-patient-hospital staff interactions were formal intervention behaviors. During feasibility testing, 7% (7 of 95) of LEO-patient-hospital staff interactions were formal intervention behaviors. The majority of interventions were performed by nurses, (63%, n=19), involved separating LEO from patients (53%, n=19) with only 21% stopping problematic LEO behavior.
Conclusions: Use of a newly developed observational tool to track formalized bystandership interventions between medical staff and LEO was feasible. These results before staff education designed to teach effective intervention techniques highlight the current lack of identifiable effective intervention techniques in this critical team interaction. This finding highlights the importance of developing formal intervention techniques for medical staff, development of shared policies between hospitals and LE agencies, and development and use of validated tools to optimize outcomes
Keywords
• Comprehensive Law Enforcement
• Evaluation
• Response Verification
• Emergency Workplace
• Emergency Department
Citation
Dowd J, Bowling P, Perez-Badillo M, Ramdath C, Mock L, et al. (2025) CLEARVIEW: Comprehensive Law Enforcement Evaluation and Response Verification in Emergency Workplace. Arch Emerg Med Crit Care 9(1): 1069.
INTRODUCTION
Law Enforcement Officer (LEO) presence in the emergency department (ED) is common. One reason unregulated LE activity in the ED may be problematic is the potential for competing priorities among care teams and LE. While both seek to enhance the greater good, clinicians are generally focused on the patient’s health, while LEO’s mission is typically centered on the investigation of a crime [1]. These competing priorities may put clinicians and law enforcement officers into conflict where clinicians feel obligated to intervene in LE behavior or have moral distress over LE behavior. There has been, to our knowledge, no systematic study to understand the frequency, character, and impact of these clinicians-LE interventions.
As there is more interest in improving these interactions, there is a need for a vetted tool to capture baseline information and ensure efficacy of efforts to optimize healthcare and law enforcement interactions in the ED. The purpose of this study was to develop the CLEARVIEW tool to observe and characterize clinician interactions with law enforcement and to demonstrate its feasibility of use in a large urban center. Law enforcement officers (LEO) come to the ED for a variety of reasons including accompanying patients in custody, investigation of crimes, and for other acts pursuant to their public safety duties. LEO presence within the ED has been shown to cause distress for patients, clinicians and LEO officers themselves [2]. Patients who are in contact with LEOs during their clinical care may experience retraumatization, decreased feelings of autonomy, and decreased trust in the healthcare team [3]. In addition, they may be at risk for violation of their civil rights.
Clinicians may experience erosion of patient-clinician relationships and moral distress navigating murky ethical waters in the absence of explicit education and policies. LEOs may feel distrusted and inefficient, and their investigations may be prolonged. While there are harms associated with each stakeholder, little has been done to understand how these stakeholders currently interact to regulate each other or how to mitigate these harms. Despite tensions, health care clinician and law enforcement officers have a number of important shared values including interest in public safety and cultures of safety. Within healthcare, improving the culture of safety has depended upon breaking down hierarchical structures and encouraging team members to speak up without fear of punishment when unsafe practices are witnessed [4]. The prime example of this is the enormous success seen with the institution of safety checklist which explicitly encourages a “see something say something” culture from all members of the healthcare team.
Law Enforcement agencies nationwide are beginning to embrace similar within team regulation, particularly with the introduction of a duty to intervene policies and active bystander intervention training. The Active Bystandership for Law Enforcement (ABLE), is a peer intervention program encouraging officers to intervene on their peers to prevent mistakes, misconduct and improve officer health and wellness. ABLE was developed by Georgetown Law’s Center for Innovations in Community Safety (CICS) to normalize peer intervention among police officers. ABLE has now been implemented in over 400 law enforcement agencies across the country.
The importance that both groups, clinicians and law enforcement, place on safety and the similar adoption of bystander intervention make the use of these techniques attractive for the mitigation of risks associated with law enforcement presence in the health care setting. To better understand the intricate interactions between clinicians and LEOs in the ED, the first step involves developing an objective tool to track intervention practices. Mitigating potential harms arising from the presence of law enforcement officers in hospitals requires the design and implementation of policies to optimize interactions...
Our long-term goal is to develop, implement, and assess bystander intervention training for clinicians seeking to reduce harm from LEO-patient interactions. In this study, we develop a standardized tool for characterizing clinician-LEO interactions in the ED and to assess its feasibility of use. We describe in this study the development and testing of CLEARVIEW: Comprehensive Law Enforcement Evaluation and Response Verification in Emergency Workplace tool, to allow for the collection of baseline data concerning LE interactions in the ED, track implementation and uptake of planned bystandership training, and allow for the comparison of interactions and implementation at multiple sites.
