Concussion Management in the Paediatric Emergency Department
- 1. Chelsea and Westminster Hospital NHS Foundation Trust, UK
- 2. Imperial College Healthcare NHS Trust, UK
Abstract
Objectives: The aim of this study was to evaluate the quality of advice given to patients and their carers in the PED with a diagnosis of concussion and the extent that correct practices were utilised. A secondary aim was to characterise concussion symptoms and duration in our study population.
Methods: Data were extracted from our hospital Electronic Patient Record (EPR) between 1/6/22 and 1/6/23 for patients 0-15 years with a discharge diagnosis of concussion.
Patients/carers were telephoned and invited to answer a questionnaire pertaining to discharge advice, management of concussion at home, symptom type and duration. A maximum of three attempts at making contact via telephone were made.
Results: 49 patients were identified with concussion. Sports were implicated in 25 (51%) with school the second most common medium (n=10, 20%). The most common symptoms were headache, nausea and dizziness which made up 72(64%).
When discharged 30 (61%) were given patient information leaflets and a further 5 (10%) were given verbal advice on rest and a graduated return to play. 14 (29%) were given incomplete or incorrect advice29 patients were contacted by telephone. The mean duration of symptoms was 27 days with a median of 14. 12 (41%) had symptoms for 7 days or less. 13/29 (48%) telephone respondents stated misleading or incorrect advice
Conclusion: While it is encouraging that concussion literature was given to the majority of patients on discharge, the recognition, discharge advice and patient support post discharge needs to be improved.
KEYWORDS
- Concussion; Paediatric emergency; Medical training; Patient support
CITATION
Stewart CG, Houbby N, Chawla J (2025) Concussion Management in the Paediatric Emergency Department. Arch Emerg Med Crit Care 9(1): 1066.
INTRODUCTION
Concussion is a complex injury for physician, patients and their carers to understand, interchangeably referred to as minor traumatic brain injury (mTBI) [1,2]. It is defined as ‘a traumatically induced transient disturbance of brain function’ however several other definitions exist as clinicians struggle to agree on how best to describe the condition [3-6]. The diagnosis of concussion, once moderate or severe brain injury has been ruled out, is challenging and relies on observed features, such as loss of consciousness, patient declared symptoms and examination findings all of which are entered into one of several algorithms to confirm or refute the diagnosis. There is no single blood test or radiological scan to make the diagnosis and uncertainty results in up to 50% of concussions going undiagnosed [7-9].
Head injuries pose a significant challenge to the paediatric population with subsequent concussions an unwanted complication [9]. It is thought that up to a third of children will sustain a head injury by the age of 13 [10], with an estimated 35,000 children presenting to hospitals in England annually, giving and estimated head injury incidence of 400/100,000 [11]. Consequently, concussion represents a large proportion of paediatric emergency department (PED) presentations with sports related events the leading cause [12].
The management of concussion is poorly understood by physicians, generally, and advice given to patients and their carers is often inconsistent and not aligned to current recommendations [13]. Return to play protocols require a period of rest, both physical and cognitive, with a graduated return to play based on reported symptoms. There are several concussion protocols originating from medical and sporting sources and the UK government has published a unifying document in 2023 [14].
The aim of this study was to evaluate the quality of advice given to patients and their carers in the PED with a diagnosis of concussion and the extent that correct practices were utilised. A secondary aim was to characterise concussion symptoms and duration in our study population
METHODS
Patients were identified from our hospital Electronic Patient Record (EPR) between 1/6/22 and 1/6/23 with a discharge diagnosis of concussion aged 0-15 years. Data were extracted for demographics, sex, race, mode of injury, place of injury, investigations and discharge advice.
Patients/carers were then telephoned and invited to answer a questionnaire pertaining to discharge advice, management of concussion at home, symptom type and duration. A maximum of three attempts at making contact via telephone were made. There were three different callers in this study to limit bias
Basic statistical methods were used to analyse data.
RESULTS
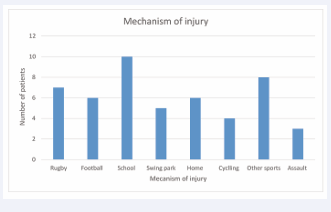
At total of 49 patients were diagnosed with concussion during the study period with 33 (67%) male and 16 (33%). Sports of all disciplines were implicated in 25 (51%) of concussions, however, school was the single most common medium for concussion (n=10, 20%) usually sustained during non-organised play either in the classroom or school yard (Figure 1).
Figure 1: Mechanism of Injury.
