Comparison of Efficacy of Nebulized Ketamine with Intravenous Morphine in Patients with Multiple Trauma; A Randomized Double-Blinded Clinical Trial
- 1. Department of Emergency Medicine, Shahid Sadoughi University of Medical Sciences, Iran
- 2. Medical doctor, Shahid Sadoughi University of Medical Sciences, Iran
Abstract
Background & Aim: Pain management is a crucial aspect of care for trauma patients, as it significantly impacts both the patient and the treatment staff. Opioids are commonly used as analgesics for multiple trauma patients in the emergency department. However, due to their side effects, there is a need to explore alternative analgesic drugs that are safer yet equally effective. Therefore, this study aimed to compare the analgesic effects of ketamine nebulizer and intravenous morphine in trauma patients.
Materials and Methods: In this double-blind randomized controlled clinical trial, we divided multiple trauma patients referred to the emergency departments of Shahid Sadougi and Rahnamon Hospitals in Yazd province during 2020-2021 into two groups: nebulized ketamine and intravenous morphine. Pain intensity was assessed using the Visual Analogue Scale (VAS) at 30, 15, 10, 0, and 60 minutes. Additionally, we compared side effects, response rate, need for additional doses, pain relief, treatment failure, the Side Effects Rating Scale for Dissociative Anesthetics (SERSDA), and the onset of drug effect between the two groups. The data were analyzed using SPSS software.
Results: A total of 202 multiple trauma patients were included in the study, with one group receiving ketamine nebulizer and the other receiving intravenous morphine. There were no significant differences in pain intensity between the morphine and ketamine groups at all measured time points (p < 0.05). However, lightheadedness, hot flashes, and chest heaviness were significantly more common in the intravenous morphine group, while hallucinations, irritation of the nasal mucosa, and tremors were significantly more common in the nebulized ketamine group. The onset time of the drug effect was significantly shorter in the nebulized ketamine group compared to the intravenous morphine group (p = 0.030).
Conclusion: Nebulized ketamine can be considered a viable alternative to intravenous morphine in emergency trauma patients due to its comparable analgesic effect and faster onset without the complications associated with intravenous morphine.
Keywords
• Pain Management
• Multiple Trauma Patients
• Nebulized Ketamine
• Intravenous Morphine
Citation
Abarghouei SA, Jafari M, Zeinali F, Roknabadi ZR, Meidany A (2025) Comparison of Efficacy of Nebulized Ketamine with Intravenous Mor phine in Patients with Multiple Trauma; A Randomized Double-Blinded Clinical Trial. Arch Emerg Med Crit Care 9(2): 1071.
ABBREVIATIONS
SERSDA: Side Effects Rating Scale for Dissociative Anesthetics; VAS: Visual Analogue Scale.
INTRODUCTION
Trauma refers to sudden physical damage or injury to the body [1]. Currently, trauma is a leading cause of death worldwide, with approximately 5.8 million annual fatalities [2,3]. Moreover, trauma imposes a significant burden on medical costs and healthcare budgets [4-6]. Among the many complaints of trauma patients, pain is a common and distressing issue [7]. Effective pain management is crucial in the emergency department for the stabilization and care of these individuals [8]. Research indicates that pain relief should be initiated within 20 to 25 minutes of the trauma patient’s arrival in the emergency department to ensure prompt relief [9]. Unfortunately, trauma patients often express dissatisfaction with their pain management [10]. Inadequate pain control not only affects the patient’s well-being but may also increase the risk of chronic pain and post-traumatic stress disorder (PTSD) [11,12]. Enhancing pain management is not only a patient’s right but also contributes to early recovery, shorter hospital stays, cost reduction, prevention of chronic pain through neuroplasticity, and improved long-term outcomes [10,13 15]. However, there is no consensus yet on the optimal analgesic drug for pain relief in trauma patients [16,17]. Currently, morphine is the most commonly used analgesic in emergency rooms for trauma pain relief. It is FDA-approved for