METHODS
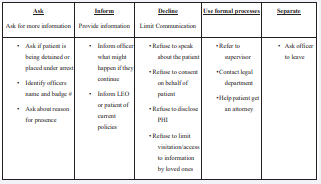
We developed CLEARVIEW using a two-stage iterative process at a large level 1 academic trauma center. During the first stage, the tool development period, trained observers conducted qualitative observations of LEO interactions to identify current interventional practices. The CLEARVIEW tool with five identifiable bystander intervention behaviors was then developed (Figure 1), rooted in ABLE principles and using qualitative observation data from this first stage. During the second stage, the tool feasibility period, observers were trained to identify specific formalized interventional practices as identified by our partners at CICS (Table 1a). To ensure understanding and consistency with scoring of behaviors, observers were trained prior to both stages using a week-long instructional interval in the trauma bay and an on-going database review for quality management throughout both stages. Following this weeklong training period, observers were alerted and observed all trauma activations.
Table 1: Summary of Observations and Intervention Outcomes Across Study Periods: This table presents the results of the two-stage observational study, which aimed to develop and assess the CLEARVIEW tool, an instrument designed to systematically observe and evaluate interactions between law enforcement officers (LEO) and clinicians/ hospital staff during trauma activations. The study was conducted in two phases: an initial development stage, where qualitative observations informed the tool's creation, and a subsequent feasibility stage, where trained observers applied the tool to assess formalized intervention behaviors
|
|
Stage I: Tool Development Period |
Stage II: Tool Feasibility Period |
|
Total Hours Observed: |
912 hours |
216 hours |
|
Total Trauma Patients Observed |
203 patients |
74 patients |
|
Number of Interactions |
398 interactions |
95 interactions |
|
- LEO-Patient |
168 interactions |
37 interactions |
|
- LEO-Clinician |
230 interactions |
58 interactions |
|
Number of Interventions |
12 interventions |
7 interventions |
Figure 1 Identifiable Intervention Behaviors Developed with Assistance from Georgetown.
Stage I: CLEARVIEW Development Period
During stage I, an observer trained in data collection in the ED employed a previously used observation tool, modified to track the number and type of LEO interventions. This pre-formed RedCAP survey collected time of patient and LEO arrival and departure, number of officers accompanying victim, type of officers, if victim was interviewed, when victim was interviewed, intervention strategy used, outcome of intervention, as well as occupation of individual who conducted the intervention. Most importantly, detailed qualitative summaries of interactions between LEO and hospital employees and victims were also logged in RedCap. Discrete interventional practices were extrapolated from these comprehensive interaction recordings.
Stage II: CLEARVIEW Feasibility Period
In the second stage, we used the qualitative observations between LEO and hospital employees to develop intervention prompts drawn on active bystander principles in order to build a RedCap observation tool. Interventions included various behaviors which hospital employees used to mitigate problematic LEO interactions and reduce tension overall. CICS’ expertise in the widespread implementation of ABLE training with LEO combined with the guidance of surgeons and hospital employees, resulted in five discrete behaviors that our observers were trained to identify and record during the observation period of stage II (Figure 2).
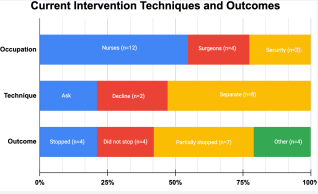
Figure 2 Current Intervention Techniques, Outcomes, and Occupation of Intervening Personnel: This chart illustrates the distribution of intervention techniques, their effectiveness in altering LEO behavior, and the occupational roles of individuals who intervened during observed trauma activations. Data were collected across both study periods, with interventions categorized by type and outcome.
RESULTS
In total, 1128 hours and 277 trauma patients were observed in the ED. There were 203 patients observed during the CLEARVIEW development period over 912 hours. During the CLEARVIEW feasibility period an additional 74 patients over the course of 216 hours were observed. In the CLEARVIEW development period, we recorded 398 interactions between LEO and patients, hospital staff and clinicians. Of these, 168 were between LEO and patients while 230 were between LEO and clinician or hospital staff. During this period, only 12 of these interactions employed formal intervention behaviors.
Nurses were responsible for nine of these interventions, surgeons two and hospital security one. We identified examples of interventions including two staff explaining policies, two staff refusing to provide information and eight asking the officer to leave. Most of these interactions either partially stopped (N=6) or completely stopped (N=3) the LEO behavior. Based on these observations and ABLE, we created the CLEARVIEW instrument to be tested for feasibility in the next period. During the subsequent CLEARVIEW feasibility period, we recorded 95 interactions between LEO and patients, hospital staff and clinicians. Interactions between LEO and patients accounted for 68 while an additional 27 were between LEO and clinicians or hospital staff.