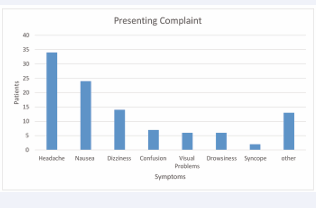
The majority of patients (n=29, 59%) presented 2 or more days after the initial head injury. The most common symptoms were headache, nausea and dizziness which made up 72(64%) of presenting features with many patients stating more than one (Figure 2).
Figure 2: Symptoms.
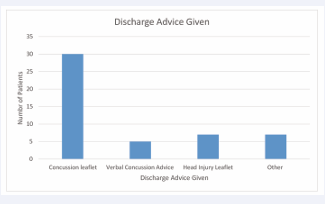
When discharged 30 (61%) were given patient information leaflets on concussion and a further 5 (10%) were given verbal advice on rest and a graduated return to play. 14 (29%) were given incomplete or incorrect advice (Figure 3).
Figure 3: Advice given to Patients.
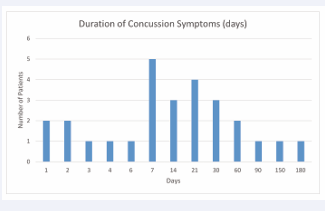
29 patients were successfully contacted by telephone. The mean duration of symptoms was 27 days with a median of 14. 12 (41%) of patients had symptoms for 7 days or less (Figure 4).
Figure 4: Duration of Concussion symptoms.
When asked to recall, 13/29 (48%) of respondents stated misleading or incorrect advice (Table 1).
Table 1: Discharge advice given to patients contradictory to standard concussion protocol
|
Patients |
Patients’ Account of Advice Given on Concussion |
|
1 |
Was given head injury leaflet, advised to stay off sports but was not given time frame for how long, told to limit screen time |
|
2 |
No sport and check for symptoms of concussion, with vomit and vision loss. |
|
3 |
Told to monitor daughter and was told it was a mild concussion, to remain off screens (couldn't remember how long), had a sports competition next week and was told could participate as long as she was feeling well |
|
4 |
Stay in a room with no light, no TV, mobile phone for 2 weeks. Stayed off school for 2 days. Hospital said when he returned to school, to go in for half days and this was done for about 1 weeks. Stayed off sports for 1 week - excluded from PE |
|
5 |
Told it was not concussion as he did not black out. Don't play rugby for 2 weeks and take paracetamol for headache. Take it easy |
|
6 |
Brain rest (no screens) for 1 week, attend headache clinic if concerns, if symptoms worsen or develops more serious symptoms such as vomiting to return |
|
7 |
Lie flat, stay away from physical activity - no specific time frame |
|
8 |
Not to play football or sports for a couple days, avoid screens as much as possible - no clearly defined period of time. Father felt he had to decide |
|
9 |
Provided with a leaflet, 1 month off sports, off screens 1 day |
|
10 |
Off physical education at school for 2 weeks, off school for 1 week, do not watch screens for 24 hours |
|
11 |
No rugby for a while, stay away from sports |
|
12 |
Stay at home, not to attend school for 2 weeks |
|
13 |
Not to look at screens |
DISCUSSION
Head injuries are common with an incidence of approximately 3.4% of all PED patients [15]. Our department receives a total of 42,000 patients per annum which would predict around 1400 children with head injury. Training in the diagnosis and management of head injury is important for PED staff including all potential outcomes such as concussion. The 49 patients with concussion in our cohort likely represents an underdiagnoses of the condition confirming findings in previous studies [7-9].
Children and young people are prone to concussion in sports [15], and this is reflected in our data with 51% of concussions occurring during sporting events. Anatomical differences, risk taking behaviour and skills acquisition all play a role in sustaining a head injury as a child. If we analyse play as a broader category including the school yard, home and play parks this accounts for 21/49 (43%) of concussions, the second biggest category. Children remain vulnerable in all situations [16]. The classic triage of headache, nausea and dizziness accounted for 64% of symptoms although it remains important to recognise the many physical, emotional, cognitive and mental health aspects of concussion symptomatology [17,18].
Regarding advice given to patients and their families on discharge, 35/49 (71%), of families received a patient information leaflet or documented verbal advice consistent with current concussion protocol. However, of the patients contacted by telephone, 13/29 (45%) recounted incorrect or contradictory advice. The subsequent median duration of symptoms was 7 days with a mean of 27 days which is broadly in keeping with current literature [19]. It is a concern, though, that symptom severity and duration may have been impacted by misinformation.
Results from our study indicate that physicians may lack a basic understanding of concussion management even when supplying patients with written information. Parents and carers should not be expected to verify advice. In a large cosmopolitan city less than fluent English language proficiency in immigrant groups adds to the challenge of understanding patient information literature.
While it is encouraging that literature on the management of concussion was given to the majority of patients, the recognition, discharge advice and patient support post discharge could to be improved.