cases of moderate to severe pain. Morphine is a potent opioid that directly affects pain modulating receptors in the central nervous system (CNS) [18]. Although morphine offers advantages such as its analgesic effect and availability [19], it also carries significant side effects including dependence, tolerance, respiratory depression, activation of the emetic center, and hypotension. Therefore, safer alternatives should be considered for pain management in trauma patients [20,21]. Ketamine is another drug that has been investigated in various studies for pain reduction. It is used for general anesthesia and pain relief through N-Methyl D-Aspartate (NMDA) antagonism. Some studies have suggested ketamine as an alternative to morphine [8]. Inhaled ketamine has been shown to be safe, with no complications such as reflux, laryngospasm, cough, dry mouth, suffocation, dyspnea, tachycardia, aspiration, or oxygen desaturation during or after administration. Inhaled nebulized ketamine is also well-tolerated and easy to administer. It offers advantages such as lower drug dosage with adequate analgesic effect, rapid absorption into the systemic circulation, and the ability to administer in situations where an IV line is not yet established [22]. Studies have reported that intranasal ketamine provides analgesia within approximately 3 minutes, while oral ketamine takes 15 to 30 minutes, and insufflated ketamine takes 5 to 10 minutes [23-25]. However, higher doses of ketamine, regardless of the route of administration, may lead to complications such as nausea and vomiting, mild hypertension, hallucinations, tremors, and tonic seizures [26,27].While some studies suggest the analgesic effect of nebulized ketamine (inhalation) [9,28,29], and the superior long-term analgesic effect of combined nebulized ketamine and morphine compared to intravenous morphine [9], other studies indicate similar analgesic effects between nebulized ketamine and intravenous morphine [21]. Some studies even suggest that opioids may cause fewer side effects than ketamine [30]. Given the significance of pain management in trauma patients in the emergency department, the inconsistent results of previous studies, and the limited research comparing nebulized ketamine with intravenous morphine in trauma patients, we conducted a clinical trial. The study involved multiple trauma patients referred to the emergency departments of Shahid Sadoughi and Rahnamon hospitals in Yazd province from 2014 to 2016.
MATERIALS AND METHODS
Design & setting
This study was a double-blind randomized controlled clinical trial conducted on 202 trauma patients between 14 and 65 years of age at Shahid Sadoughi and Dr. Rahnamoun hospitals in 2020-2021. The study received ethical approval from the ethics committee of Shahid Sadougi University of Yazd (ethics code: IR.SSU.MEDICINE. REC.1399.023) and was registered in the Iranian registry of clinical trials (IRCT number: IRCT20200602047633N1). Prior to the research, the study objectives were explained to the patients, and written consent was obtained from those who wished to participate. For patients unable to provide written consent due to language barriers or writing difficulties, consent was obtained from their legal guardians. The authors strictly adhered to the principles outlined in the Declaration of Helsinki throughout the study.
Sample Size
The sample size was calculated to be 100 patients in each group using a formula for comparing proportions between the two groups. The calculation considered the assumption of noninferiority, a 95% confidence level, and 80% statistical power.
Inclusion and Exclusion Criteria: The study included patients aged 14 to 65 years with trauma-related pain and a pain score higher than 4. Exclusion criteria encompassed a Glasgow Coma Scale (GCS) score of 13 or less, recent analgesic use within the past 4 hours, lack of consent, history of seizures, use of psychedelics or drug addiction, inability to use a nebulizer mask in cases of maxillofacial trauma, systolic blood pressure outside the range of 90 180 mmHg, respiratory rate less than 10, pulse rate less than 60 or greater than 140, suspected brain hemorrhagic lesions or edema, pregnancy, allergy to study drugs, nausea and repeated vomiting, brain tumor, and glaucoma.
