Pancytopenia Unveiling a Silent Pituitary Crisis: A Rare Presentation of Sheehan’s Syndrome
- 1. Coimbatore Medical College Hospital, India
- 2. PSG Hospitals, India
- 3. Tamil Nadu Dr. M.G.R. Medical University, India
Abstract
Sheehan’s syndrome is a type of postpartum hypopituitarism that results from ischemic pituitary necrosis caused by severe obstetric haemorrhage. Pancytopenia generally raises suspicion for hematologic malignancies or marrow failure syndromes rather than endocrine disorders.
However, it is essential to recognize that endocrine pathologies, especially panhypopituitarism, can also lead to pancytopenia due to the complex interplay of multiple hormonal deficiencies leading to bone marrow suppression. Awareness of this rare presentation can help prevent delays in diagnosis and management. Here we report a woman in her late 30’s, fourteen years postpartum, with giddiness, shortness of breath and chronic fatigue who presented in the ER with hypotension and routine blood investigations revealed pancytopenia. On further probing, her obstetric history revealed postpartum haemorrhage and lactation failure over a decade ago and led to the long workup for Sheehan’s. Hormone replacement with glucocorticoids and levothyroxine led to clinical stabilization and gradual reversal of pancytopenia.
Keywords
• Pancytopenia
• Sheehan’s syndrome
• Pituitary Crisis
• Obstetric haemorrhage
Citation
Manikandan K, Saravanan NKS, Senthilkumar V (2025) Pancytopenia Unveiling a Silent Pituitary Crisis: A Rare Presentation of Sheehan’s Syndrome. Arch Emerg Med Crit Care 9(1): 1070.
INTRODUCTION
While classic presentations include lactation failure, amenorrhea, and features of adrenal or thyroid hormone deficiency, the condition often remains undiagnosed for years, especially when symptoms are subtle or attributed to other causes. Hematologic abnormalities, though uncommon, may serve as critical diagnostic clues. Pancytopenia is particularly rare in Sheehan’s syndrome and is more commonly associated with hematological malignancies or marrow failure syndromes. The possibility of hypopituitarism is often overlooked in such cases, delaying diagnosis and treatment. Increased clinical awareness of this association is essential, as hormone replacement therapy can reverse the hematologic abnormalities, underscoring the importance of timely recognition. This case aims to highlight a rare but reversible manifestation of panhypopituitarism and reinforces the need for clinicians to consider endocrine causes in patients with unexplained pancytopenia and subtle postpartum history.
CASE PRESENTATION
A woman in her late 30s presented to the emergency department with complaints of giddiness, extreme fatigue, and breathlessness on exertion for two weeks. She was hypotensive on arrival, with a blood pressure of 70/50 mmHg and a mean arterial pressure of 56.7 mmHg. On general examination, patient was drowsy, but oriented to place, person, and time. She had facial puffiness, pallor over palpebral conjunctiva, loss of hair in the lateral aspect of eyebrows, loss of axillary and pubic hair, dry and coarse skin. On neurological examination, a slow hung-up knee jerk reflex was observed. A review of other systems was normal with no murmurs or added sounds.
Electrocardiogram showed low voltage QRS complexes, and echocardiography reported trivial tricuspid regurgitation with preserved left ventricular function.
On ultrasound of the abdomen, the IVC diameter was 1.9cm with greater than 50% collapsibility during inspiration, showing a hypovolemic status. She was started on iv crystalloids and inotropes. Furthermore, her blood pressure kept falling during the hospital stay, almost questioning the pathophysiology behind the refractory hypotension despite treatment protocols.
On further history taking, the menstrual history indicated amenorrhea for the past five years. Her obstetric history indicated massive blood loss following her last vaginal delivery a decade ago, for which she was admitted in the intensive care unit and given subsequent blood transfusions. She was also unable to breastfeed her child during her immediate postpartum, confirming lactation failure.
Routine blood investigations, along with thyroid profile were ordered. The possibility of Sheehan’s was considered, and a MRI-Brain was ordered.
INVESTIGATIONS
Initial laboratory evaluation revealed pancytopenia: haemoglobin of 5.9 g/dL, white blood cell count of 3.5 × 10³/ µL, and platelet count of 96 × 10³/µL. Mean corpuscular volume was slightly elevated at 99.5 fL and peripheral smear showed dimorphic anemia with thrombocytopenia. Electrolytes were within normal limits, though potassium was slightly low at 3.4 mmol/L.