Seven formalized interventions from the CLEARVIEW tools were identified during this period. Three interventions were conducted by nurses, two by surgeons and two by hospital security. Two of these interventions were characterized as informing, three as declining and two as separating. The result of these interventions included one which did not stop LEO behavior, one which partially stopped LEO behavior, one which completely stopped the behavior and four which resulted in an indeterminate outcome.
DISCUSSION
The objective of this study was to develop and evaluate a standardized observation tool, CLEARVIEW to record, characterize, and track effectiveness of clinicians and law enforcement interventions in the ED. We found that this tool was able to observe and track law enforcement behavior and staff interactions, and was able to be used in a typical real-world setting. We classified interactions between LEO and hospital employees in the ED using standard observations to shape CLEARVIEW development.
This is similar to previous tool development strategies that employ a step-wise iterative process to isolate and track specific behaviors [5]. In our study we isolated five classes of interventions that could be reliably recorded and categorized. Operationalizing behavioral patterns into discrete and recordable categories following a general observation period is a common study method across observation tool development in the medical and sociological settings [6]. We were able to use this method during our tool feasibility period and with the team’s expertise in active bystandership. The development of a standardized, replicable tool will enable us to look at differences in intervention practices following planned future crosstraining in a modified version of ABLE, one that applies active bystandership principles within the hospital setting.
This would include policies and training that aim to optimize clinician-LEO interactions, protect patient rights, and reduce tensions in the ER. Using the CLEARVIEW tool regularly will allow the collection and comparison of data before and after training interventions. This tool could be used not only at our hospital, but others across the country as well. The lack of clear policy, education and shared language in ED with regard to law enforcement presence has negatively impacted the wellness of hospital employees. Clinicians are impacted by LEO presence in the ED by the introduction of moral distress, as well as breaking down of the patient-clinician relationship [7]. Lack of knowledge of current policies by both employees and LEO creates conflict as members of the healthcare team experience confusion in navigating patient care responsibilities without knowing a clear right and wrong in their responsibilities to LEO investigation [8]. Sonnenberg et al., illustrated that clinicians have found it “exhausting identifying issues and have somebody beg for help, and you not knowing where to send them” when balancing the legal and clinical needs of patients with LEO present [9].
In another study only 12% of clinicians knew of local rules that kept LEO out of non-LEO areas of the hospital [10]. Clear guideline education and support may help to alleviate harms caused to clinicians in this situation but in order to enact these effectively, development of a shared language across treatment team, including law enforcement, is needed. Currently, hospital employees and LEOs do not share a common training or language about their interactions in this setting, which may lead to a lack of effective interventions. Staff are often unaware of when they can and should intervene, and how to effectively do so.
This is seen in our findings that interventions were infrequent and often unproductive. Future active bystandership training focusing on nursing and medical staff could empower hospital employees to intervene in the ED and promote cooperation between organizations. This training should also be offered to LEO, to give them an understanding of ED workflow to minimize risk of conflict. LEO are unable to effectively meet their professional responsibility without clear guidelines from the hospital and education of healthcare employees [11]. Without direction, for example, LEO inappropriately access hospital resources, including patient information and belongings, which can cause conflict with clinicians [8]. This miscommunication not only harms patients and clinicians but may also impair investigations and inhibit LEO efficiency. A pilot study demonstrates that LEOs desire clear direction within the ED in order to gather information that would help with their case without interfering with patient care [12].
There have been examples of officer misconduct and departments being sued due to lack of understanding of their rights and responsibilities in the hospital setting [13]. Evidence obtained in the ED through unconstitutional practices also may interfere with effective prosecution. A common set of training and language between LEO and hospital employees would create a team environment and allow LEO to best fulfill their professional obligations. Through this team interaction and prioritization on safety, LEO may approach interactions with a more traumainformed lens, centering care for victims of violence and, perhaps, increasing investigatory effectiveness.
Anchoring safety is a marker of a high reliability organization (HRO). Both healthcare and law enforcement seek to be HROs. A common tool of HROs include checklist culture and the embedded messages to encourage within team monitoring and accountability [4]. A result of this culture of safety in other HRO’s has been the development and implementation of safety protocols including those rooted in ABLE principles. Active bystandership opposes the harmful social phenomenon of the bystander effect by encouraging peer intervention and highlighting the benefits of speaking up to colleagues to prevent misbehavior and punishment [14].