Procedure and Intervention
After obtaining informed consent from the patient or legal guardian and explaining the study procedure, patients underwent cardiac monitoring, pulse oximetry, peripheral vein puncture, and oxygen administration. Patients were randomly assigned to either Group A (case group) or Group B (control group) using a simple randomization method with a table of random numbers. In Group A, patients received nebulized ketamine (1 mg/kg, maximum 50 mg) diluted with 3 cc of distilled water, along with oxygen at a rate of 5 to 10 liters per minute. Additionally, 5 cc of intravenous distilled water was slowly injected into the peripheral vein. In Group B, patients received nebulized distilled water (3 cc) with oxygen at the same flow rate, and intravenous morphine (0.1 mg/kg, maximum 10 mg) diluted with 5 cc of distilled water was slowly injected into the peripheral vein.
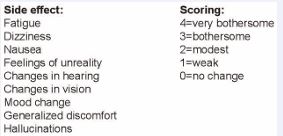
It is important to note that neither the patients nor the researchers were aware of the type of drug being administered. The data collection included demographics, pain scores based on the Visual Analog Scale (VAS), pulse rate, respiratory rate, blood pressure, side effects (hot flashes, lightheadedness, chest discomfort, nausea and vomiting, delusion, drowsiness, nasal mucus provocation, apnea, arrhythmia, tremor, and seizure), the Side Effects Rating Scale for Dissociative Anesthetics (SERSDA), excessive doses, and the type of injury (musculoskeletal injury, long bone fracture, vertebral injury, abdominal and pelvic or chest injury). These data were collected at 0, 10, 15, 30, and 60 minutes.If a patient requested analgesic, half of the previous dose was repeated up to two times. If the patient requested analgesic more than twice, the treatment was considered a failure, and a rescue drug (non-steroidal anti-inflammatory drugs (NSAIDs) or fentanyl) was prescribed based on the doctor’s judgment. Information and data related to these patients were also recorded. The Visual Analog Scale (VAS) was used to assess pain intensity. Patients indicated their pain intensity by marking a point on a 10 cm horizontal line, with the left end representing no pain and the right end representing the worst imaginable pain [9]. The Side Effects Rating Scale for Dissociative Anesthetics (SERSDA) was employed to evaluate the side effects of ketamine. This nine-component scale, although not validated, assessed the severity of each component on a scale from “0” (no side effects) to “4” (very bothersome). The components included fatigue, headaches, dizziness, feelings of unreality, generalized discomfort, changes in hearing, changes in mood, hallucinations, and changes in vision. SERSDA was chosen despite not being validated because it is commonly used in studies on ketamine side effects [31].
Statistical Analysis
The collected data were analyzed using SPSS (version 20; SPSS Inc., Chicago, Ill., USA). Qualitative data were presented as frequencies and percentages, while quantitative data were presented as means and standard deviations. Chi-Square Tests were used for the analysis of qualitative data, and an independent t-test was used to compare mean age, blood pressure, heart rate, and respiratory rate between the two groups. The Mann Whitney test was employed to compare the onset of drug effects in the two groups. A significance level of less than 0.05 was considered statistically significant.
Primary and Secondary Outcomes
The primary outcome of this study was defined as a two-point (20 mm) reduction in pain score based on the Visual Analog Scale (VAS). The secondary outcome was achieving pain relief to a score below four, determining the time of response to treatment in both groups, evaluating the complications of the studied drugs, determining the frequency of treatment failure in both groups, and determining the number of drug administrations.
RESULTS AND DISCUSSION
Results
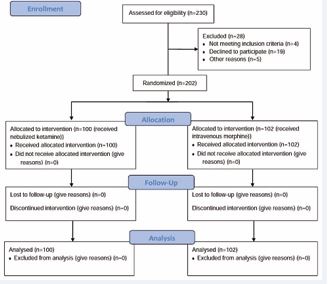
A total of 202 trauma patients were included in the study and divided into two groups: nebulized ketamine (n=100) and morphine (n=102). The average age of the patients was 38.17±13.7 years, with 110 patients (54.5%) being women and 92 patients (45.5%) being men. Both groups were similar in terms of age (p value=0.634), gender (p value=0.889), and type of trauma (p value>0.05), with no significant differences found (Table 1 and Figure 1).
Figure 1 CONSORT flowchart of study patients.