Thyroid function testing revealed low triiodothyronine(T3) and thyroxine(T4) with a normal thyroid-stimulating hormone (2.73 µIU/mL), suggestive of central hypothyroidism.
A complete endocrine panel of investigations was conducted. Serum cortisol was markedly reduced at 2.0 µg/dL confirming adrenal insufficiency. Levels of anterior pituitary hormones were also suppressed: growth hormone (0.4 ng/mL), luteinizing hormone (6.77 mIU/ mL), and follicle-stimulating hormone (5.76 mIU/mL), all below expected post-menopausal levels. All the laboratory investigations are shown in Figure 1.
Figure 1: Table showing all the Laboratory investigations
|
Investigations |
Values |
Reference range |
|
Complete Blood Count |
||
|
Hb (g/dL) |
5.9 |
12-15 |
|
MCV (fl) |
99.5 |
80-100 |
|
Hct (%) |
21.8 |
36-48 |
|
WBC count (/µL) |
3.5x 103 |
(4-10) × 103 |
|
Platelet count (/µL) |
96x 103 |
(150-400) × 103 |
|
Serum laboratory tests |
||
|
Na+ (mmol/L) |
144 |
136-144 |
|
K+ (mmol/L) |
3.4 |
3.6-5.1 |
|
GH (ng/ml) |
0.4 |
0.5- 10 |
|
TSH (µIU/mL) |
2.73 |
0.27-4.2 |
|
T3 (ng/dL) |
46.75 |
80-200 |
|
T4 (µg/dL) |
3.62 |
5.1-14.1 |
|
Cortisol (µg/dL) |
2.0 |
4.8-19.5 (morning- fasting) |
|
LH (mIU/mL) |
6.77 |
7.7-58.5 (post-menopausal) |
|
FSH (mIU/mL) |
5.76 |
25.8-134.8 (post-menopausal) |
|
Others |
||
|
RBS (mg/dL) |
86 |
70-140 |
Magnetic resonance imaging of the brain demonstrated a cerebrospinal fluid-filled sella turcica with absent visualization of the pituitary gland, consistent with empty sella syndrome, as shown in Figure 2, confirming the diagnosis of Sheehan’s syndrome in our patient.
Figure 2: T2-weighted MRI Brain (Sagittal section), arrow pointing to “Empty Sella” with absent Pituitary gland
TREATMENT
Initial management focused on stabilizing the patient’s hemodynamic status with intravenous crystalloids and inotropic support, given the persistent hypotension. Despite these measures, her blood pressure remained low, prompting consideration of endocrine causes. Once adrenal insufficiency was confirmed, she was promptly started on intravenous hydrocortisone 100 mg every 12 hours, which led to a gradual improvement in blood pressure.
Following confirmation of central hypothyroidism, oral levothyroxine was initiated at a dose of 100 micrograms once daily. After clinical stabilization, intravenous hydrocortisone was transitioned to oral prednisolone. No hematinics or bone marrow stimulants were used, as the pancytopenia was attributed to panhypopituitarism.
The combination of corticosteroid and thyroid hormone replacement led to significant clinical improvement, including normalization of blood pressure and progressive resolution of pancytopenia over several weeks of follow-up.
OUTCOME AND FOLLOW-UP
The patient showed marked clinical improvement following initiation of hormone replacement therapy. Within days of corticosteroid initiation, her blood pressure stabilized, and symptoms such as fatigue, drowsiness, and giddiness improved significantly. Oral thyroid hormone was well tolerated, and her energy levels gradually returned to baseline.
Serial complete blood counts over the following weeks showed a progressive increase in haemoglobin, white blood cell count, and platelet count, indicating full reversal of pancytopenia. At her six-week follow-up, she remained clinically stable, with normal hematologic parameters and improved quality of life. She resumed household activities and reported better physical stamina and mood.
Long-term endocrine follow-up was arranged through the endocrinology clinic for continued monitoring and dose adjustments. She was educated on the need for lifelong hormone replacement and stress-dose steroid coverage during illness or surgery. Surveillance for other potential pituitary axis deficiencies is ongoing.
DISCUSSION
The gradual reversal of the pancytopenia in this patient after hormone replacement therapy strongly proves the positive association between Panhypopituitarism and its resulting Pancytopenia.