As discussed previously, peer intervention already exists in the law enforcement space and has shown the potential to elevate the quality of policing by training partners to intervene on harmful behaviors [15]. In the past, officers may feel discouraged to speak up against partners or their department given the high stress, highly hierarchical system of policing. Interestingly, these conditions mirror hospitals where stress and power dynamics can prevent individuals from speaking up.
LIMITATIONS
During our study period observers were restricted by the ability to observe a limited number of interactions at once. Given that only an individual observer was present at any given time, interventions may have gone unrecorded if there was more than one LEO interaction occurring at the same time. Future studies should be conducted with multiple observers and additional methods of data collection including hospital surveillance footage or bodyworn-cameras. Additionally, qualitative analyses were limited by the observers’ definition of “intervention” and ability to classify a hospital employee’s intervention consistently into one of five discrete intervention categories (ask, inform, decline, use formal processes, separate). To mitigate this, observers were given examples of each intervention strategy in the context of the hospital to aid in classification and the development of observer training and categorization was an iterative process. The development of the CLEARVIEW tool was an attempt to address some of the limitations to allow for observation of interventions to occur across multiple settings.
CONCLUSION
The CLEARVIEW instrument has been an effective tool for us to observe and categorize healthcare and law enforcement interactions in the ED. The current shortage of effective intervention practices supports the idea that these practices are absent without training. The reframing of peer intervention and novel active bystandership training for the hospital setting could be a positive step towards effective protection of patients’ rights, improving clinician well being, and increasing LEO efficiency. One of the first steps to understanding this complex interplay is development of an objective assessment tool to record what intervention practices are currently done in the ED. We have demonstrated feasibility of use of such a tool as well as collected information on the dearth of effective interventions between clinicians and law enforcement officers in the ED.
REFERENCES
- Alur R, Hall E, Khatri E, Jacoby S, South E, Kaufman EJ. Law Enforcement in the Emergency Department. Jama Surg. 2022; 157: 852-854.
- Tahouni MR, Liscord E, Mowafi H. Managing Law Enforcement Presence in the Emergency Department. J Emerg Med. 2015; 49: 523- 529.
- Gallen KM, Smith MJ, Crane J, Loughran C, Schuster K, Sonnenberg J, et al. Law Enforcement and Patient Privacy Among Survivors of Violence. J Surg Res. 2023; 283: 648-657.
- Thomassen O, Espeland A, Softeland E, Lossius HM, Heltne JK, Brattebo G. Implementation of Checklists in Health Care; Learning from High-Reliability Organisations. Scand J Trauma Resusc Emerg Med. 2011; 3: 53.
- Leenstra NF, Jung OC, Cnossen F, Jaarsma ADC, Tulleken JE. Development and Evaluation of the Taxonomy of Trauma Leadership Skills–Shortened for Observation and Reflection in Training. Simul Healthc. 2020; 16: 37-45.
- Flowerdew L, Brown R, Vincent C, Woloshynowych M. Development and Validation of a Tool to Assess Emergency Physicians’ Nontechnical Skills. Ann Emerg Med. 2012; 59: 376-385.
- Metchik. Assessing Opportunities for Change and Collaboration Among Law Enforcement and Hospital-Based Violence Intervention Programs to Support Patient Rights in the Emergency Room.
- Gallen K, Sonnenberg J, Loughran C, Smith MJ, Sheppard M, Schuster K, et al. Health Effects of Policing in Hospitals. J Racial Ethn Health Disparities. 2023; 10: 870-882.
- Sonnenberg J, Metchick A, Hall E. Integration of Medical LegalServices into a Hospital-Based Violence Intervention Program. 2024.
- Moore PQ, Roy C, Aceves J, Palter JS. Interactions with Immigration Officers in the Emergency Department. Am J Emerg Med. 2020; 38: 1281-1283.
- Metchik. Assessing Opportunities for Change and Collaboration Among Law Enforcement and Hospital-Based Violence Intervention Programs to Support Patient Rights in the Emergency Room. 2014.
- Olsen DP, Brous E. The Ethical and Legal Implications of a Nurse’s Arrest in Utah. Am J Nurs. 2018; 118: 47-53.
- Wichmann D, Campos CEB, Ehrhardt CEB, Kock T, Weber C, Rohde H, et al. Efficacy of Introducing a Checklist to Reduce Central Venous Line Associated Bloodstream Infections in the ICU Caring for Adult Patients. BMC Infect Dis. 2018; 18: 267.
- Darley JM, Latane B. Bystander Intervention in Emergencies. J Personal Social Psychol. 1968; 8: 377-383.
- Lopez A. Active Bystandership for Law Enforcement (ABLE) Project Fact Sheet.