Table 1: Demographic variables of patients.
|
Variable |
nebulized Ketamine |
intravenous morphine |
P |
|
Gender (n (%)) * |
100(49.50) |
102(50.49) |
0.889 |
|
Female |
45(45) |
47(46.08) |
|
|
Male |
55(55) |
55(53.92) |
|
|
Age (mean±SD (years)) ** |
38.38±12.87 |
37.50±13.37 |
0.634 |
|
Type of injury * |
|
|
|
|
musculoskeletal injury |
24(24) |
31(30.5) |
0.308 |
|
long bone fracture |
42(42) |
31(30.4) |
0.086 |
|
vertebral injury |
19(19) |
22(21.6) |
0.650 |
|
abdominal injury |
3(3) |
8(7.8) |
0.129 |
|
pelvic injury |
20(20) |
17(16.7) |
0.540 |
|
chest injury |
18(18) |
11(10.8) |
0.144 |
* Chi-Square
** Independent t-test.
Pain intensity in the two groups was assessed before the intervention (p value=0.330), at 10 minutes (p value=0.058), 15 minutes (p value=0.289), 30 minutes (p value=0.790), and 60 minutes (p value=0.068). No significant differences were observed (Table 2).
Table 2: Pain score and hemodynamic variables studied in two groups at different times.
|
Variable |
nebulized Ketamine |
intravenous morphine |
P |
|
pain score (VAS) * |
|
|
|
|
Baseline |
8.15±0.89 |
8.12±0.95 |
0.330 |
|
after 10 minutes |
7.27±1.66 |
7.68±1.35 |
0.058 |
|
after 15 minutes |
6.25±1.91 |
6.25±1.67 |
0.289 |
|
after 30 minutes |
4.6±1.54 |
4.85±1.53 |
0.790 |
|
after 60 minutes |
3.7±1.18 |
3.7±1.02 |
0.068 |
|
Blood pressure(mmhg) * |
|
|
|
|
Baseline |
133±11 |
133±13 |
0.110 |
|
after 60 minutes |
129±8 |
129±9 |
0.617 |
|
pulse rateError! Bookmark not defined. |
|
|
|
|
Baseline |
94±11 |
91±10 |
0.001 |
|
after 60 minutes |
87±9 |
83±9 |
0.949 |
|
Respiratory rate * |
|
|
|
|
Baseline |
14±2 |
13±1 |
0.621 |
|
after 60 minutes |
12±1 |
14±1 |
0.990 |
|
The Onset of drug effects (mean±SD (Minutes)) * |
19.7±10.5 |
21.8±10.3 |
0.030 |
|
The additional dose (n (%)) |
61(61) |
65(63.7) |
0.569 |
VAS: visual analog scale
* Mann Whitney test.
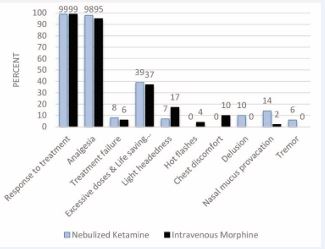
There were no statistically significant differences between the two groups (morphine and nebulized ketamine) in terms of treatment response rate (p value=0.989), achieving painlessness (p value=0.094), and treatment failure (p value=0.553) (Figure 2).
Figure 2 Side effects rating scale for dissociative anesthetics )SERSDA).
The incidence of lightheadedness (p value=0.034), flushing (p value=0.045), and chest discomfort (p value=0.001) was significantly higher in the group receiving intravenous morphine. Hallucinations (p value=0.001), nasal mucus provocation (p value=0.002), and tremor (p value=0.012), were significantly higher in the group receiving nebulized ketamine (Figure 3).
Figure 3 Comparison of some important variables of the two studied groups.
The onset time of ketamine’s effect was significantly shorter than that of morphine, as determined by the Mann-Whitney test (p value=0.030) (Table 2). Ten patients (10%) treated with ketamine experienced side effects according to the SERSDA criteria.In the analysis using the independent sample test, there were no significant differences in blood pressure (p value=0.617), respiratory rate (p value=0.949), and heart rate (p value=0.990) between the two groups 60 minutes after the intervention. Additionally, there was no significant difference in the need for an additional dose of the drug between the morphine and nebulized ketamine groups (p value=0.569) (Table 2).