While classical symptoms such as amenorrhea and lactation failure are well described in our case, this case highlights a rare and underrecognized manifestation— pancytopenia. Anaemia is the most commonly documented haematological abnormality in Sheehan’s syndrome [1]. Pancytopenia, however, is a rare hematologic abnormality and has been reported in only a few published case reports worldwide [2]. Since pancytopenia is extremely uncommon and can easily be misattributed to hematologic or infectious causes, this can cause a significant delay in the diagnosis.
The extent of pituitary dysfunction varies from patient to patient. Patients can present with a combination of central hypothyroidism, hypogonadotropic hypogonadism and adrenal insufficiency, each presenting in varied extents clinically [3].
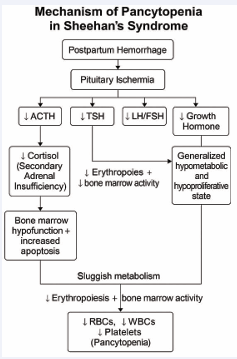
The pathophysiology involves multiple anterior pituitary hormone deficiencies that impair haematopoiesis. Cortisol deficiency reduces erythropoietin responsiveness and impairs leukocyte and platelet production. Thyroid hormone deficiency reduces metabolic demand and erythropoiesis, and growth hormone deficiency limits hematopoietic progenitor cell proliferation via reduced insulin-like growth factor 1 (IGF-1) activity [4].
Collectively, these deficits can lead to a functional bone marrow suppression. Figure 3 depicts a flowchart explaining the mechanism discussed.
Figure 3: Flowchart showing the Mechanism of Pancytopenia
The diagnosis of hypopituitarism may be delayed, especially if symptoms emerge insidiously years after delivery. In this case, recognition of the patient’s obstetric history and subtle physical signs such as eyebrow thinning and dry skin prompted endocrine evaluation. The detection of low pituitary hormones and MRI evidence of an empty sella led to the final diagnosis.
Importantly, this case reinforces that hormone replacement alone—with corticosteroids and levothyroxine—can reverse pancytopenia without the need for bone marrow biopsy or hematopoietic agents. Clinicians should be vigilant for endocrine causes of pancytopenia, especially when other signs of hypopituitarism are present.
A review of published cases reveals only a few reports of similar presentations, all of which responded to hormone therapy [5,6]. This case adds to the growing body of evidence that panhypopituitarism must be considered in unexplained pancytopenia, especially in females with a suggestive obstetric history.
LEARNING POINTS
· Persistent hypotension and pancytopenia in a middle-aged woman with a history of postpartum haemorrhage should prompt evaluation for hypopituitarism.
· Sheehan’s syndrome, though classically associated with amenorrhea and lactation failure, can present decades later with subtle and systemic signs, including pancytopenia.
· Hormonal deficiencies, particularly cortisol and thyroid hormone, can lead to reversible bone marrow suppression; timely endocrine evaluation can prevent unnecessary invasive work-up.
· Hormone replacement therapy with glucocorticoids and levothyroxine can lead to full hematologic recovery of pancytopenia, reinforcing the critical role of pituitary hormones in haematopoiesis.
REFERENCES
- Fatma M, Mouna E, Nabila R, Mouna M, Nadia C, Mohamed A. Sheehan’s syndrome with pancytopenia: a case report and review of the literature. J Med Case Rep. 2011; 5: 1-3.
- Rabee’ H, Tanbour R, Yaseen A, Zaidan M, Amer R. Case report: Pancytopenia as a rare presentation of Sheehan’s syndrome. SAGE Open Med Case Rep. 2022; 10: 2050313X221109431.
- Elfaleh E, Oueslati I, Chihaoui M, Yazidi M, Chaker F, Rejeb O, Slimane H. Sheehan. InEndocrine Abstracts 2018 May 8 (Vol. 56). Bioscientifica.
- Christ ER, Cummings MH, Westwood NB, Sawyer BM, Pearson TC, Sonksen PH, et al. The importance of growth hormone in the regulation of erythropoiesis, red cell mass, and plasma volume in adults with growth hormone deficiency. J Clin Endocrinol Metab. 1997; 82: 2985-2990.
- Kim DY, Kim JH, Park YJ, Jung KH, Chung HS, Shin S, et al. Case of complete recovery of pancytopenia after treatment of hypopituitarism. Annals of hematology. 2004; 83: 309-312.
- Laway BA, Bhat JR, Mir SA, Khan RS, Lone MI, Zargar AH. Sheehan’s syndrome with pancytopenia—complete recovery after hormone replacement (case series with review). Ann Hematol. 2010; 89: 305-308.