Regular repeated teaching is required to tackle this gap in training amongst the PED team. Post discharge patient support must be developed to ensure adherence to protocols at home via the general practitioner service by the creation of a concussion clinic in PED. Such a hub in support of families, health professionals, schools and sports communities would be a boost in the management of concussion.
LIMITATIONS
While this study is small it is encouraging that results for symptom duration and the prevalence of sports concussion agree with current literature. As a retrospective study we were reliant on documentation for data extraction which is sometimes incomplete. Also the telephone respondents may not have remembered details of their children’s presentations accurately up to a year post injury. There is always the potential for bias with human contact and while utilising three callers for the telephone survey will hopefully have limited this, the potential for bias remains.
CONTRIBUTORSHIP
Dr Stewart designed the study, gathered data, co-wrote and edited the submission
Dr Houbby gathered data and co-wrote the submission
Dr Chawla gathered data and co-wrote the submission
ETHICS
This service evaluation was registered locally in keeping with the General Medical Council’s Good Practice in Clinical Governance Guidelines. The project was undertaken in accordance with the Trust Research and Development guidelines; ethics approval was not required by the hospital trust Research and Ethics Committee which approved the study.
REFERENCES
- Sussman ES, Pendharkar AV, Ho AL, Ghajar J. Mild traumatic brain injury and concussion: terminology and classification. Handb Clin Neurol. 2018; 158: 21-24.
- Rivera RG, Roberson SP, Whelan M, Rohan A. Concussion evaluation and management in pediatrics. MCN Am J Matern Child Nurs. 2015; 40: 76-86.
- Menon DK, Schwab K, Wright DW, Maas AI. Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010; 91: 1637- 1640.
- Patricios JS, Schneider KJ, Dvorak J, Ahmed OH, Blauwet C, Cantu RC, et al. Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport-Amsterdam, October 2022. Br J Sports Med. 2023; 57: 695-711.
- Iverson GL, Lange RT, Waljas M, Liimatainen S, Dastidar P, Hartikainen KM, et al. Outcome from complicated versus uncomplicated mild traumatic brain injury’. Rehabil Res Pract. 2012; 1-7.
- Decq P, Brauge D, Calmat A, Cassodesalle H, Dehail P, Deroche F, et al. Diagnosis clinical criteria of sport related concussion: Toward an operational criteria definition in France. Neurochirurgie. 2021; 67: 222-230.
- Echemendia RJ, Meeuwisse W, McCrory P, Davis GA, Putukian M, Leddy J, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. Br J Sports Med. 2017; 51: 848- 850.
- Pfister T, Pfister K, Hagel B, Ghali WA, Ronksley PE. The incidence of concussion in youth sports: a systematic review and meta-analysis. Br J Sports Med. 2016; 50: 292-297.
- Hux K, Dymacek R, Childers C. ‘Possible brain injury events and symptoms in elementary school children’. Brain Inj. 2013; 27: 1348- 1355.
- Trefan L, Houston R, Pearson G, Edwards R, Hyde P, Maconochie I, et al. Epidemiology of children with head injury: a national overview. Arch Dis Childhood. 2016; 101: 527-532
- Yaramothu C, Goodman AM, Alvarez TL. Epidemiology and incidence of pediatric concussions in general aspects of life’. Brain Sci. 2019; 9: 257.
- Haroon Rashid, Smarak Mishra, Nick Dobbin. Management of sport- related concussion in emergency departments in England: a multi- center study, Brain Inj. 2021; 35: 1035-1042.
- Department for Culture, Media and Sport. UK Concussion Guidelines for Non-Elite (Grassroots) Sport. 2023.
- Ramsay S, Dahinten S. Concussion Education in Children and Youth: A Scoping Review. SAGE Open Nurs. 2023; 6: 2377960820938498.
- Kirkwood G, Parekh N, Ofori-Asenso R, Pollock AM. Concussion in youth rugby union and rugby league: a systematic review. Br J Sports Med. 2015; 49: 506-510.
- Haas R, Zayat M, Sevrin A. Current Concepts in the Evaluation of the Pediatric Patient with Concussion. Curr Rev Musculoskelet Med. 2019; 12: 340-345.
- Gornall A, Takagi M, Morawakage T, Liu X, Anderson V. Mental health after paediatric concussion: a systematic review and meta-analysis. Br J Sports Med. 2021; 55: 1048-1058
- Manzanero S, Elkington LJ, Praet SF, Lovell G, Waddington G, Hughes DC. Post-concussion recovery in children and adolescents: A narrative review. J Concussion. 2017; 1.
- Schilling S, Mansour A, Sullivan L, Ding K, Pommering T, Yang J. Symptom Burden and Profiles in Concussed Children with and without Prolonged Recovery. Int J Environ Res Public Health. 2020; 17: 351.