Discussion
Pain management is crucial for trauma patients and should be initiated promptly. This study aimed to enhance and expedite pain control in trauma patients, ultimately improving their quality of life. Nebulization of analgesics in the emergency department offers a rapid, effective, and titratable delivery method while minimizing toxicity and side effects associated with intramuscular or intravenous injections. This approach optimizes the management of pain-related conditions in the emergency department. The study results strongly indicated that nebulized ketamine, similar to intravenous morphine, effectively controlled pain in multiple trauma patients, without the side effects commonly associated with morphine. Among the complications examined, hallucinations, nasal mucus provocation, and tremors were more frequently observed in the ketamine group, while vital signs remained unchanged in both groups. Consistent with our findings, a study by Azizkhani et al., in 2020 compared pain intensity in organ trauma patients receiving nebulized ketamine versus intravenous morphine. The study demonstrated the significant and comparable efficacy of both drugs in reducing pain intensity, with a higher incidence of nausea and vomiting in the morphine group and hallucinations in the ketamine group [21]. Another study by Lee et al., reported a higher risk of neurological side effects such as psychological events with ketamine and cardiopulmonary side effects with morphine. Overall, ketamine was deemed a safe drug with no side effects, although cautious use was recommended in patients with a history of mental health issues [32]. Heydari et al.’s study on trauma patients revealed that the combination of nebulized ketamine with morphine had effects similar to morphine alone, significantly reducing the need for additional morphine doses without increasing morphine-related complications [33]. A 2016 meta analysis by Lee et al. also supported low-dose ketamine as a key medication for pain management in the emergency department, potentially reducing opioid side effects [32]. In contrast to most studies showing similar analgesic effects between ketamine and morphine, Esfahani et al. found that ketamine’s analgesic effect was significantly higher than morphine across all time periods in a study involving 73 isolated limb injury patients [34]. Furthermore, Lee et al.’s study confirmed the hypothesis that ketamine’s effectiveness varies depending on the location of pain [32]. Similar to our study, Tran et al., reported a significantly lower rate of vomiting in the ketamine group compared to the morphine group. However, the ketamine group exhibited higher rates of hallucinations and irritability. Notably, ketamine administration did not have any adverse effects on the level of consciousness in patients with head trauma, suggesting its safety as an alternative to morphine in the emergency department [35]. In our study, nebulized ketamine showed a faster onset of action. In a 2015 study by Miller et al., the effects of intravenous ketamine and intravenous morphine were compared in patients with acute pain in the emergency department. Low-dose ketamine demonstrated similar effects to morphine but with a faster onset, aligning with the findings of our study [36]. Other studies comparing the effects of ketamine and morphine have also reported similar analgesic efficacy between the two, highlighting the absence of dangerous side effects associated with morphine use. For instance, Azizkhani et al., conducted a study in 2018 investigating the effectiveness of nebulized ketamine in combination with nebulized morphine and intravenous morphine in patients with long bone fractures. In contrast to our study, the onset of the analgesic effect was faster with intravenous morphine, but the combination of nebulized ketamine with nebulized morphine exhibited a longer duration of analgesia. Thus, the combination of ketamine with morphine enhances morphine’s effectiveness and reduces its side effects [9].
LIMITATIONS
One important limitation of this study was the short follow-up period for patients. The evaluation period was limited to 60 minutes. Therefore, future studies should assess the drug’s effectiveness over longer follow-up periods. Another limitation was the absence of a placebo group due to ethical considerations, making it impractical to follow patients without medical intervention. Future studies are recommended to explore alternative routes of drug administration (e.g., intramuscular and local) and different administration regimens (continuous and infusion) to further enhance pain management.
CONCLUSION
Based on the findings of this study, it was observed that nebulized ketamine, similar to intravenous morphine, exhibited effective analgesic properties in patients with multiple trauma. However, it demonstrated a faster onset of action compared to intravenous morphine, while avoiding side effects such as respiratory depression, apnea, nausea, and vomiting. Consequently, nebulized ketamine presents itself as a viable alternative to intravenous morphine for patients in the emergency department.
ACKNOWLEDGEMENTS
The authors appreciate the insightful cooperation of Medical Sciences and the staff of the Emergency Departments of Shahid Sadougi and Rahnamon Hospital, Yazd, Iran.
REFERENCES
- Dgu T. 20 years of trauma documentation in Germany-actual trends and developments. Injury. 2014; 45: S14-19.
- Gross CP, Anderson GF, Powe NR. The relation between funding by the National Institutes of Health and the burden of disease. N Engl J Med. 1999; 340: 1881-1887.
- Safari S, Radfar F, Baratloo A. Thoracic injury rule out criteria and NEXUS chest in predicting the risk of traumatic intra-thoracic injuries: A diagnostic accuracy study. Injury. 2018; 49: 959-962.
- Bastida JL, Aguilar PS, González BD. The economic costs of trafficaccidents in Spain. J Trauma Acute Care Surg. 2004; 56: 883-889.
- Van Beeck EF, van Roijen L, Mackenbach JP. Medical costs and economic production losses due to injuries in the Netherlands. J Trauma Acute Care Surg. 1997; 42: 1116-1123.
- Rahmati F, Doosti M, Bahreini M. The cost analysis of patients with traffic traumatic injuries presenting to emergency department; a cross-sectional study. Adv J Emerg Med. 2019; 3.
- Wenderoth BR, Kaneda ET, Amini A, Amini R, Patanwala AE. Morphine versus fentanyl for pain due to traumatic injury in the emergency department. J Trauma Nurs. 2013; 20: 10-15.
- Majidinejad S, Esmailian M, Emadi M. Comparison of intravenous ketamine with morphine in pain relief of long bones fractures: a double blind randomized clinical trial. Emergency. 2014; 2: 77.
- Azizkhani R, Akhbari K, Masoumi B, Parna A, Golshani K. Comparison of Efficacy of Nebulized Ketamine with Morphine and Intravenous Morphine in Pain Reduction in Patients with Traumatic Long-Bone Fractures Admitted to Emergency Department. Arch Trauma Res. 2018; 7: 114-120.
- Ahmadi A, Bazargan-Hejazi S, Zadie ZH, Euasobhon P, Ketumarn P, Karbasfrushan A, et al. Pain management in trauma: a review study. J Inj Violence Res. 2016; 8: 89.
- Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010; 11: 1859-1871.
- Siqveland J, Hussain A, Lindstrøm JC, Ruud T, Hauff E. Prevalence of posttraumatic stress disorder in persons with chronic pain: a meta- analysis. Front psychiatry. 2017; 8: 164.
- Gausche-Hill M, Brown KM, Oliver ZJ, Sasson C, Dayan PS, Eschmann NM, et al. An evidence-based guideline for prehospital analgesia in trauma. Prehospital Emerg Care. 2014; 18: 25-34.
- Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: Emerging concepts from the global war on terrorism. Crit Care Med. 2008; 36: S346-357.
- Masoumi B, Farzaneh B, Ahmadi O, Heidari F. Effect of intravenous morphine and ketorolac on pain control in long bones fractures. Adv Biomed Res. 2017; 6.
- Wakai A, O’Sullivan R, Staunton P, Walsh C, Hickey F, Plunkett PK. Development of key performance indicators for emergency departments in Ireland using an electronic modified-Delphi consensus approach. Eur J Emerg Med. 2013; 20: 109-114.
- Puntillo K, Neighbor M, O’Neil N, Nixon R. Accuracy of emergency nurses in assessment of patients’ pain. Pain Manag Nurs. 2003; 4: 171-175.
- Gupta A, Bodin L, Holmström B, Berggren L. A systematic review of the peripheral analgesic effects of intraarticular morphine. Anesth Analg. 2001; 93: 761-770.
- Mahshidfar B, Mofidi M, Fattahi M, Farsi D, Moghadam PH, Abbasi S, et al. Acute pain management in emergency department, low dose ketamine versus morphine, a randomized clinical trial. Anesthesiol pain Med. 2017; 7.
- Galinski M, Dolveck F, Combes X, Limoges V, Smaïl N, Pommier V, et al. Management of severe acute pain in emergency settings: ketamine reduces morphine consumption. Am J Emerg Med. 2007; 25: 385-390.
- Azizkhani R, Hassan S, Boroumand A, Rastin G, Ghasemi A, ShahbaziA. Analgesic Effects of Ketamine Nebulizer vs. Intravenous Morphine in Limb Trauma Patients in Pre-Hospital Emergency Setting; A Randomized Double-Blinded Clinical Trial. Front Emerg Med. 2020; 4: e84-e84.
- Jonkman K, Duma A, Velzen M, Dahan A. Ketamine inhalation. BJA Br J Anaesth. 2017; 118: 268-269.
- Hospital TU. Inhaled Nebulised S(+)-Ketamine for Postoperative Analgesia. 2018.
- Sinner B, Graf BM. Ketamine. In: Modern Anesthetics. Springer. 2008; 313-333.
- Quibell R, Prommer EE, Mihalyo M, Twycross R, Wilcock A. Ketamine. J Pain Symptom Manage. 2011; 41: 640-649.
- Klepstad P, Maurset A, Moberg ER, Øye I. Evidence of a role for NMDA receptors in pain perception. Eur J Pharmacol. 1990; 187: 513-518.
- SADOVE MAXS, SHULMAN M, HATANO S, FEVOLD N. Analgesiceffects of ketamine administered in subdissociative doses. Anesth Analg. 1971; 50: 452-457.
- Drapkin J, Masoudi A, Butt M, Hossain R, Likourezos A, Motov S. Administration of nebulized ketamine for managing acute pain in the emergency department: a case series. Clin Pract Cases Emerg Med. 2020; 4: 16.
- Dove D, Fassassi C, Davis A, Drapkin J, Butt M, Hossain R, et al. Comparison of Nebulized Ketamine at Three Different Dosing Regimens for Treating Painful Conditions in the Emergency Department: A Prospective, Randomized, Double-Blind Clinical Trial. Ann Emerg Med. 2021; 78: 779-787.
- Sobieraj DM, Martinez BK, Miao B, Cicero MX, Kamin RA, Hernandez AV, et al. Comparative Effectiveness of Analgesics to Reduce Acute Pain in the Prehospital Setting. Prehospital Emerg Care. 2020; 24: 163-174.
- Clattenburg EJ, Hailozian C, Haro D, Yoo T, Flores S, Louie D, et al. Slow Infusion of Low-dose Ketamine Reduces Bothersome Side Effects Compared to Intravenous Push: A Double-blind, Double- dummy, Randomized Controlled Trial. Acad Emerg Med. 2018; 25: 1048-1052.
- Lee EN, Lee JH. The effects of low-dose ketamine on acute pain in an emergency setting: A systematic review and meta-analysis. PLoS One. 2016; 11: 1-15.
- Heydari F, Azarian R, Masoumi B, Ghahnavieh AA. The effect of low dose ketamine on the need for morphine in patients with multiple trauma in emergency department. Eurasian J Emerg Med. 2020; 19: 219-226.
- Esfahani H, Khazaeipour Z, Safaie A, Aghili SM. Ketamine sub- dissociative dose vs. morphine sulfate for acute pain control inpatients with isolated limb injuries in the emergency department: a randomized, double-blind, clinical trial. Bull Emerg Trauma. 2021; 9: 73.
- Tran KP, Nguyen Q, Truong XN, Le V, Le VP, Mai N, et al. A comparison of ketamine and morphine analgesia in prehospital trauma care: acluster randomized clinical trial in rural Quang Tri province, Vietnam. Prehospital Emerg Care. 2014; 18: 257-264.
- Miller JP, Schauer SG, Ganem VJ, Bebarta VS. Low-dose ketamine vs morphine for acute pain in the ED: a randomized controlled trial. Am J Emerg Med. 2015; 33: 402-408.